Abstract
Background
Intraoperative testing of implantable cardioverter–defibrillators (ICDs) is time consuming and associated with risks. In the present study, we elucidated whether the initial implantation of an ICD with high energy output makes intraoperative defibrillation threshold testing (DFTT) unnecessary even though antiarrhythmic (AA) therapy is needed in the future.
Methods
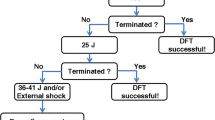
A total of 111 patients (94 men, 17 women) receiving an ICD with subsequent AA therapy (mexiletine, amiodarone, sotalol, flecainide) were analyzed retrospectively. DFT was performed during ICD implantation and after AA drug therapy. In a second step, DFT results from the study cohort were analyzed for implantation of virtual ICDs with either low (≤ 30 J, LOD), intermediate (34 J, IOD), or high energy output (36 J, HOD).
Results
In the study cohort, all patients reached the safety margin (SM) of 10 J between DFT and maximal shock energy of the ICD. After loading of AA agents, 6 patients (12%) with a LOD, 3 patients (11%) with an IOD, and 3 (13%) patients with a HOD failed the 10 J SM. Using virtual ICDs, 6 (5.5%) patients with a LOD, 1 patient (1%) with an IOD, and no patients with a HOD would have failed the 10 J SM. After loading of AA agents, 18 patients (16%) with a virtual LOD, 12 patients (10.8%) with an IOD, and still 9 patients (8%) with a HOD would have failed the 10 J SM.
Conclusion
Our results demonstrate that the 10 J SM would have been achieved intraoperatively in all patients with virtual HOD ICDs. Thus, determination of the DFT during implantation does not seem to be obligatory. However, in patients receiving AA agents, DFT testing is still required.
Zusammenfassung
Hintergrund
Die intraoperative Testung von implantierbaren Kardioverter/Defibrillatoren (ICD) ist personalintensiv und mit Komplikationen vergesellschaftet. In der vorliegenden Studie untersuchten wir, ob bei ICD-Implantationen mit unterschiedlicher maximaler Energieabgabe eine intraoperative Testung inklusive der Induktion von Kammerflimmern (DFT) notwendig gewesen wäre.
Material und Methoden
In einer retrospektiven Studie erhielten 111 Patienten (94 männlich, 17 weiblich) einen ICD. Nach Auftreten von ventrikulären Tachyarrhythmien wurden im weiteren Verlauf alle Patienten mit antiarrhythmischen Substanzen aufgesättigt (Mexiletin, Amiodaron, Sotalol, Flecainid). DFT-Testungen wurden intraoperativ und nach Aufsättigung mit antiarrhythmischen Substanzen durchgeführt. In einem zweiten Schritt wurden die DFT-Resultate der Studienkohorte analysiert hinsichtlich virtueller ICDs mit unterschiedlicher maximaler Energieabgabe ≤ 30 J (LOD), 34 J (IOD) oder 36 J (HOD).
Ergebnisse
Während Implantation erreichten alle Patienten die Sicherheitsmarge von 10 J (10-J-SM) zwischen maximaler Energieabgabe und DFT. Nach Aufsättigung mit antiarrhythmischen Substanzen verpassten 6 Patienten (12%) mit LOD, 3 Patienten (11%) mit IOD und 3 Patienten (13%) mit HOD die 10-J-Sicherheitsmarge. Hätte man für die Kohorte virtuelle ICDs mit LOD, IOD oder HOD implantiert, so hätten sechs (5,5%), ein (1%) bzw. kein Patient(en) (0%) die 10-J-SM nicht erreicht. Im Falle einer Aufsättigung der Studienkohorte mit antiarrhythmischen Substanzen hätten 18 (16%), 12 (10,8%) bzw. 9 (8%) der Patienten mit virtuellen ICDs (LOD/IOD/HOD) die 10-J-SM verpasst.
Schlussfolgerung
Die vorliegende Studie zeigt, dass intraoperativ bei allen Patienten mit virtuellem HOD-ICD die 10-J-SM erreicht worden wäre, jedoch nicht nach Aufsättigung mit antiarrhythmischen Substanzen. Eine intraoperative Testung aller Patienten mit HOD scheint entsprechend verzichtbar, solange keine Aufsättigung mit einem Antiarrhythmikum erfolgt.
