Abstract
Background
To analyze in-hospital complications in patients with acute ST-elevation myocardial infarction (STEMI) depending on renal function.
Design
Observational study in patients with STEMI.
Methods
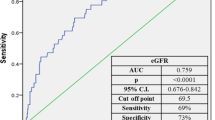
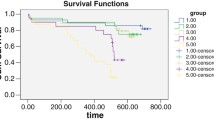
The study included 169 patients undergoing primary percutaneous coronary intervention. In all patients glomerular filtration rate (GRF) was calculated using the Modification of Diet in Renal Disease Study (MDRD) equation. Of these patients, 84 had a GFR ≥ 90 ml/min/1.73 m2 (Group 1) and 85 < 90 ml/min/1.73 m2 (Group 2). Other parameters in both groups were comparable. Study groups were followed to compare Killip class > 2 acute heart failure, in-hospital pneumonia, pulseless ventricular tachycardia or ventricular fibrillation, new onset atrial fibrillation, and high grade atrioventricular block. All patients were treated according to European Society of Cardiology (ESC) guidelines for the management of acute myocardial infarction in patients presenting with ST elevation.
Results
Mean GFR in Group 1 was 107.6 \(\pm 17.8\) and in Group 2 75.3 \(\pm\) 11.2 (p < 0.0001). The incidence of atrial fibrillation was higher in Group 2: in Group 1 and Group 2 the atrial fibrillation rate was 1.12% (one of 84) vs 8.24% (seven of 85) (p = 0.031), respectively. Group 1 revealed significantly lower rates of acute heart failure (Killip class > 2): in Group 1 and Group 2 0% (0 of 84 patients) vs 5.88% (five of 85 patients) (p = 0.024), respectively. The authors found no significant differences for other complications: in Group 1 and Group 2 ventricular tachycardia or ventricular fibrillation was 4.76% (four of 84 patients) vs 5.89% (five of 85 patients) (p = 0.75), high grade atrioventricular block was 2.38% (two of 84 patients) vs 4.71% (four of 85 patients) (p = 0.41), and the in-hospital pneumonia rate was 2.38% (two of 84 patients) vs 4.71% (four of 85 patients) (p = 0.41), respectively.
Conclusion
Patients with lower GFR were more likely to suffer from in-hospital acute heart failure (Killip class > 2) and atrial fibrillation in STEMI despite primary percutaneous coronary intervention. Renal function did not affect in-hospital pneumonia, pulseless ventricular tachycardia or ventricular fibrillation rates. The evaluation of kidney function through GFR in STEMI patients may make in-hospital complications more predictable.
Zusammenfassung
Hintergrund
Die sich stationär bei Patienten mit akutem ST-Hebungsinfarkt (STEMI [„ST-elevation myocardial infarction“]) ereignenden Komplikationen wurden bezüglich ihrer Abhängigkeit von der Nierenfunktion analysiert.
Studiendesign
Es handelte sich um eine Beobachtungsstudie bei STEMI-Patienten.
Methoden
In die Studie wurden 169 Patienten, die einer primären perkutanen koronaren Intervention unterzogen worden waren, eingeschlossen. Bei allen Probanden wurde die glomeruläre Filtrationsrate (GFR) mittels der Gleichung der MRDR-Studie (MDRD: „modification of diet in renal disease“) ermittelt. Von ihnen hatten 84 eine GFR ≥ 90 ml/min/1,73 m2 (Gruppe 1) und 85 eine GFR < 90 ml/min/1,73 m2 (Gruppe 2). Andere Parameter beider Gruppen waren vergleichbar. Die Studiengruppen wurden bezüglich der Häufigkeit des Auftretens von akuter Herzinsuffizienz (Killip-Klasse > 2), im Krankenhaus auftretender Pneumonie, pulsloser ventrikulärer Tachykardie oder Kammerflimmern, neu auftretendem Vorhofflimmern und hochgradigem atrioventrikulärem (AV) Block verglichen. Alle Patienten wurden nach den ESC-Leitlinien (ESC: „European Society of Cardiology“) zum Management des akuten Myokardinfarkts bei ST-Hebung behandelt.
Ergebnisse
Die mittlere GFR in Gruppe 1 bzw. 2 war 107,6 \(\pm 17,8\) bzw. 75,3 \(\pm\)11,2 (p < 0,0001). Die Inzidenz von Vorhofflimmern war in Gruppe 2 höher: In Gruppe 1 betrug diese 1,12 % (1 von 84), in Gruppe 2 8,24 % (7 von 85; p = 0,031). Bei den Probanden von Gruppe 1 kam es signifikant seltener zur akuten Herzinsuffizienz (Killip-Klasse > 2): In Gruppe 1 trat diese bei 0 % (0 von 84 Patienten) auf vs. 5,88 % (5 von 85 Patienten) in Gruppe 2 (p = 0,024). Für die anderen Komplikationen wurden keine signifikanten Unterschiede festgestellt: Ventrikuläre Tachykardie oder Kammerflimmern traten in Gruppe 1 bei 4,76 % (4 von 84 Patienten), in Gruppe 2 bei 5,89 % (5 von 85 Patienten) auf (p = 0,75), ein hochgradiger AV-Block bei 2,38 % (2 von 84 Patienten) vs. 4,71 % (4 von 85 Patienten; p = 0,41), und stationär eine Pneumonie wurde bei 2,38 % (2 von 84 Patienten) bzw. 4,71 % (4 von 85 Patienten) beobachtet (p = 0,41).
