Abstract
Introduction
The aim of our study was to compare the effectiveness of high-pressure pulsatile lavage and low-pressure lavage in patients with an orthopaedic implant infection treated with open débridement followed by antibiotic treatment.
Patients and methods
Patients with an orthopaedic implant infection requiring open débridement from January 2008 to August 2009 were randomized prospectively to a low-pressure or a high-pressure pulsatile lavage arm. Relevant information about demographics, co-morbidity, type of implant, microbiology data, surgical treatment, and outcome were recorded. Comparison of proportions was made using χ2 test or Fisher exact test when necessary. The Kaplan–Meier survival method was used to estimate the cumulative probability of treatment failure from open débridement to the last visit.
Results
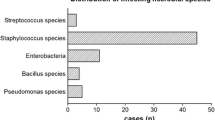
Seventy-nine patients were included. There were no differences between the main characteristics between both groups (p > 0.05). Mean (SD) age of the whole cohort was 70.2 (11.9) years. There were 46 infections on knee prosthesis, 17 on hip prosthesis, 7 on hip hemiarthroplasties and 9 on osteosynthesis devices. There were 69 acute post-surgical infections, 8 acute haematogenous infections and 2 chronic infections. The most common microorganisms isolated were coagulase-negative Staphylococci in 34 cases, Staphylococcus aureus in 26 and Escherichia coli in 19 cases. There were 30 polymicrobial infections. A total of 42 and 37 patients were randomized to a high-pressure pulsatile or a low-pressure lavage, respectively. There was no difference in the success rate between both arms (80.9 vs. 86.5%, p = 0.56).
Conclusion
The use of a high-pressure pulsatile lavage during open débridement of implant infections had a similar success rate as a low-pressure lavage.

Similar content being viewed by others
References
Barberán J, Aguilar L, Carroquino G et al (2006) Conservative treatment of staphylococcal prosthetic joint infections in elderly patients. Am J Med 119:7–10
Brandt CM, Sistrunk WW, Duffy MC et al (1997) Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin Infect Dis 24:914–919
Deirmengian C, Greenbaum J, Lotke PA et al (2003) Limited success with open debridement and retention of components in the treatment of acute staphylococcus aureus infections after total knee arthroplasty. J Arthroplasty 18:22–26
Martínez-Pastor JC, Muñoz-Mahamud E, Vilchez F et al (2009) Outcome of acute prosthetic joint infections due to gram-negative bacilli treated with open debridement and retention of the prosthesis. Antimicrob Agents Chemother 53:4772–4777
Soriano A, García S, Bori G et al (2006) Treatment of acute post-surgical infection of joint arthroplasty. Clin Microbiol Infect 12:930–933
Zimmerli W, Widmer AF, Blatter M et al (1998) Role of rifampin for treatment of orthopedic implant-related staphylococcal infections: a randomized controlled trial. foreign-body infection study group. JAMA 279:1537–1541
Marculescu CE, Berbari EF, Hanssen AD et al (2006) Outcome of prosthetic joint infections treated with debridement and retention of components. Clin Infect Dis 42:471–478
Bhandari M, Schemitsch EH (2002) High-pressure irrigation increases adipocyte-like cells at the expense of osteoblasts in vitro. J Bone Joint Surg Br 84:1054–1061
Hassinger SM, Harding G, Wongworawat MD (2005) High-pressure pulsatile lavage propagates bacteria into soft tissue. Clin Orthop Relat Res 439:27–31
Font-Vizcarra L, García S, Martínez-Pastor JC et al (2010) Blood culture flasks for culturing synovial fluid in prosthetic joint infections. Clin Orthop Relat Res 468(8):2238–2243
Hargrove R, Ridgeway S, Russell R et al (2006) Does pulse lavage reduce hip hemiarthroplasty infection rates? J Hosp Infect 62:446–449
Svoboda SJ, Bice TG, Gooden HA et al (2006) Comparison of bulb syringe and pulsed lavage irrigation with use of a bioluminescent musculoskeletal wound model. J Bone Joint Surg Am 88:2167–2174
Caprise PAJ, Miclau T, Dahners LE et al (2002) High-pressure pulsatile lavage irrigation of contaminated fractures: effects on fracture healing. J Orthop Res 20:1205–1209
Di Pasquale DJ, Bhandari M, Tov A et al (2007) The effect of high and low pressure pulsatile lavage on soft tissue and cortical blood flow: a canine segmental humerus fracture model. Arch Orthop Trauma Surg 127:879–884
Conflict of interest
For the present study, the authors have received a grant of 4000€ from Stryker®. No financial arrangement entered between the sponsor of the covered study and the study staff or an immediate family member involved in the conduct of the covered study, whereby the value of the grant has not influenced in the outcome of the study. The authors declare that they have no affiliations that might affect the objective and scientific presentation of this research. All authors have full control of all primary data and they agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muñoz-Mahamud, E., García, S., Bori, G. et al. Comparison of a low-pressure and a high-pressure pulsatile lavage during débridement for orthopaedic implant infection. Arch Orthop Trauma Surg 131, 1233–1238 (2011). https://doi.org/10.1007/s00402-011-1291-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1291-8