Abstract
Angiotensin-converting enzyme (ACE) inhibitors are now accepted as part of the routine management of patients with heart failure. Their use has been mandated in all the new major mortality trials to test the efficacy of β-blockers in heart failure. Morbidity and mortality remain high in those with heart failure even with the benefits proven for both these groups of agents.
In spite of the evidence for benefit of ACE inhibitors they are persistently used in lower doses in clinical practice than tested in the large-scale trials. This was so prevalent as to allow the conduct of a substantial study, the ATLAS trial, to compare high and low dose ACE inhibition. Its equivocal findings have allowed different interpretations. Clinical experience would suggest that starting with a low dose is appropriate but the dose should be titrated then without undue delay to the levels used in the trials wherever possible.
The evidence for benefit with these drugs had been obtained largely in patients with impaired systolic function. However the AIRE study selected patients with clinical evidence of heart failure after myocardial infarction rather than with impaired systolic function. A substantial and long-term benefit was found from ACE inhibition. A cohort of patients had ventricular function assessed and as anticipated almost one half had preserved systolic function. Whilst the absolute benefit in lives saved was greater in the higher risk/low ejection fraction group, the relative risk reduction was not significantly different between those with preserved or impaired systolic function. The publication of the HOPE trial, although not a study of patients with heart failure, has clarified the situation considerably for those taking day to day care of patients.
The HOPE study selected patients on the basis of high cardiovascular risk excluding those with known impaired systolic function. Although not an entry requirement for the study, ejection fraction was measured in a substantial majority and was above 40% indicating preservation of systolic function. The ACE inhibitor ramipril markedly reduced the combined end-point of cardiovascular death, stroke and myocardial infarction. Importantly there was a highly significant 20% risk reduction in the rate of myocardial infarction, a prospectively defined end-point, over the average four and a half year follow-up. Taken together with the retrospectively derived evidence from the heart failure trials there is now compelling evidence that the ACE inhibitors prevent myocardial infarction.
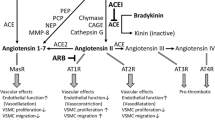
The majority of patients with clinical heart failure have underlying ischaemic heart disease. Prevention of myocardial infarction and control of blood pressure are two key factors in the management of these patients irrespective of systolic ventricular function. The ACE inhibitors like the β-blockers therefore have a pivotal role in their management. A challenge to current clinical trials is to determine whether these properties are shared to the same degree by the angiotensin antagonists or if even further gains in benefit can come from their combination. The neutral findings of the ELITE II study comparing the angiotensin antagonist, losartan, with the ACE inhibitor, captopril, have heightened interest in the on-going trials addressing these issues.
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Smith, W., Ball, S. ACE inhibitors in heart failure: an update. Basic Res Cardiol 95 (Suppl 1), I8–I14 (2000). https://doi.org/10.1007/s003950070003
Issue Date:
DOI: https://doi.org/10.1007/s003950070003