Abstract
Background
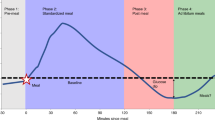
Following consumption of a meal, circulating glucose concentrations can rise and then fall briefly below the basal/fasting concentrations. This phenomenon is known as reactive hypoglycaemia but to date no researcher has explored potential inter-individual differences in response to meal consumption.
Objective
We conducted a secondary analysis of existing data to examine inter-individual variability of reactive hypoglycaemia in response to breakfast consumption.
Methods
Using a replicate crossover design, 12 healthy, physically active men (age: 18–30 y, body mass index: 22.1 to 28.0 kg⋅m− 2) completed two identical control (continued overnight fasting) and two breakfast (444 kcal; 60% carbohydrate, 17% protein, 23% fat) conditions in randomised sequences. Blood glucose and lactate concentrations, serum insulin and non-esterified fatty acid concentrations, whole-body energy expenditure, carbohydrate and fat oxidation rates, and appetite ratings were determined before and 2 h after the interventions. Inter-individual differences were explored using Pearson’s product-moment correlations between the first and second replicates of the fasting-adjusted breakfast response. Within-participant covariate-adjusted linear mixed models and a random-effects meta-analytical approach were used to quantify participant-by-condition interactions.
Results
Breakfast consumption lowered 2-h blood glucose by 0.44 mmol/L (95%CI: 0.76 to 0.12 mmol/L) and serum NEFA concentrations, whilst increasing blood lactate and serum insulin concentrations (all p < 0.01). Large, positive correlations were observed between the first and second replicates of the fasting-adjusted insulin, lactate, hunger, and satisfaction responses to breakfast consumption (all r > 0.5, 90%CI ranged from 0.03 to 0.91). The participant-by-condition interaction response variability (SD) for serum insulin concentration was 11 pmol/L (95%CI: 5 to 16 pmol/L), which was consistent with the τ-statistic from the random-effects meta-analysis (11.7 pmol/L, 95%CI 7.0 to 22.2 pmol/L) whereas effects were unclear for other outcome variables (e.g., τ-statistic value for glucose: 0 mmol/L, 95%CI 0.0 to 0.5 mmol/L).
Conclusions
Despite observing reactive hypoglycaemia at the group level, we were unable to detect any meaningful inter-individual variability of the reactive hypoglycaemia response to breakfast. There was, however, evidence that 2-h insulin responses to breakfast display meaningful inter-individual variability, which may be explained by relative carbohydrate dose ingested and variation in insulin sensitivity of participants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postprandial metabolic responses to a mixed-macronutrient meal typically include a shift from predominantly fat to predominantly carbohydrate metabolism. This shift is reflected by a transient increase in circulating glucose concentrations, caused largely by appearance of ingested carbohydrate [1]. There is also an increase in systemic insulin concentrations which suppresses endogenous glucose production and adipose tissue lipolysis [2], and stimulates peripheral tissue glucose uptake and glycolysis [2]. These responses contribute to buffering the glucose excursion [3], characterised by increased carbohydrate oxidation rates and circulating lactate concentrations, decreased fat oxidation rates, and a return of glucose concentrations to fasting concentrations [3].
In some scenarios, the recovery of circulating glucose concentrations after ingestion of a meal can “overshoot” and “dip” below their basal/fasting concentration before homeostasis is fully restored [4]. This phenomenon is known as reactive hypoglycaemia and is associated with a variety of symptoms including fatigue, light-headiness, sweating and irritability. It has recently been suggested that reactive hypoglycaemia may also be relevant for appetite control [4]. Small correlations (r < 0.3) were observed between a more pronounced reduction in glucose concentrations 2 h after a meal and increased feelings of hunger (r = 0.16, p < 0.001) and the reporting of greater energy intake over the subsequent 24 h (r = 0.27, p < 0.001) [4]. Within-individual analyses revealed a negligible (r < 0.1) association between the day-to-day variation in postprandial glucose reductions at 2–3 h and the day-to-day variation in 24-h reported energy intake (r = 0.06, p < 0.001) [4]. Based on this work, it has been suggested that there may be inter-individual differences in the metabolic response to meals with relevance to appetite control, although the small size of the between-variable correlations combined with the free-living conditions under which participants were testing, make inferences regarding the interindividual heterogeneity of each variable of interest somewhat unclear.
Establishing true inter-individual variability of a measured variable in response to an intervention requires repeated administration of experimental conditions or interventions within the same individuals, with randomisation in the order of exposures to control and intervention [5,6,7]. This approach has been termed a repeated period (replicate) randomised crossover design, which is a form of n-of-1 trial [5,6,7]. N-of-1 trials involve repeated administration of the intervention or control within individuals and there is an example of this design in the context of individual response heterogeneity of antihypertensive drugs [8]. Only with repeated administration of treatment and control conditions can the necessary participant-by-treatment interaction be derived (i.e., the variation between people in the effects of a treatment such as diet). The practical/clinical relevance of treatment response heterogeneity is that, when a true and clinically meaningful participant-by-treatment interaction is identified, then this facilitates rational approaches to personalised treatment. In other words, knowledge about appropriately quantified response heterogeneity provides the rationale to treat individual people differently or with a generalised “cover-all” treatment approach. The use of a replicate crossover design within nutrition research is, to date, rare. In one recent report, the researchers examined the glucose, insulin, and appetite responses to a meal with a replicate crossover design, focussing on the initial 30–60-min postprandial period [9]. It was reported that there was evidence for true inter-individual differences in the responses of peak glucose concentrations and hunger ratings in response to a breakfast [9]. However, since blood sampling finished at 60 min after the meal, it is not known whether reactive hypoglycaemia, which typically occurs between 1 and 3 h postprandially [4, 10], displays true interindividual variability in response to a meal. We previously reported on a study examining the interactive effects of breakfast and exercise on mean changes in postprandial metabolism later in the day. The design of this study was, essentially, a replicate crossover design for the initial 2 h of the study day. Therefore, the aim of this study was to examine whether there was evidence for true inter-individual variability in the metabolic response to a breakfast consumption over a 2-h period. We focused on the 2-h change in glucose as the primary outcome to understand whether there is evidence that reactive hypoglycaemia displays inter-individual response variability. We hypothesised that 2-h glucose concentrations display meaningful inter-individual variability in response to breakfast consumption.