Schlussfolgerung
Bei Patienten mit STEMI und niedriger GFR kam es trotz primärer perkutaner koronarer Intervention eher zur akuten Herzinsuffizienz (Killip-Klasse > 2) im Krankenhaus und Vorhofflimmern. Die Häufigkeiten des Auftretens von Pneumonie im Krankenhaus, pulsloser ventrikulärer Tachykardie oder Kammerflimmern waren nicht mit der Nierenfunktion assoziiert. Die Beurteilung der Nierenfunktion mittels GFR-Bestimmung bei STEMI-Patienten kann das Auftreten von Komplikationen im Krankenhaus vorhersehbarer machen.
Similar content being viewed by others
References
Kuller LH (2003) Hormone replacement therapy and risk of cardiovascular disease: implications of the results of the women’s health initiative. Arterioscler Thromb Vasc Biol 23:11–16
Di Carli MF, Janisse J, Grunberger G, Ager J (2003) Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol 41(8):1387–1393
Wison S, Foo K, Cunningham J et al (2003) Renal function and risk stratification in acute coronary syndromes. Am J Cardiol 91:1051–1054
Herzog CA, Ma JZ, Collins AJ (1998) Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med 339(12):799–805
Gibson CM, Pinto DS, Murphy SA et al (2003) Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol 42:1535–1543
Luft FC (2000) Renal disease as a risk factor for cardiovascular disease. Basic Res Cardiol 95(1):I72–I76
Foley RN, Parfrey PS, Sarnak MJ (1998) Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 9:S16–S23
Sarnak MJ, Levey AS (2000) Cardiovascular disease and chronic renal disease: a new paradigm. Am J Kidney Dis 35(1):S117–S131
Chertow GM, Normand SLT, Silva LR, McNeil BJ (2000) Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis 35:1044–1051
Wright RS, Reeder GS, Herzog CA et al (2002) Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med 137:563–570
Al Suwaidi J, Reddan DN, Williams K et al (2002) Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation 106:974–980
Masoudi FA, Plomondon ME, Magid DJ, Sales A, Rumsfeld JS (2004) Renal insufficiency and mortality from acute coronary syndromes. Am Heart J 147:623–629
Michalis LK, Stroumbis CS, Pappas K, Sourla E, Niokou D, Goudevenos JA et al (2000) Treatment of refractory unstable angina in geographically isolated areas without cardiac surgery: Invasive versus conservative strategy (TRUCS study). Eur Heart J 21:1954–1959
Chaitman BR, McMahon RP, Terrin M, Younis LT, Shaw LJ, Weiner DA, Frederick MM, Knatterud GL, Sopko G, Braunwald E (1993) Impact of treatment strategy on predischarge exercise test in the thrombolysis in myocardial infarction (TIMI) II trial. Am J Cardiol 71:131–138
Kim JW, Lim DS, Sun K, Shim WJ, Rho YM (2005) Stenting or MIDCAB using ministernotomy for revascularization of proximal left anterior descending artery? Int J Cardiol 99:437–441
Germing A, Lindstaedt M, Ulrich S, Grewe P, Bojara W, Lawo T, von Dryander S, Jager D, Machraoui A, Mugge A, Lemke B (2005) Normal angiogram in acute coronary syndrome: preangiographic risk stratification, angiographic findings and follow-up. Int J Cardiol 99:19–23
Chiamvimonvat V, Goodman SG, Langer A, Barr A, Freeman MR (2001) Prognostic value of dipyridamole SPECT imaging in low-risk patients after myocardial infarction. J Nucl Cardiol 8:136–143
Schachinger V, Kasper W, Zeiher AM (1996) Adjunctive intracoronary urokinase therapy during percutaneous transluminal coronary angioplasty. Am J Cardiol 77:1174–1178
Sarnak MJ, Levey AS, Schoolwerth AC et al (2003) Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American heart association councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Hypertension 42:1050–1065
Gibson CM, Dumaine RL, Gelfand EV et al (2004) Association of glomerular filtration rate on presentation with subsequent mortality in non-STsegment elevation acute coronary syndrome; observations in 13307 patients in five TIMI trials. Eur Heart J 25:1998–2005
Santopinto JJ, Fox KAA, Goldberg RJ et al (2003) Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE). Heart 89:1003–1008
Herzog CA, Littrell K, Arko C, Frederick PD, Blaney M (2007) Clinical characteristics of dialysis patients with acute myocardial infarction in the United States: a collaborative project of the United States renal data system and the national registry of myocardial infarction. Circulation 116:1465–1472
Ba J, Brown D, Friedman PA (2003) Calcium-sensing receptor regulation of PTH-inhibitable proximal tubule phosphate transport. Am J Physiol Renal Physiol 285:F1233–F1243
Sosnov J, Lessard D, Goldberg RJ, Yarzebski J, Gore JM (2006) Differential symptoms of acute myocardial infarction in patients with kidney disease: a community-wide perspective. Am J Kidney Dis 47:378–384
Bassand JP, Hamm CW, Ardissino D et al (2007) Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 28:1598–1660
