Abstract
Objectives
The aim of this study was to compare the radiological outcome of open and close reduction and osteosynthesis methods in the treatment of type II and III supracondylar humerus fractures in childhood with respect to the immediate post-operative reduction quality in sagittal plane.
Method
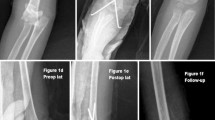
One hundred and forty four-pediatric patients with type IIb and III supracondylar humerus fractures treated at two centers between 1995 and 2005 were evaluated radiologically within a retrospective study. Seventy-six patients (54 boys, 22 girls, mean age 7.6, range 2–12) were treated by closed reduction and cross percutaneous pinning while 68 (49 boys, 19 girls, mean age 7.3, range 2–13) were treated by open reduction. The reduction quality of the open and closed groups was compared on immediate post-operative lateral radiographs by measuring of lateral humerocapitellar angle, anterior humeral line and anterior coronoid line criteria. The reduction quality was classified excellent, good, fair and poor according to the achievement of three, two, one or none of the criteria, respectively. Reductions classified as excellent and good were introduced as acceptable results.
Results
At least one criterion was achieved in all the patients of both the groups. The mean humerocapitellar angle was 30.1° in closed reduction group while the mean of it was 29.8° in open reduced group. Radiograph of 48 (63.1%) patients with closed reduction were found to display the anterior humeral line intersecting the middle one-third of capitellum while this criteria was 45 (66%) in open reduction group. The anterior coronoid line was disturbed in three patients in each of both the groups. The reduction quality was evaluated to be excellent in 32 patients, good in 31, fair in 13 at the closed reduction group while these evaluations were 31, 20 and 17 in open reduction group, respectively. Successful reduction was achieved in 74.9% of the patients in closed reduction group and 75% of the patients in open reduction group.
Conclusion
It is concluded that there was no significant difference between closed and open reductions of pediatric displaced supracondylar fractures with regard to the radiological criteria of reduction quality in sagittal plane.





Similar content being viewed by others
References
Fahey JJ (1960) Fractures ofs elbow in children. Instr Course Lect 17:13–46
Maylahn DJ, Fahey JJ (1958) Fractures of elbow in children. JAMA 166:220–228
Boyd DW, Aronson DD (1992) Supracondylar fractures of the humerus: a prospective study of percutaneous pinning. J Pediatr Orthop 12(6):789–794
Landin LA, Danielson LG (1986) Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand 57:309–312
Sarıoğlu A, Arpacıoğlu HÖ, Kıral A, Kuşkucu M, Rodoplu O, Kaplan H, Çilli F (1997) Çocuk humerus suprakondiler kırıklarında açık redüksiyon ve internal fiksasyon. Acta Orthop Traumatol Turc 31:1–4
Otsuka NY, Kasser JR (1997) Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg 5:19–26
Mesherle WL, Meehan PL (1992) Treatment of the displaced supracondylar fracture of the humerus (type III) with closed reduction and percutaneous cross-pin fixation. J Pediatr Orthop 12:789–794
Cheng JC, Shen WY (1993) Limb fracture pattern in different pediatric age groups, a study of 3,3350 children. J Orthop Trauma 7:15–22
Eliason EL (1924) Dressing for supracondylar fractures of the humerus. JAMA 82:1934–1935
Henrikson B (1966) Supracondylar fracture of the humerus in children. A late review of end-results with special reference to the cause of deformity, disability and complications. Acta Chir Scand Suppl 369:1–72
Woods GM, Tullos HG (1977) Elbow instability and medial epicondyle fracture. Am J Sports Med 5:23–30
Wilkins KE.(2006) Fracture and dislocation of teh elbow region. In: Rockwood CA Jr, Wilkins KE, King RE (eds). Fracture in children (3rd edn) Lippincott, New York
Hanlon CR, Estes WL Jr (1954) Fractures in childhood, a statistical analysis. Am J Surg 87(3):312–323
Arnold JA, Nasca RJ, Nelson CL (1977) Supracondylar fractures of the humerus: the role of dynamic factors in prevention of deformity. J Bone Joint Surg Am 59(5):589–595