Methods
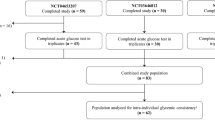
The original study design was a randomised crossover with 4 conditions, fasted prior to rest, fasted prior to exercise, breakfast prior to rest and breakfast prior to exercise and is available open access [10]. Up to the exercise period (and parallel period in control), these conditions provided, essentially, a replicate crossover with two control and two breakfast conditions. The data collected peri-exercise are not included in the present study. Therefore, the conditions are first fasted visit, second fasted visit, first breakfast visit and second breakfast visit. The methods have been reported in detail previously and are described in brief herein. Participants were 12 young, healthy males who provided written informed consent prior to participation. The protocol was approved by the School of Life Sciences Ethics Committee at Northumbria University, and the study was conducted in line with the latest version of the Declaration of Helsinki.
Participants arrived at the laboratories at 0730 in the overnight fasted (10–14 h), rested state for 4 separate study visits, with the condition sequence randomised for each participant (unrestricted randomisation performed using randomizer.org by J.T.G), with at least a 7-day washout. The study was conducted as open label by necessity of meal consumption. Participants were asked to replicate food intake and physical activity for the day before study visits, and asked to avoid alcohol, caffeine, and vigorous activity for 24 h prior to study visits.
Upon arrival at the laboratory, a cannula was inserted into an antecubital vein for repeated blood sampling. A baseline blood sample was taken, alongside a 5-minute measurement of expired gases via indirect calorimetry (Metalyzer 3B, Cortex). Visual analogue scales (VAS, 0–100 mm scale) were then completed to assess ratings of hunger, fullness, satisfaction, and prospective consumption Participants then ingested a test breakfast or remained fasted (water was permitted ad libitum). Further 5-minute breath samples were taken every 30 min after breakfast consumption, and a further blood sample and set of VAS were taken 2 h after breakfast consumption. Participants were familiarised with the visual analogue scales on a preliminary visit prior to the main study days.
Test breakfast
The breakfast comprised 72 g instant oats (Oatso Simple Golden Syrup, Quaker Oats, PepsiCo, UK) and 360 mL semi-skimmed milk (Tesco, UK) which provided 1859 kJ (444 kcal) energy, 67 g carbohydrate, 19 g protein and 11 g fat.
Blood sampling and analysis
10-mL blood samples were collected whilst participants were seated upright to control for postural changes to plasma volume. From the 10-mL blood samples, a 20-µL capillary tube was filled with whole blood to determine blood glucose and lactate concentrations (Biosen C_Line, EKF Diagnostics), and 5 mL allowed to stand for 30 min in a non-anticoagulant tube before being centrifuged at 3000 rpm at 4 °C for 10 min. Aliquots of serum were then stored for later determination of NEFA (WAKO Diagnostics) and insulin (DIAsource ImmunoAssays S.A.) concentrations in duplicate. All serum samples were stored at − 80 °C. The intra-assay CV were 5.6 and 7.2% for NEFA and insulin, respectively. Inter-assay CV were 8.1 and 3.6 for NEFA and insulin, respectively. To reduce the inter-assay variation, samples from each participant were analysed during the same run where possible.
Breath sampling and analysis
Expired gas samples were collected using an online gas analysis system (Metalyzer 3B, Cortex) calibrated using gases of known concentrations and a 3-L syringe. Participants wore a facemask and after a 2-min stabilisation phase, 5-min samples were obtained and averaged. Carbohydrate and fat oxidation rates were calculated assuming negligible protein oxidation, using stoichiometric equations [11]. Since the baseline sampling was not in accordance with best practice measures for resting metabolic rate [12] and could thereby introduce additional error into the postprandial change measures, the data for energy expenditure, carbohydrate oxidation and fat oxidation are not adjusted for baseline.
Statistical analysis
Although the sample size for the present study has been set a priori by the previous study (for detection of mean treatment effects), we can estimate minimal detectable effect sizes that are relevant to response heterogeneity for our sample size of 12 participants. In terms of the between-replicate correlation coefficient (see below), 12 participants would translate to a between-replicate correlation of 0.5 as being statistically significant (one-tailed P = 0.049). The 90% confidence interval for this correlation would be 0.00 to 0.80. A directional (one-tailed) hypothesis is relevant in this context because both a zero and a negative correlation would mean non-rejection of the null hypothesis (r ≤ 0). Adjustment for multiple comparisons due to secondary outcomes was not undertaken on the basis that if secondary outcomes are interpreted precisely and exclusively, then the per-comparison-wise error rate is not increased [13].
The analysis framework in the present study involved a four-step approach consistent with previous research adopting similar designs and methodological standards for the analysis of replicate crossover trials [9, 14,15,16]:
-
1)
The association between the first and second replicate of the control-adjusted individual treatment effects was quantified for each outcome using Pearson’s product-moment correlation coefficients. Pearson’s correlation was selected over an intraclass correlation coefficient because the latter statistic traditionally pools systematic bias (in our case, the mean treatment effect) and random individual variability together, which would mask appropriate quantification of the individual consistency in response. The first breakfast condition in any participant’s sequence was paired to the first control condition in the same individual’s sequence. Thresholds of 0.1, 0.3 and 0.5 were used to infer correlations as small, moderate, and large, respectively [17]. This correlation coefficient quantifies the consistency of the breakfast effect across the replicated experimental conditions.