Van de Werf F, Bax J, Betriu A et al (2008) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the task force on themanagement of ST-segment elevation acute myocardial infarction of the European society of cardiology. Eur Heart J 29:2909–2945
Reddan DN, Szczech L, Bhapkar MV et al (2005) Renal function, concomitant medication use and outcomes following acute coronary syndromes. Nephrol Dial Transplant 20(10):2105–2112
Brosius FC III, Hostetter TH, Kelepouris E et al (2006) Detection of chronic kidney disease in patients with or at increased risk of cardiovascular disease: a science advisory from the American heart association kidney and cardiovascular disease council; the councils on high blood pressure research, cardiovascular disease in the young, and epidemiology and prevention; and the quality of care and outcomes research interdisciplinaryworking group: developed in collaboration with the national kidney foundation. Circulation 114:1083–1087
Minai K, Horie H, Takahashi M, Nozawa M (2002) Kinoshita M long-term outcome of primary percutaneous transluminal coronary angioplasty for low-risk acute myocardial infarction in patients older than 80 yr: a single-center, open, randomized trial. Am Heart J 143:497–505
Chen JS, Hwang CL, Lee DY, Chen YT (1995) Regression of left ventricular aneurysm after delayed percutaneous transluminal coronary angioplasty (PTCA) in patients with acute myocardial infarction. Int J Cardiol 48:39–47
Gibbons RJ, Holmes DR, Reeder GS, Bailey KR, Hopfenspirger MR, Gersh BJ (1993) Immediate angioplasty compared with the administration of a thrombolytic agent followed by conservative treatment for myocardial infarction. The mayo coronary care unit and catheterization laboratory groups. N Engl J Med 328:685–691
Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O’Keefe J, Overlie P, Donohue B, Chelliah N, Timmis GC et al (1993) A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The primary angioplasty in myocardial infarction study group. N Engl J Med 328:673–679
No authors listed (1997) Coronary angioplasty versus medical therapy for angina: the second randomized intervention treatment of angina (RITA-2) trial. RITA‑2 trial participants. Lancet 350:461–468
Coca SG, Krumholz HM, Garg AX, Parikh CR (2006) Underrepresentation of renal disease in randomized controlled trials of cardiovascular disease. JAMA 296(11):1377–1384. https://doi.org/10.1001/jama.296.11.1377
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med 130:461–470
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S et al (2018) 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J 39(2):119–177. https://doi.org/10.1093/eurheartj/ehx393
Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G et al (2015) 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European society of cardiology (ESC) endorsed by: association for European paediatric and congenital cardiology (AEPC). Eur Heart J 36(41):2793–2867. https://doi.org/10.1093/eurheartj/ehv316
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener H‑C, Heidbuchel H, Hendriks J et al (2016) 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37(38):2893–2962. https://doi.org/10.1093/eurheartj/ehw210
Kalil AC, Metersky ML, Klompas M et al (2016) Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of america and the American thoracic society. Clin Infect Dis 63:e61–e111
Levey AS, Eckardt K‑U et al (2005) Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int 67(6):2089–2100
National Kidney Foundation (2002) K ⁄ DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1–266
Ibanez B et al (2018) ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. https://doi.org/10.1093/eurheartj/ehx393
Acknowledgements
The authors would like to thank all patients that contributed to the success of the study.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Hamlet Hayrapetyan and Harutyun Petrosyan conceived of the study. All authors participated in its design and coordination and helped to draft the manuscript. Hamlet Hayrapetyan and Harutyun Petrosyan drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
H. Petrosyan, H. Hayrapetyan, S. Torozyan, A. Tsaturyan and S. Tribunyan declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Availability of data and material
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Petrosyan, H., Hayrapetyan, H., Torozyan, S. et al. In-hospital complications in acute ST-elevation myocardial infarction depending on renal function. Herzschr Elektrophys 32, 359–364 (2021). https://doi.org/10.1007/s00399-021-00782-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-021-00782-3
Keywords
- Acute coronary syndrome
- STEMI
- Percutaneous coronary intervention
- Renal dysfunction
- Glomerular filtration rate