Similar content being viewed by others
References
Bardy GH, Lee KL, Mark DB et al (2005) Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352:225–237
Bhandari AK, Isber N, Estioko M et al (1998) Efficacy of low-energy T wave shocks for induction of ventricular fibrillation in patients with implantable cardioverter defibrillators. J Electrocardiol 3:31–37
Moss AJ, Zareba W, Hall WJ et al (2002) Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346:877–883
Moss AJ, Hall WJ, Cannom DS et al (1996) Improved survival with an implantable defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med 335:1933–1940
Gauder D, Vohl MC, Perron P et al (1997) The Antiarrhythmics Versus Implantable Defibrillator Investigators. A comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from near-fatal arrhythmias. N Engl J Med 337:1576–1583
Blatt JA, Poole JE, Johnson GW et al (2008) No benefit from defibrillation threshold testing in the SCD-HeFT (Sudden Cardiac Death in Heart Failure Trial). J Am Coll Cardiol 52:551–556
Bakker P, Viens E, Vries J de, Bredee J (1994) Impact of defibrillation threshold testing on cerebral circulation and oxygenation. PACE 17:802
Benedini G, Marchini A, Curnis A et al (1995) Implantable defibrillator and thromboembolic event. PACE, 18:199–202
Tokano T, Bach D, Chang J et al (1998) The effect of ventricular shock strength on caridac hemodynamics. J Cardiovasc Electrophysiol 9:791–797
Hall B, Jeevanantham V, Levine E et al (2007) Comparison of outcomes in patients undergoing defibrillation threshold testing at the time of implantable cardioverter-defibrillator implantation versus no defibrillation threshold testing. Cardiol J 14:463–469
Russo AM, Sauer W, Gerstenfeld EP et al (2005) Defibrillation threshold testing: is it really necessary at the time of implantable cardioverterdefibrillator insertion? Heart Rhythm 2:456–461
Epstein AE, Ellenbogen KA, Kirk KA et al (1992) Clinical characteristics of patients with high defibrillation thresholds. Circulation 86:1206–1216
Theuns DA, Szili-Torok T, Jordaens LJ (2005) Defibrillation efficacy testing: long-term follow-up and mortality. Europace 7:509–515
DeSouza C, Koehler J, DeGroot P (1998) Failing defibrillator implant criterion on the initial attempt is a predictive factor for sudden cardiac death. Pacing Clin Electrophysiol 21:801 (abstract)
Shukla HH, Flaker GC, Jayam V, Roberts D (2003) High defibrillation thresholds in transvenous biphasic implantable defibrillators: Clinical predictors and prognostic implications. Pacing Clin Electrophysiol 26:44–48
Gula LJ, Massel D, Krahn AD, Yee R et al (2008) Is defibrillation testing still necessary? A decision analysis and Markov model. J Cardiovasc Electrophysiol 19:400–405
Gold MR, Higgins S, Klein R et al (2002) Efficacy and temporal stability of reduced safety margins for ventricular defibrillation: Primary results from the Low Energy Safety Study (LESS). Circulation 105(17):2043–2048
Manz M, Jung W, Luderitz B (1994) Interactions between drugs and devices: experimental and clinical studies. Am Heart J 127(4 Pt 2):978–984
Carnes CA, Mehdirad AA, Nelson SD (1998) Drug and defibrillator interactions. Pharmacotherapy 18(3):516–525
Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators (1997) A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from nearfatal ventricular arrhythmias. The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. N Engl J Med 337(22):1576–1583
Pelosi F Jr, Oral H, Kim MH et al (2000) Effect of chronic amiodarone therapy on defibrillation energy requirements in humans. J Cardiovasc Electrophysiol 11(7):736–740
Hohnloser SH, Dorian P, Roberts R et al (2006) Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation 114(2):104–109
Zhou L, Chen BP, Kluger J et al (1998) Effects of amiodarone and its active metabolite desethylamiodarone on the ventricular defibrillation threshold. J Am Coll Cardiol 31(7):1672–1678
Dorian P (2000) Amiodarone and defibrillation thresholds: a clinical conundrum. J Cardiovasc Electrophysiol 11(7):741–743
Kuhlkamp V, Mewis C, Suchalla R (1999) Effect of amiodarone and sotalol on the defibrillation threshold in comparison to patients without antiarrhythmic drug treatment. Int J Cardiol 69(3):271–279
Jung W, Manz M, Pizzulli L et al (1992) Effects of chronic amiodarone therapy on defibrillation threshold. Am J Cardiol 70(11):1023–1027
Swerdlow CD, Russo AM, Degroot PJ (2007) The dilemma of ICD implant testing. Pacing Clin Electrophysiol 30:675–700
Goldschlager N, Epstein A, Friedman P et al (2001) Environmental and drug effects on patients with pacemakers and implantable cardioverter/defibrillators: a practical guide to patient treatment. Arch Intern Med 161(5):649–655
Rajawat YS, Dias D, Gerstenfeld EP et al (2002) Interactions of antiarrhythmic drugs and implantable devices in controlling ventricular tachycardia and fibrillation. Curr Cardiol Rep 4(5):434–440
Topham SL, Cha YM, Peters BB, Chen PS (1992) Effects of lidocaine on relation between defibrillation threshold and upper limit of vulnerability in open-chest dogs. Circulation 85(3):1146–1151
Peters RW, Gilbert TB, Johns-Walton S, Gold MR (1997) Lidocaine related increase in defibrillation threshold. Anesth Analg 85(2):299–300
Ellenbogen KA, Kay GN, Lau CP, Wilkoff BL (eds) (2007) Clinical cardiac pacing, defibrillation, and resynchronization therapy, 3rd edn. Saunders, Philadelphia, PA
Gold MR, Olsovsky MR, Pelini MA et al (1998) Comparison of single- and dual-coil acive pectoral defibrillation lead systems. J Am Coll Cardiol 31:1391–1394
Birnie D, Tung S, Simpson D et al (2008) Complications associated with defibrillation threshold testing: the Canadian experience. Heart Rhythm 5:387–390
Grubb BP, Durzinsky D, Brewster P et al (1997) Sudden cerebral vasoconstriction during induced polymorphic ventricular tachycardia and fibrillation: further observations of a paradoxic response. Pacing Clin Electrophysiol 20:1667–1672
Meyer J, Mollhoff T, Seifert T et al (1996) Cardiac output is not affected during intraoperative testing of the automatic implantable cardioverter defibrillator. J Cardiovasc Electrophysiol 7:211–216
Murkin JM, Baird DL, Martzke JS et al (1997) Cognitive dysfunction after ventricular fibrillation during implantable cardiovertor/defibrillator procedures is related to duration of the reperfusion interval. Anesth Analg 84:1186–1192
Conflict of interest
The corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
*The first two authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Licka, M., Jahn, L., Kelemen, K. et al. Is the determination of the defibrillation threshold in patients with an implantable cardioverter–defibrillator still required?. Herzschr. Elektrophys. 22, 209–213 (2011). https://doi.org/10.1007/s00399-011-0150-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-011-0150-1