-
2)
The SD of the of the breakfast condition was adjusted for the SD of the control condition to provide an overall estimate of the true between-participant differences in treatment response using the following equation:
Where SDIR represents the true interindividual variation in treatment effect. SDBreakfast and SDControl are the SDs of the pre-to-post change scores for the breakfast and fasting control conditions (averaged over the 2 replicates using the relevant equation for pooling SDs [18]. This SD is a naïve estimation of individual response variability adjusted for any random trial-to-trial variability (quantified using the comparator condition data).
-
3)
Whilst Eq. 1 estimates response variance adjusted for the change variance in the control condition, the associated SEs and CIs are not appropriate for a within-participant crossover study design. Therefore, we also performed a within-participant linear mixed model. Using the MIXED procedure in SAS OnDemand for Academics (SAS Institute), a within-participant linear mixed model was formulated to quantify participant-by-condition interaction for each outcome [19]. Each included condition and period (sequence), and their interaction, were modelled as fixed effects with participant plus participant-by-condition interaction term modelled as random effects (refer to the SAS code supplied in Supplemental Methods). Standard residual diagnostics were undertaken to assess the “influence diagnostics” of a potential set of observations on the adequacy and the stability of the modelled covariance parameter estimates [20,21,22]. These analyses were also performed for circulating metabolite and insulin concentrations with and without baseline adjustment to explore the effect of baseline adjustment in analyses of response heterogeneity.
-
4)
Using the approach recently reported by Senn [16], we calculated the replicate-averaged treatment effect for each participant along with the respective 95% confidence intervals (CI). A sample estimate of within-subjects variance is calculated and converted to a standard error using appropriate degrees of freedom given the completed cycles to derive per participant replicate-averaged treatment effects [16]. A random-effects meta-analysis approach summarised each individual-participant replicate-averaged treatment effect and respective standard errors of the mean effect (SE) using the metagen() function available in the meta package [16, 23]. The tau-statistic (τ) value described the between-participant variability across the distribution of true replicate-averaged treatment effects [24, 25]. The restricted maximum-likelihood estimation method determined the mean τ-statistic value with uncertainty surrounding the point estimate described as 95%CI derived using the generalised Q-statistic method [26]. Weighted raw mean replicate-averaged treatment effect differences were reported as descriptive statistics with the 95% prediction interval (95% PI) describing the expected range for the distribution of true mean differences for 95% of similar future studies [27, 28]. Meta-analyses were conducted in R (version 3.6.3, R Foundation for Statistical Computing).
Existing literature and information in this field informed minimal clinically important differences (MCID; ∆) definitions [29]. A target difference in glucose concentrations of ∆=±0.5 mmol/L on the basis that this is the smallest difference shown to be associated with mortality [30]. A target difference in insulin concentrations of ∆=±6 pmol/L as the smallest difference shown to have a meaningful effect on non-esterified fatty acid (NEFA) turnover rates [2]. A target difference in NEFA concentrations of ∆=±0.29 mmol/L as the smallest difference shown to affect skeletal muscle insulin signalling [31]. A target difference in lactate concentrations of ∆=±0.5 mmol/L on the basis that this is the typical rise seen after a mixed-macronutrient meal [32], and is also the target difference used as a threshold in exercise testing [33]. For appetite ratings a ∆=±5 mm was selected as the target difference as suggested by authors in the field [34].
Pearson’s product-moment correlation coefficients were quantified between the pooled mean control-adjusted meal response for the change in glucose and the pooled mean control-adjusted response for all other outcomes to assess whether reactive hypoglycaemia was associated with responses of other metabolites or hormones, or appetite ratings. Finally, to explore whether participant characteristics were associated with postprandial responses, Pearson’s product-moment correlation coefficients were quantified between the participant age, height, body mass and body mass index, and the pooled mean control-adjusted response for all other outcomes.
Results
Participant characteristics
Participant characteristics have been reported previously and are reproduced in Table 1.
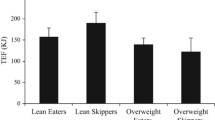
Circulating metabolites and insulin
When taking the average of both breakfast trials and both fasting trials, there was evidence of reactive hypoglycaemia at the group level, as the 2-h change in glucose concentrations demonstrated a greater decline following breakfast than with compared with continued overnight fasting p < 0.01, Table 2). A negligible correlation was observed between the 2 replicates of fasting-adjusted 2-h postprandial glucose responses (r < -0.001, 90%CI: -0.52 to 0.52, p = 0.50, Fig. 1A). Both estimates of the individual differences SD were below the MCID of ± 0.50 mmol/L and the p value for the participant-by-condition interaction was above the threshold for statistical significance (Table 2; Fig. 2A). Analysis without adjustment for baseline values did not change this inference (participant-by-condition interaction, p = 0.35).
Correlation between the replicates of the baseline-to-two-h response to breakfast minus the fasting control condition, for blood glucose (A), serum insulin (B), blood lactate (C), and serum NEFA concentrations (D). “Response 1” corresponds to the first pair of conditions (breakfast 1 minus control 1) and “Response 2” to the second pair of conditions (breakfast 2 minus control 2). Each data point is an individual participant. The dotted lines represent the MCID and the solid lines represent the group mean. n = 11. MCID, minimal clinically important difference. NEFA, non-esterified fatty acid
Results of the meta-analysis of each participants treatment effect estimate for blood glucose (A), serum insulin (B), blood lactate (C), and serum NEFA concentrations (D) two h after consumption of breakfast (BREAKFAST) relative to two h after remaining in the overnight fasted state (FASTED). n = 11. NEFA, non-esterified fatty acid
In contrast to glucose, the group mean 2-h change in insulin concentrations was higher with breakfast compared with fasting (p < 0.01, Table 2). A large positive correlation of 0.74 (90%CI: 0.35 to 0.91, p < 0.01, Fig. 1B) was observed between the 2 replicates of fasting-adjusted 2-h postprandial insulin responses. The within-trial SD for insulin was substantially greater during the breakfast trial than the fasting trial, with both estimates of the individual differences SD approximately 2-fold larger than the MCID of ± 6 pmol/L plus a statistically significant participant-by-condition interaction (Table 2; Fig. 2B). Analysis without adjustment for baseline values did not change this inference (participant-by-condition interaction, p = 0.02).
