Abstract
Summary of background data
We reported that excessive disc space distraction caused by insertion of large cages during posterior lumbar interbody fusion (PLIF) combined with pedicle screws (PS) induces adjacent segment disease (ASD). Spinous process plate (SPP) is known to allow cage subsidence when used in PLIF, since they cannot share vertical loads. We therefore hypothesize that the incidence of ASD after PLIF with SPP should be lower than that after PLIF with PS due to this loss of disc space distraction.
Materials and methods
Radiographic ASD is defined as development of spondylolisthesis >3 mm, decrease in disc height >3 mm, or intervertebral angle at flexion lesser than −5°. Symptomatic ASD is defined by a decrease of ≥4 points in Japanese Orthopedic Association score. One hundred and thirty patients with L4 spondylolisthesis were treated with either PLIF with SPP (n = 45) or PLIF with PS (n = 85) and followed up for a minimum of 2 years (mean, 39.0 months).
Results
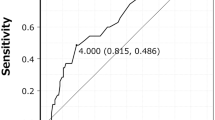
L4–5 disc space distraction in the SPP group was significantly smaller (0.4 mm) as compared to the PS group (1.8 mm). The incidence of clinical ASD in the SPP group (2%, 1/45) was also significantly less than that in the PS group (15%, 13/85). Multivariate analysis showed that disc space distraction was the most significant risk factor.
Conclusions
Among various risk factors for ASD after PLIF, the excessive distraction of disc space proved to be a potent risk factor for ASD.






Similar content being viewed by others
References
Cheh G, Bridwell KH, Lenke LG et al (2007) Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation. Spine 32:2253–2257
Fuji T, Namekata M, Kaito T et al (2007) Posterior lumbar interbody fusion using BAK cage and the lumbar alligator spinal system for degenerative spondylolisthesis of the lumbar spine. Clin Orthop Surg 42(3):243–247 (Jpn)
Kumar MN, Jacquot F, Hall H (2001) Long term follow-up functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J 10:309–313
Rohlmann A, Burra NK, Zander T, Bergmann G (2007) Comparison of the effects of bilateral posterior dynamic and rigid fixation devices on the loads in the lumbar spine: a finite element analysis. Eur Spine J 16:1223–1231
Sudo H, Oda I, Abumi K et al (2006) Biomechanical study on the effect of five different lumbar reconstruction techniques on adjacent–level intradiscal pressure and lamina strain. J Neurosurg Spine 5:150–155
Aota Y, Kumano K, Hirabayashi S (1995) Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Diord 8:464–473
Cheh G, Bridwell KH, Lenke LG et al (2007) Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation. Spine 32:2253–2257
Etebar S, Cahill DW (1999) Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg 90:163–169
Nakai S, Yoshizawa H, Kobayashi S (1999) Long-term follow-up study of posterior lumbar interbody fusion. J Spinal Disord 12:293–299
Okuda S, Oda T, Miyauchi A et al (2008) Lamina horizontalizaiton and facet tropism as the risk factors for adjacent segment degeneration after PLIF. Spine 33(25):2754–2758
Okuda S, Iwasaki M, Miyauchi A et al (2004) Risk factors for adjacent segment degeneration after PLIF. Spine 29(14):1535–1540
Kaito T, Hosono N, Mukai Y et al (2010) Excessive distraction of lumbar disc space inducesearly degeneration of the adjacent segment after posterior lumbar interbody fusion (PLIF). J Neurosurg Spine 12:671–679
Leong YCJ, Chun SY, Grange WJ et al (1983) Long-term results of lumbar intervertebral disc prolapsed. Spine 8:797–799
Van Horn JR, Bohnen LMLJ (1992) The development of discopathy in lumbar discs adjacent to a lumbar anterior interbody spondylodesis. A retrospective matched-pair study with a postoperative follow-up of 16 years. Acta Orthop Belg 58:280–286
Cheung KMC, Zhang YG, Lu DS et al (2003) Reduction of disc space distraction after anterior lumbar interbody fusion with autologous iliac crest graft. Spine 32:1385–1389
Dennis S, Watkns R, Landaker S et al (1989) Comparison of disc space heights after anterior lumbar interbody fusion. Spine 14:876–878
Kawamura M, Hosono N, Ohwada T et al (2007) Postoperative alignment change and cage subsidence after posterior lumbar interbody fusion with threaded cages and a spinous process plate. Clin Orthop Surg 42(1):63–67 (Jpn)
Brantigan JW, Steffee AD (1993) A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical result in the first 26 patients. Spine 18:2106–2107
Izumida S, Inoue S (1986) The criteria for evaluation of the results of operation for low back pain by the Japanese orthopaedic association. J Jpn Orthop Assoc 60:391–394 (Jpn)
Ha KY, Shin JH, Kim KW et al (2007) The fate of anterior autogenous bone graft after anterior radical surgery with or without posterior instrumentation in the treatment of pyogenic lumbar spondylodiscitis. Spine 2:1856–1864
Nagaosa Y, Kikuchi S, Hasue M (1998) Pathoanatomic mechanisms of degenerative spondylolisthesis : a radiographic study. Spine 23:1447–1451
Vannaranta H, Floyd T, Ohnmeiss DD et al (1993) The relationship of facet tropism to degenerative disc disease. Spine 18:1000–1005
Wiltse LL, Radecki SE, Biel HM et al (1999) Comparative study of the incidence and severity of degenerative change in the transition zones after instrumented versus noninstrumented fusions of the lumbar spine. J Spinal Disord 12:27–33
Ohkohchi T, Ohwada T, Yamamoto T (2000) Long-term results of posterior lumbar interbody fusion for lumbar degenerative disorders. Clin Orthop Surg 35(5):519–526 (Jpn)
Nagata H, Schendel MJ, Transfeldt EE et al (1993) The effects of immobilization of long segments of the spine on the adjacent and distal fact force and lumbosacral motion. Spine 18:2471–2479
Yasukawa Y (1994) Age changes in the lumbar spine; radiological follow-up studies over more than ten years. J Jpn Orthop Assoc 68:854–863 (Jpn)
Chosa E, Goto K, Totoribe K et al (2004) Analysis of the effect of lumbar spine fusion on the superior adjacent intervertebral disk in the presence of disk degeneration, using the three-dimensional finite element method. J Spinal Disord 17(2):134–139
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar and lumbosacral fusion: review of the literature. Spine 29:1938–1944
Hioki A, Miyamoto K, Kodama H et al (2005) Two-level posterior lumbar interbody fusion for degenerative disc disease: improved clinical outcome with restroration of lumbar lordosis. Spine J 5:600–607
Schlegel JD, Smith JA, Schleusener RL (1996) Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusion. Spine 21:970–981
Umehara S, Zindrick MR, Patwardhan AG et al (2000) The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine 25:1617–1624
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaito, T., Hosono, N., Fuji, T. et al. Disc space distraction is a potent risk factor for adjacent disc disease after PLIF. Arch Orthop Trauma Surg 131, 1499–1507 (2011). https://doi.org/10.1007/s00402-011-1343-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1343-0