Abstract
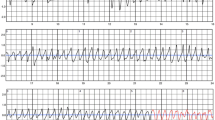
Peripartum cardiomyopathy (PPCM) is a rare but life-threatening heart disease, with onset in the last month of pregnancy or in the first months after delivery. Extensive studies on the burden of supraventricular and ventricular arrhythmias are lacking. Patients with PPCM present with electrocardiographic findings typical in acute heart failure. Management of arrhythmias in PPCM depends on the severity and the onset (during pregnancy or after delivery). Studies on the use of the wearable cardioverter–defibrillator in patients with PPCM show a substantial burden of ventricular tachyarrhythmias and sudden death in patients with severely reduced left ventricular function. The aim of the present article is to summarize actual knowledge on electrocardiogram findings, arrhythmias, and sudden cardiac death in patients with PPCM.
Zusammenfassung
Die Peripartumkardiomyopathie (PPCM) ist eine seltene, aber lebensbedrohliche Herzerkrankung, die in den letzten Schwangerschaftsmonaten oder den ersten Monaten nach der Entbindung auftritt. Detaillierte Studien zur Arrhythmielast durch supraventrikuläre und ventrikuläre Arrhythmien bei PPCM liegen nicht vor. Patientinnen mit PPCM weisen die typischen EKG-Befunde einer akuten Herzinsuffizienz auf. Die Behandlung von Arrhythmien bei PPCM hängt von der Schwere und vom Zeitpunkt des Auftretens – während der Schwangerschaft oder nach der Entbindung – ab. Studien mit tragbaren Defibrillatoren bei Patientinnen mit PPCM konnten relevante ventrikuläre Tachyarrhythmien und plötzlichen Herztod bei Patientinnen mit schwer eingeschränkter linksventrikulärer Funktion nachweisen. Ziel der vorliegenden Übersichtsarbeit ist es, die aktuelle Datenlage zu EKG, Arrhythmien und plötzlichem Herztod bei Patientinnen mit PPCM zusammenzufassen.


Similar content being viewed by others
References
Bauersachs J, Arrigo M, Hilfiker-Kleiner D et al (2016) Current management of patients with severe acute peripartum cardiomyopathy: practical guidance from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur J Heart Fail 18:1096–1105. https://doi.org/10.1002/ejhf.586
Bauersachs J, König T, van der Meer P et al (2019) Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur J Heart Fail 21:827–843. https://doi.org/10.1002/ejhf.1493
DeBenedetti Zunino ME, Schuger C, Lahiri M (2014) High rate of ventricular arrhythmias in women with peripartum cardiomyopathy and implanted cardioverter defibrillators. J Am Coll Cardiol 63:A313. https://doi.org/10.1016/S0735-1097(14)60313-2
Diao M, Diop IB, Kane A et al (2004) Electrocardiographic recording of long duration (Holter) of 24 hours during idiopathic cardiomyopathy of the peripartum. Arch Mal Coeur Vaiss 97:25–30
Duncker D, Haghikia A, König T et al (2014) Risk for ventricular fibrillation in peripartum cardiomyopathy with severely reduced left ventricular function-value of the wearable cardioverter/defibrillator. Eur J Heart Fail 16:1331–1336. https://doi.org/10.1002/ejhf.188
Duncker D, Westenfeld R, Konrad T et al (2017) Risk for life-threatening arrhythmia in newly diagnosed peripartum cardiomyopathy with low ejection fraction: a German multi-centre analysis. Clin Res Cardiol 12:767–768. https://doi.org/10.1007/s00392-017-1090-5
Ekizler FA, Cay S, Kafes H et al (2019) The prognostic value of positive T wave in lead aVR: a novel marker of adverse cardiac outcomes in peripartum cardiomyopathy. Ann Noninvasive Electrocardiol 24:e12631. https://doi.org/10.1111/anec.12631
Ersbøll AS, Johansen M, Damm P et al (2017) Peripartum cardiomyopathy in Denmark: a retrospective, population-based study of incidence, management and outcome. Eur J Heart Fail 19:1712–1720. https://doi.org/10.1002/ejhf.882
Goland S, Modi K, Bitar F et al (2009) Clinical profile and predictors of complications in peripartum cardiomyopathy. J Card Fail 15:645–650. https://doi.org/10.1016/j.cardfail.2009.03.008
Hilfiker-Kleiner D, Haghikia A, Berliner D et al (2017) Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study. Eur Heart J 38:2671–2679. https://doi.org/10.1093/eurheartj/ehx355
Hilfiker-Kleiner D, Haghikia A, Nonhoff J, Bauersachs J (2015) Peripartum cardiomyopathy: current management and future perspectives. Eur Heart J 36:1090–1097. https://doi.org/10.1093/eurheartj/ehv009
Hilfiker-Kleiner D, Kaminski K, Podewski E et al (2007) A cathepsin D‑cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell 128:589–600. https://doi.org/10.1016/j.cell.2006.12.036
Hoevelmann J, Viljoen CA, Manning K et al (2019) The prognostic significance of the 12-lead ECG in peripartum cardiomyopathy. Int J Cardiol 276:177–184. https://doi.org/10.1016/j.ijcard.2018.11.008