At the group mean level, the 2-h change in lactate concentrations was higher with breakfast compared with fasting (p < 0.01, Table 2). A large positive correlation of 0.68 (90%CI: 0.24 to 0.89, p = 0.01, Fig. 1C) was observed between the 2 replicates of fasting-adjusted 2-h postprandial lactate responses. However, the within-trial SD for lactate was not substantially greater during the breakfast trial than the fasting trial, with both estimates of the individual differences SD below the MCID of ± 0.50 mmol/L and a trivial the participant-by-condition interaction (Table 2; Fig. 2C). Analysis without adjustment for baseline values did not change this inference (participant-by-condition interaction, p = 0.28).
At the group mean level, the 2-h change in NEFA concentrations showed a greater decline following breakfast than with extended fasting (p < 0.01; Table 2). A moderate positive correlation of 0.48 (90%CI: -0.05 to 0.80, p = 0.07, Fig. 1D) was observed between the 2 replicates of fasting-adjusted 2-h postprandial NEFA responses. Both estimates of the individual differences SD were below the MCID of ± 0.29 mmol/L, with a trivial effect for the participant-by-condition interaction (Table 2; Fig. 2D). Analysis without adjustment for baseline values did not change this inference (participant-by-condition interaction, p = 0.45).
Energy expenditure and substrate oxidation
Whole-body energy expenditure and carbohydrate oxidation were both higher following breakfast consumption than extended overnight fasting (Table 1, p < 0.01 and < 0.0001, respectively), whereas fat oxidation was lower with breakfast consumption than extended overnight fasting (p < 0.01; Table 2). A small positive correlation was observed between the 2 replicates of fasting-adjusted 2-h postprandial energy expenditure (r = 0.18, 90%CI: -0.35 to 0.62, p = 0.29; Fig. 3A) moderate positive correlation for carbohydrate oxidation (r = 0.44, 90%CI: -0.08 to 0.77, p = 0.08, Fig. 3B) and negligible correlation for fat oxidation responses (r = 0.07, 90%CI: -0.45 to 0.55, p = 0.42, Fig. 3C). The within-trial SD for energy expenditure, carbohydrate and fat oxidation rates were not substantially greater during the breakfast trial than the fasting trial, with trivial effects for the participant-by-condition interaction terms (Table 2; Fig. 4A, B and C).
Correlation between the replicates of the baseline-to-two-h response to breakfast minus the fasting control condition, for whole-body energy expenditure (A), carbohydrate oxidation (B), and fat oxidation (C). “Response 1” corresponds to the first pair of conditions (breakfast 1 minus fasting 1) and “Response 2” to the second pair of conditions (breakfast 2 minus fasting 2). Each data point is an individual participant. The dotted lines represent the MCID and the solid lines represent the group mean. n = 12. MCID, minimal clinically important difference
Results of the meta-analysis of each participants treatment effect estimate for whole-body energy expenditure (A), carbohydrate oxidation (B), and fat oxidation rates (C) two h after consumption of breakfast (BREAKFAST) relative to two h after remaining in the overnight fasted state (FASTED). n = 12
Appetite ratings
The 2-h change in ratings of hunger and prospective consumption were both lower following breakfast consumption than extended overnight fasting (p < 0.01 and < 0.001, respectively; Table 2), whereas ratings of fullness and satisfaction were both higher following breakfast consumption than extended overnight fasting (p < 0.001 and < 0.01, respectively; Table 2).
A large positive correlation was observed between the 2 replicates of fasting-adjusted 2-h change in hunger (r = 0.52, 90%CI: 0.03 to 0.81, p = 0.04; Fig. 5A). The within-trial SD for hunger was not substantially greater during the breakfast trial than the fasting trial, with a trivial effect for the participant-by-condition interaction (Table 2; Fig. 6A).
Correlation between the replicates of the baseline-to-two-h response to breakfast minus the fasting control condition, for hunger (A), prospective consumption (B), fullness (C), and satisfaction ratings. “Response 1” corresponds to the first pair of conditions (breakfast 1 minus fasting 1) and “Response 2” to the second pair of conditions (breakfast 2 minus fasting 2). Each data point is an individual participant. The dotted lines represent the MCID and the solid lines represent the group mean. n = 12. MCID, minimal clinically important difference
A small negative positive correlation was observed between the 2 replicates of fasting-adjusted 2-h change in prospective consumption (r = -0.29, 90%CI: -0.69 to 0.24, p = 0.18; Fig. 5B). The within-trial SD for hunger was not substantially greater during the breakfast trial than the fasting trial, with a trivial effect for the participant-by-condition interaction (Table 2; Fig. 6B).
A negligible correlation was observed between the 2 replicates of fasting-adjusted 2-h change in fullness (r = 0.04, 90%CI: -0.47 to 0.53, p = 0.45; Fig. 5C). The within-trial SD for fullness was not substantially greater during the breakfast trial than the fasting trial, and the p value for the participant-by-condition interaction was above the threshold for statistical significance (Table 2; Fig. 6C).
A large positive correlation was observed between the 2 replicates of fasting-adjusted 2-h change in satisfaction (r = 0.53, 90%CI: 0.04 to 0.81, p = 0.04; Fig. 5D). The within-trial SD for hunger was not substantial greater during the breakfast trial than the fasting trial, and the p value for the participant-by-condition interaction was above the threshold for statistical significance (Table 2; Fig. 6D).