Diri B, Tomak Y, Karaismailoglu TN (2003) The treatment of displaced supracondylar fractures of the humerus in children (an evaluation of three different treatment methods). Ulus Travma Acil Cerrahi Derg 9(1):62–69
Bombaci H, Gereli A, Kucukyazici O, Gorgec M, Deniz G (2007) The effect of surgical exposure on the clinic outcomes of supracondylar humerus fractures in children. Ulus Travma Acil Cerrahi Derg 13(1):49–54
de las Heras J, Duran D, de la Cerda J, Romanillos O, Martinez-Miranda J, Rodriguez-Merchan EC (2005) Supracondylar fractures of the humerus in children. Clin Orthop Relat Res (432):57–64
Abebneh M, Shannak A, Agabi S, Hadidi S (1998) The treatment of dispalced supracondylar fractures of the humerus in children. A comparison of three methods. Int Orthop (22):263–265
Flynn JC, Matthews JG, Benoit RL (1971) Blind pinning for displased supracondylar fractures of the humerus in children. J Bone Joint Surg A56:1096–1101
Griffin PP (1975) Supracondylar fractures of the humerus. Pediatr Clin North Am 22:477–486
Aranson DD, Prager BI (1987) Supracondylar fractures of the humerus in children, a modified technique for closed pinning. Clin Orthop 219:174–184
Williamson DM, Coates CJ, Miller RK, Cole WG (1992) Normal characteristics of the Baumann (humerocapitellar) angle: an aid in assessment of supracondylar fractures. J Pediatr Orthop 12:636
Dodge HS (1972) Displaced supracondylar fractures of the humerus in children: treatment by Dunlop’s traction. J Bone Joint Surg A54:1408
Wilkins KE (1984) Fractures and dislocations of the elbow region. In: Rockwood CA, Wilkins KE, King RE (eds) Fractures in children. vol 3. Lippincott, Philadelphia, pp 363–575
Biyani A, Gupta SP, Sharma JC (1993) Determination of medial epicondylar epiphyseal angle for supracondylar humeral fractures in children. J Pediatr Orthop 13:94
Roberts PH (1969) Dislocation of the elbow. Br J Surg 56:806–815
Silberstein MJ, Brodeur AE, Graviss ER, Atchawee L (1981) Some vagaries of the capitellum. J Bone Joint Surg A63:524–528
Wilkins KE (1990) The operative management of supracondylar fractures. Orthop Clin North Am 21:269
Pirone AM, Graham HK, Krajbich JI (1988) Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg A70:641
O’hara LJ, Barlow JW, Clarke NM (2000) Displaced supracondylar fractures of the humerus in children. Audit changes practice. J Bone Joint Surg B82:204–210
Williamson DM, Coates CJ, Miller RK, Cole WG (1992) Normal characteristics of the Baumann (humerocapitellar) angle: an aid in assessment of supracondylar fractures. J Pediatr Orthop 12:636
Webb AJ, Sherman FC (1989) Supracondylar fractures of the humerus in children. J Pediatr Orthop 9:315
Mohammad S, Rymaxzewski LA, Runciman J (1999) The Baumann angle in supracondylar fractures of the distal humerus in children. J Pediatr Orthop 19:65
Foster BK, Paterson DC (1991) Difficult supracondylar elbow fractures in children: analysis of percutaneous pinning technique. J Pediatr Orthop 12:11
Fowles JV, Kassab MT (1974) Displaced supracondylar fractures of the elbow in children. J Bone Joint Surg B56:490
French PR (1959) Varus deformity of elbow following supracondylar fractures of the humerus in children. Lancet 2:439
Fuller DJ, McCullough CJ (1982) Malunited fractures of the forearm in children. J Bone Joint Surg B64:364
Skibo L, Reed MH (1994) A criterion for a true lateral radiograph of the elbow. Can Assoc Radiol J 45:287–291
Marion J, LaGrange J, Faysse R, Rigault P (1962) Les fractures d l’extremite inferieure de l’humerus chez l’enfant. Rev Chir Orthop 48:337
Korner J, Rommens PM, Hepp P (2004) Spontaneous defect remodeling in a distal humerus fracture with extensive osseous loss: a case report of a complex elbow fracture. J Orthop Trauma 46(6):524–528
Zatti G, Bini A, De Pietri M (2001) The surgical treatment of supracondylar fractures of the humerus in children by percutaneous fixation using Kirschner wires: analysis of residual deformities. Chir Organi Mov 86(2):111–117
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turhan, E., Aksoy, C., Ege, A. et al. Sagittal plane analysis of the open and closed methods in children with displaced supracondylar fractures of the humerus (a radiological study). Arch Orthop Trauma Surg 128, 739–744 (2008). https://doi.org/10.1007/s00402-007-0523-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0523-4