Honigberg MC, Elkayam U, Rajagopalan N et al (2019) Electrocardiographic findings in peripartum cardiomyopathy. Clin Cardiol 42:524–529. https://doi.org/10.1002/clc.23171
Karaye KM, Lindmark K, Henein MY (2016) Electrocardiographic predictors of peripartum cardiomyopathy. Cardiovasc J Afr 27:66–70. https://doi.org/10.5830/CVJA-2015-092
Krexi D, Sheppard MN (2017) Cardiovascular causes of maternal sudden death. Sudden arrhythmic death syndrome is leading cause in UK. Eur J Obstet Gynecol Reprod Biol 212:155–159. https://doi.org/10.1016/j.ejogrb.2017.03.006
Labidi S, Hilfiker-Kleiner D, Klein G (2011) Left bundle branch block during pregnancy as a sign of imminent peripartum cardiomyopathy. Eur Heart J 32:1076. https://doi.org/10.1093/eurheartj/ehq487
Laghari AH, Khan AH, Kazmi KA (2013) Peripartum cardiomyopathy: ten year experience at a tertiary care hospital in Pakistan. BMC Res Notes 6:495. https://doi.org/10.1186/1756-0500-6-495
Mallikethi-Reddy S, Akintoye E, Trehan N et al (2017) Burden of arrhythmias in peripartum cardiomyopathy: analysis of 9841 hospitalizations. Int J Cardiol 235:114–117. https://doi.org/10.1016/j.ijcard.2017.02.084
Mbakwem AC, Bauersachs J, Viljoen C et al (2021) Electrocardiographic features and their echocardiographic correlates in peripartum cardiomyopathy: results from the ESC EORP PPCM registry. ESC Heart Fail 97:25. https://doi.org/10.1002/ehf2.13172
Ntusi NBA, Badri M, Gumedze F et al (2015) Pregnancy-associated heart failure: a comparison of clinical presentation and outcome between hypertensive heart failure of pregnancy and idiopathic Peripartum Cardiomyopathy. Plos One 10:e133466. https://doi.org/10.1371/journal.pone.0133466
Opotowsky AR, Siddiqi OK, D’Souza B et al (2012) Maternal cardiovascular events during childbirth among women with congenital heart disease. Heart 98:145–151. https://doi.org/10.1136/heartjnl-2011-300828
Pfeffer TJ, Klüsch V, Duncker D et al (2020) Long-term follow-up of patients with peripartum cardiomyopathy and an implantable cardioverter defibrillator—a multicenter study. Clin Res Cardiol 109:V639. https://doi.org/10.1007/s00392-020-01621-0
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. https://doi.org/10.1093/eurheartj/ehw128
Priori SG, Blomström-Lundqvist C, Mazzanti A et al (2015) 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Europace 17:1601–1687. https://doi.org/10.1093/europace/euv319
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J et al (2018) 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J 39:3165–3241. https://doi.org/10.1093/eurheartj/ehy340
Saltzberg MT, Szymkiewicz S, Bianco NR (2012) Characteristics and outcomes of peripartum versus nonperipartum cardiomyopathy in women using a wearable cardiac defibrillator. J Card Fail 18:21–27. https://doi.org/10.1016/j.cardfail.2011.09.004
Sliwa K, Hilfiker-Kleiner D, Petrie MC et al (2010) Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail 12:767–778. https://doi.org/10.1093/eurjhf/hfq120
Sliwa K, Petrie MC, van der Meer P et al (2020) Clinical presentation, management, and 6‑month outcomes in women with peripartum cardiomyopathy: an ESC EORP registry. Eur Heart J 41:3787–3797. https://doi.org/10.1093/eurheartj/ehaa455
Tanaka H, Katsuragi S, Osato K et al (2017) The increase in the rate of maternal deaths related to cardiovascular disease in Japan from 1991–1992 to 2010–2012. J Cardiol 69:74–78. https://doi.org/10.1016/j.jjcc.2016.01.005
Tibazarwa K, Lee G, Mayosi B et al (2012) The 12-lead ECG in peripartum cardiomyopathy. Cardiovasc J Afr 23:322–329. https://doi.org/10.5830/CVJA-2012-006
Vaidya VR, Arora S, Patel N et al (2017) Burden of Arrhythmia in Pregnancy. Circulation 135:619–621. https://doi.org/10.1161/CIRCULATIONAHA.116.026681
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Duncker has received speaker honoraria and/or travel grants from Abbott, Astra Zeneca, Bayer, Biotronik, Boehringer Ingelheim, Boston Scientific, Medtronic, Pfizer, and Zoll. J. Bauersachs reports honoraria for lectures and/or consulting from Novartis, BMS, Pfizer, Vifor, Bayer, Servier, Daichii Sankyo, CVRx, MSD, Boehringer Ingelheim, Cardior, AstraZeneca, Abiomed, Abbott, and Medtronic, and research support from Zoll, CVRx, and Vifor. C. Veltmann has received honoraria for lectures and/or consulting from Abbott, Astra Zeneca, Bayer, Biotronik, BMS, Boehringer Ingelheim, Boston Scientific, CVRx, Daichii Sankyo, Medtronic, and Zoll. T.J. Pfeffer declares that he has no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Duncker, D., Pfeffer, T.J., Bauersachs, J. et al. ECG and arrhythmias in peripartum cardiomyopathy. Herzschr Elektrophys 32, 207–213 (2021). https://doi.org/10.1007/s00399-021-00760-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-021-00760-9