Correlations between glucose responses, participant characteristics and other outcomes
Moderate, positive correlations were observed between the pooled, fasting-adjusted glucose response and the pooled, fasting-adjusted insulin (r = 0.47, 95%CI: -0.18 to 0.83, p = 0.15), lactate (r = 0.32, 95%CI: -0.34 to 0.77, p = 0.33) and NEFA responses (r = 0.40, 95%CI: -0.27 to 0.80, p = 0.23). A small, positive correlation was observed between the pooled, fasting-adjusted glucose response and the pooled, fasting-adjusted fullness response (r = 0.25, 95%CI: -0.41 to 0.74, p = 0.46), whereas correlations between the pooled, fasting-adjusted glucose response and the pooled, fasting-adjusted hunger (r = -0.07, 95%CI: -0.64 to 0.56, p = 0.85), satisfaction (r = 0.06, 95%CI: -0.56 to 0.63, p = 0.87), and prospective consumption responses (r = -0.16, 95%CI: -0.69 to 0.48, p = 0.63) were small-to-negligible. A large, negative correlation was observed between body mass and the pooled, fasting-adjusted lactate response (r = -0.59, 95%CI: -0.88 to 0.01, p = 0.06), whereas the correlation between body mass and the pooled, fasting-adjusted insulin response was moderate and negative (r = -0.37, 95%CI: -0.80 to 0.29, p = 0.26).
Discussion
The present investigation provides evidence of reactive hypoglycaemia 2 h following breakfast consumption at the group (mean response) level, but with undetectable meaningful inter-individual variability. The only postprandial outcome to display meaningful inter-individual variability in response to breakfast consumption was serum insulin concentrations. These data, therefore, do not support the concept that people respond differently to one another with respect to blood glucose “dips” after a breakfast meal, nor that this translates into individual differences in appetite responses. Rather, that individual differences in the insulin response to the breakfast regulate blood glucose concentrations within a range.
Reactive hypoglycaemia in the postprandial state (sometimes referred to as glucose dips) typically occurs 2–3 h after a meal and is thought to be primarily due to insulin-stimulated peripheral glucose uptake superseding the increase in exogenous (meal-derived) glucose appearance rates [35]. Whilst sampling from compartments that drain insulin sensitive tissues (e.g., mixed or deep venous blood, and interstitial fluid) is likely to over diagnose reactive hypoglycaemia compared to arterial, capillary or arterialised blood [36], reactive hypoglycaemia is still observed with arterialised sampling [35] and the phenomenon is therefore not simply an artefact of blood sampling site. It has been suggested that reactive hypoglycaemia displays interindividual variability and contributes to appetite regulation on the basis of correlations between and within individuals [4]. The current study is the first to employ a replicate crossover design with postprandial glucose sampling over a timeframe relevant for capturing reactive hypoglycaemia. The replicate crossover design allows for quantification of the participant-by-condition interaction and thus allows inferences to be drawn about true inter-individual heterogeneity of responses to an intervention [7]. The data in the current study do no provide evidence of meaningful inter-individual heterogeneity of the 2-h glucose response to breakfast consumption when accounting for the control condition of extended overnight fasting. Nor do the data provide evidence for meaningful inter-individual heterogeneity for 2-h lactate or NEFA concentrations, energy expenditure, substrate metabolism, or appetite ratings. The only outcome to show meaningful inter-individual heterogeneity of response to breakfast consumption was serum insulin concentrations.
Insulin is the primary hormone controlling the shift in substrate metabolism from the fasted to the postprandial state. Insulin controls glucose concentrations primarily by suppressing endogenous glucose production and stimulating peripheral tissue glucose uptake. The availability of circulating insulin is dependent on insulin secretion and hepatic insulin extraction. The former of which is stimulated by circulating glucose concentrations and potentiated by the incretin hormones. When the size and composition of the meal is fixed across participants, as is the case in the current study, then the relative macronutrient load differs. Smaller individuals will receive a larger relative proportion of nutrients and thus, all else being equal, would receive a larger signal for insulin secretion. Consistent with this, we observed a negative relationship between body mass and the 2-h insulin response adjusted for the fasting condition. Consequently, it is likely that the interindividual heterogeneity in the insulin response to breakfast resulted in regulatory control of glucose concentrations, such that meaningful interindividual heterogeneity for glucose concentrations were not observed. This principle can also be demonstrated by observations that within-individuals, doubling energy intake increases postprandial insulin concentrations without significantly increasing postprandial glucose concentrations [37].
The postprandial circulating lactate concentrations in response to a meal are the net result of changes in the uptake and release of lactate from tissues. Insulin-stimulated glycolysis can increase lactate production in splanchnic and peripheral tissues [38,39,40], and the inclusion of specific monosaccharides within a meal, such as fructose and galactose, may further increase lactate concentrations due to their interconversion by the liver and splanchnic bed [32, 41,42,43]. Accordingly, it might be expected that lactate concentrations display inter-individual variability in response to a fixed size meal due to differences in insulin-stimulated peripheral glycolysis and relative availability of lactate precursors. Whilst we observed a large positive correlation between the fasting-adjusted first and second lactate responses to breakfast consumption, the response variance estimates did not exceed the pre-defined target MCID, with a trivial effect for the participant-by-condition interaction. This may be explained by consistent within-individual responses but relatively low absolute concentrations and between-individual heterogeneity, combined with a relatively small sample size. Since the majority of the hydrolysed carbohydrate in the meal would be glucose (~ 52 g glucose, ~ 9 g galactose and ~ 6 g fructose), the increase in blood lactate concentrations at 2 h is likely to be primarily due to stimulation of glycolysis [38] rather than hepatic interconversion of metabolites. If the galactose and/or fructose content of the meal was higher, there is likely to have been higher absolute lactate concentrations [32, 41]. It is therefore possible that a meal high in fructose and galactose containing sugars may produce greater evidence of inter-individual heterogeneity of the lactate response. The current inferences for inter-individual variability of postprandial lactate responses relate to mixed-macronutrient meals with a modest sugar content.
Postprandial increases in carbohydrate metabolism are mirrored by changes in fat metabolism, including decreased circulating NEFA concentrations from inhibition of net adipose tissue lipolysis. Consistent with this, we observed a mean reduction in 2-h NEFA concentrations with breakfast consumption compared with the fasting control. Whilst we observed a moderate positive correlation between the fasting-adjusted first and second NEFA responses to breakfast consumption, the response variance did not exceed the pre-defined target MCID, with a trivial effect for the participant-by-condition interaction. This is possibly due to two reasons. First, like glucose concentrations, the variance in insulin response results in a controlled suppression of lipolysis to achieve a similar NEFA concentration. Second, suppression of adipose tissue lipolysis is highly sensitive to insulin such that in most postprandial situations adipose tissue lipolysis is maximally suppressed [2, 44], thereby resulting a “floor” effect.
Changes in circulating metabolite and hormone concentrations can be both cause and effect of changes in whole-body substrate metabolism. In the postprandial state, whole-body energy expenditure and carbohydrate oxidation is increased, whereas fat oxidation is decreased. Consistent with this we observed mean increases in energy expenditure and carbohydrate oxidation rates and decreases in fat oxidation rates with breakfast consumption compared with fasting. However, we did not find evidence for true interindividual variability in whole-body energy expenditure or substrate metabolism responses to breakfast consumption. It is possible that measurement error is too large to detect such differences with the current sample size, and/or the lack of baseline measure contributes to observing observations of interindividual variance.
Reactive hypoglycaemia has been shown to correlate with appetite ratings and self-reported energy intake [4]. Accordingly, we also examined the interindividual heterogeneity of the appetite responses to a meal. We observed large positive correlations between the fasting-adjusted first and second hunger and satisfaction responses to breakfast consumption, whereas the equivalent correlations for prospective consumption and fullness were negligible or negative. Furthermore, the additional estimate on interindividual response did not provide evidence for meaningful inter-individual heterogeneity of any of the appetite ratings in response to breakfast consumption. To the best of the authors knowledge, only one other study has examined inter-individual heterogeneity of appetite responses to a meal adopting a replicate crossover design [9]. The prior study provided evidence of meaningful inter-individual heterogeneity of appetite ratings 1-h after consumption of a 1200 kcal breakfast (i.e., estimated SDs for all ratings above 10 mm and significant participant-by-condition interaction). The current study provided a breakfast with less than half the energy content, with appetite ratings determined at the 2-h timepoint. It is, therefore, possible that inter-individual heterogeneity of appetite responses to a meal are dependent on the absolute meal size and the timeframe of measurement. To examine whether reactive hypoglycaemia was associated with appetite ratings, we explored correlations between the pooled, fasting-adjusted glucose responses to breakfast, and the pooled, fasting-adjusted responses for each of the appetite ratings. We found no evidence that reactive hypoglycaemia was associated with meaningful increases in appetite.
The present study sample size and the standard absolute portion size of the meal provided constitute aspects that deserve consideration. This designed experiment is limited by the relatively small sample size, which, however, also reflects the onerous nature of the replicate crossover trial per se that requires rigorous standardization, replicated dietary protocols, and different outcome measure assessments [15, 45]. Nevertheless, it is important to highlight that the fundamental nature of a replicate crossover trial, that aims to separate pragmatically sources of random participant-by-condition interaction variance from within-participant trial-to-trial variability via the repeated assessment of the same participants, maximizes study costs in a way that reduces the recruitment pool [45]. Accordingly, our analysis outcomes suggested the number of trial replicates was suitable enough for a reasonably precise estimation of each primary outcome measure participant-by-condition interaction variance components (Table 2). The ability to detect inter-individual heterogeneity for insulin could be, in part, due to a lower day-to-day variability in insulinaemia, yet the day-to-day variability reported for insulin concentrations (~ 0.7%) is only marginally lower than that of glucose (1.1%), lactate (1.5%) or NEFA (1.1%) [46]. The current study estimates based on meta-analysis and SAS modelling outcomes provide the basis to design more replicate crossover studies with differing meal compositions, to assess whether the is low-to-moderate inter-individual heterogeneity of lactate, NEFA and appetite responses to breakfast. Whether any inter-individual heterogeneity of the insulin response to a meal is still evident when meal size is scaled to body size therefore requires further investigation, and requires consideration of how to scale (e.g., for body mass, resting metabolic rate, total energy requirements, fat-free mass, splanchnic and/or skeletal muscle mass). Partly due to these decisions, and also because in practice instant oats are provided in absolute portion sizes, we chose an absolute portion size for the current investigation. This was deemed the most efficient approach, since if there was no evidence for interindividual heterogeneity of response to a fixed size breakfast, then it is unlikely that there would be meaningful interindividual heterogeneity when scaling the breakfast to body size.
To conclude, we were unable to detect any meaningful interindividual heterogeneity of the reactive hypoglycaemia response to breakfast, despite the observation of reactive hypoglycaemia at the group mean level, 2 h after breakfast consumption. We did, however, observe meaningful inter-individual heterogeneity of the 2-h insulin response to breakfast which may partly be explained by differences in body mass and thus relative carbohydrate dose ingested, combined with variance in insulin sensitivity. Whether there is clinically meaningful heterogeneity of the 2-h lactate, NEFA and appetite responses to breakfast require further work, which would benefit from a larger sample size and may depend on the composition of the meal.
References
Edinburgh RM, Hengist A, Smith HA, Travers RL, Koumanov F, Betts JA, Thompson D, Walhin JP, Wallis GA, Hamilton DL et al (2018) Preexercise breakfast ingestion versus extended overnight fasting increases postprandial glucose flux after exercise in healthy men. Am J Physiol - Endocrinol Metabolism 315(5):E1062–E74. https://doi.org/10.1152/ajpendo.00163.2018
Groop LC, Bonadonna RC, DelPrato S, Ratheiser K, Zyck K, Ferrannini E, DeFronzo RA (1989) Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus. Evidence for multiple sites of insulin resistance. J Clin Investig 84(1):205–213
Taylor R, Magnusson I, Rothman DL, Cline GW, Caumo A, Cobelli C, Shulman GI (1996) Direct assessment of liver glycogen storage by 13 C nuclear magnetic resonance spectroscopy and regulation of glucose homeostasis after a mixed meal in normal subjects. J Clin Investig 97(1):126–132
Wyatt P, Berry SE, Finlayson G, O’Driscoll R, Hadjigeorgiou G, Drew DA, Khatib HA, Nguyen LH, Linenberg I, Chan AT (2021) Postprandial glycaemic dips predict appetite and energy intake in healthy individuals. Nat Metabolism 3(4):523–529
Senn S (2016) Mastering variation: variance components and personalised medicine. Stat Med 35(7):966–977. https://doi.org/10.1002/sim.6739
Senn S (2018) Statistical pitfalls of personalized medicine. Nature 563(7733):619–621. https://doi.org/10.1038/d41586-018-07535-2
Senn S, Rolfe K, Julious SA (2011) Investigating variability in patient response to treatment–a case study from a replicate cross-over study. Stat Methods Med Res 20(6):657–666. https://doi.org/10.1177/0962280210379174
Sundstrom J, Lind L, Nowrouzi S, Hagstrom E, Held C, Lytsy P, Neal B, Marttala K, Ostlund O (2023) Heterogeneity in blood pressure response to 4 antihypertensive drugs: a Randomized Clinical Trial. JAMA 329(14):1160–1169. https://doi.org/10.1001/jama.2023.3322
Goltz FR, Thackray AE, Atkinson G, Lolli L, King JA, Dorling JL, Dowejko M, Mastana S, Stensel DJ (2019) True interindividual variability exists in postprandial appetite responses in healthy men but is not moderated by the FTO Genotype. J Nutr 149(7):1159–1169. https://doi.org/10.1093/jn/nxz062
Gonzalez JT, Veasey RC, Rumbold PL, Stevenson EJ (2013) Breakfast and exercise contingently affect postprandial metabolism and energy balance in physically active males. Brit J Nutr 110(4):721–732
Frayn KN (1983) Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiology: Respiratory Environ Exerc Physiol 55(2):628–634
Compher C, Frankenfield D, Keim N, Roth-Yousey L, Evidence Analysis Working G (2006) Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc 106(6):881–903. https://doi.org/10.1016/j.jada.2006.02.009
Parker RA, Weir CJ (2022) Multiple secondary outcome analyses: precise interpretation is important. Trials 23(1):27
Goltz FR, Thackray AE, King JA, Dorling JL, Atkinson G, Stensel DJ (2018) Interindividual responses of appetite to Acute Exercise: a replicated crossover study. Med Sci Sports Exerc 50(4):758–768. https://doi.org/10.1249/MSS.0000000000001504
Shen T, Thackray AE, King JA, Alotaibi TF, Alanazi TM, Willis SA, Roberts MJ, Lolli L, Atkinson G, Stensel DJ (2024) Are there interindividual responses of Cardiovascular Disease risk markers to Acute Exercise? A replicate crossover trial. Med Sci Sports Exerc 56(1):63–72
Senn S (2024) The analysis of continuous data from n-of-1 trials using paired cycles: a simple tutorial. Trials 25(1):128
J. C. Statistical power analysis for the behavioural sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates, (1988)
Higgins JPT, Green S Internet: http://handbook-5-1.cochrane.org
Academics SOf Internet: https://www.sas.com/en_us/software/on-demand-for-academics.html
West BT, Galecki AT (2011) An overview of current software procedures for fitting linear mixed models. Am Stat 65(4):274–282
Oman SD (1995) Checking the assumptions in mixed-model analysis of variance: a residual analysis approach. Comput Stat Data Anal 20(3):309–330
Schabenberger O (2004) Mixed model influence diagnostics. Proceedings of the twenty-ninth annual SAS Users Group International Conference. Cary (NC): SAS Institute, :189 – 29
Schwarzer G (2007) meta: an R package for meta-analysis. R news 7:40–45
Langan D, Higgins JP, Jackson D, Bowden J, Veroniki AA, Kontopantelis E, Viechtbauer W, Simmonds M (2019) A comparison of heterogeneity variance estimators in simulated random-effects meta‐analyses. Res Synthesis Methods 10(1):83–98
Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, Kuss O, Higgins JP, Langan D, Salanti G (2016) Methods to estimate the between-study variance and its uncertainty in meta‐analysis. Res Synthesis Methods 7(1):55–79
Viechtbauer W (2007) Confidence intervals for the amount of heterogeneity in meta-analysis. Stat Med 26(1):37–52
Borenstein M, Hedges LV, Higgins JP, Rothstein HR (2010) A basic introduction to fixed-effect and random‐effects models for meta‐analysis. Res Synthesis Methods 1(2):97–111
Borenstein M (2023) Avoiding common mistakes in meta-analysis: understanding the distinct roles of Q, I‐squared, tau‐squared, and the prediction interval in reporting heterogeneity. Research Synthesis Methods
Cook JA, Julious SA, Sones W, Hampson LV, Hewitt C, Berlin JA, Ashby D, Emsley R, Fergusson DA, Walters SJ DELTA2 guidance on choosing the target difference and undertaking and reporting the sample size calculation for a randomised controlled trial. bmj 2018;363.
Collaboration ERF (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364(9):829–841
Belfort R, Mandarino L, Kashyap S, Wirfel K, Pratipanawatr T, Berria R, DeFronzo RA, Cusi K (2005) Dose-response effect of elevated plasma free fatty acid on insulin signaling. Diabetes 54(6):1640–1648
Hengist A, Davies RG, Rogers PJ, Brunstrom JM, van Loon LJ, Walhin J-P, Thompson D, Koumanov F, Betts JA, Gonzalez JT Restricting sugar or carbohydrate intake does not impact physical activity level or energy intake over 24 h despite changes in substrate use: a randomised crossover study in healthy men and women. Eur J Nutr 2022:1–20
Jamnick NA, Botella J, Pyne DB, Bishop DJ (2018) Manipulating graded exercise test variables affects the validity of the lactate threshold and V˙ O 2 peak. PLoS ONE 13(7):e0199794
Flint A, Raben A, Blundell J, Astrup A (2000) Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes 24(1):38–48
Leonetti F, Foniciello M, Iozzo P, Riggio O, Merli M, Giovannetti P, Sbraccia P, Giaccari A, Tamburrano G (1996) Increased nonoxidative glucose metabolism in idiopathic reactive hypoglycemia. Metabolism 45(5):606–610
Edinburgh RM, Hengist A, Smith HA, Betts JA, Thompson D, Walhin JP, Gonzalez JT (2017) Prior exercise alters the difference between arterialised and venous glycaemia: implications for blood sampling procedures. Br J Nutr 117(10):1414–1421. https://doi.org/10.1017/S0007114517001362
Hengist A, Edinburgh RM, Davies RG, Walhin J-P, Buniam J, James LJ, Rogers PJ, Gonzalez JT, Betts JA (2020) Physiological responses to maximal eating in men. Brit J Nutr 124(4):407–417
Jackson R, Hamling J, Sim B, Hawa M, Blix P, Nabarro J (1987) Peripheral lactate and oxygen metabolism in man: the influence of oral glucose loading. Metabolism 36(2):144–150
Moore MC, Smith MS, Farmer B, Coate KC, Kraft G, Shiota M, Williams PE, Cherrington AD (2018) Morning hyperinsulinemia primes the liver for glucose uptake and glycogen storage later in the day. Diabetes 67(7):1237–1245
Moore MC, Smith MS, Farmer B, Kraft G, Shiota M, Williams PE, Cherrington AD (2017) Priming effect of a morning meal on hepatic glucose disposition later in the day. Diabetes 66(5):1136–1145
Watkins J, Simpson A, Betts JA, Thompson D, Holliday A, Deighton K, Gonzalez JT (2020) Galactose ingested with a high-fat beverage increases postprandial lipemia compared with glucose but not fructose ingestion in healthy men. J Nutr 150(7):1765–1772
Jang C, Wada S, Yang S, Gosis B, Zeng X, Zhang Z, Shen Y, Lee G, Arany Z, Rabinowitz JD (2020) The small intestine shields the liver from fructose-induced steatosis. Nat Metabolism 2(7):586–593
Theytaz F, De Giorgi S, Hodson L, Stefanoni N, Rey V, Schneiter P, Giusti V, Tappy L (2014) Metabolic fate of fructose ingested with and without glucose in a mixed meal. Nutrients 6(7):2632–2649
Enevoldsen L, Simonsen L, Macdonald I, Bülow J (2004) The combined effects of exercise and food intake on adipose tissue and splanchnic metabolism. J Physiol 561(3):871–882
Senn S (2019) Sample size considerations for n-of-1 trials. Stat Methods Med Res 28(2):372–383
Widjaja A, Morris RJ, Levy JC, Frayn KN, Manley SE, Turner RC (1999) Within-and between-subject variation in commonly measured anthropometric and biochemical variables. Clin Chem 45(4):561–566
Funding
The current manuscript was prepared without external funding. For a full list of JTG’s disclosures see https://gonzalezjt1.wordpress.com/2024/03/, JTG has received research funding from BBSRC, MRC, British Heart Foundation, Clasado Biosciences, Lucozade Ribena Suntory, ARLA Foods Ingredients and Cosun Nutrition Center; is a scientific advisory board member to ZOE and 6d Sports Nutrition; and has completed paid consultancy for The Dairy Council, PepsiCo, Violicom Medical, Tour Racing Ltd., the European Fruit Juice Association, and SVGC. JAB is an investigator on research grants funded by BBSRC, MRC, British Heart Foundation, Rare Disease Foundation, EU Hydration Institute, GlaxoSmithKline, Nestlé, Lucozade Ribena Suntory, ARLA foods, Cosun Nutrition Center, American Academy of Sleep Medicine Foundation and Salus Optima (L3M Technologies Ltd); has completed paid consultancy for PepsiCo, Kellogg’s, SVGC and Salus Optima (L3M Technologies Ltd); is Company Director of Metabolic Solutions Ltd; receives an annual honorarium as a member of the academic advisory board for the International Olympic Committee Diploma in Sports Nutrition; and receives an annual stipend as Editor-in Chief of International Journal of Sport Nutrition & Exercise Metabolism.
Author information
Authors and Affiliations
Contributions
JTG, RCV, PLSR and EJS conceived and designed the research. JTG, LL and GA analysed the data, JTG, LL, JAB and GA interpreted the results, JTG, LL and GA drafted the figures and initial manuscript. All authors reviewed and revised the manuscript. All authors approved the final manuscript.
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gonzalez, J.T., Lolli, L., Veasey, R.C. et al. Are there interindividual differences in the reactive hypoglycaemia response to breakfast? A replicate crossover trial. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03467-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03467-y