Abstract
Purpose
Combining different statistical methods to identify dietary patterns (DP) may provide new insights on how diet is associated with adiposity. This study investigated the association of DP derived from three data-driven methods and adiposity indicators over time.
Methods
This study used data from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). DP were identified at baseline applying three statistical methods: Factor Analysis (FA), Treelet Transform (TT), and Reduced Rank Regression (RRR). The association between DP and adiposity indicators (weight, body mass index, waist circumference, body fat percentage and fat mass index) over the period of 8.2 years of follow-up was assessed by linear mixed-models.
Results
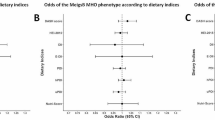
Convenience DP, marked by unhealthy food groups, was associated with higher adiposity over the follow-up period, regardless of the method applied. The DP identified by TT and marked by high consumption of rice and beans was associated with lower adiposity, whereas the similar DP identified by FA, but additionally characterised by consumption of poultry and red meat was associated with higher adiposity. Prudent DP, marked by plant-based food groups and fish, identified by FA was associated with lower adiposity across the median follow-up time.
Conclusion
Applying different methods to identify DP showed that a convenience DP was associated with higher adiposity independent of the method applied. We also identified the nuances within adherence to a Brazilian traditional dietary pattern characterised by the consumption of rice and beans, that only when combined with reduced consumption of animal protein and unhealthy foods was associated with lower adiposity over time.

Similar content being viewed by others
References
Global Burden of Disease Collaborative Network (2017) Global Burden of Disease Study 2015 (GBD 2015) Obesity and Overweight Prevalence 1980–2015. Institute for Health Metrics and Evauation (IHME), Seattle, United State of America
Chooi YC, Ding C, Magkos F (2019) The epidemiology of obesity. Metabolism 92:6–10. https://doi.org/10.1016/j.metabol.2018.09.005
Rodrigues LC, Canella DS, Claro RM (2022) Time trend of overweight and obesity prevalence among older people in Brazilian State Capitals and the Federal District from 2006 to 2019. Eur J Ageing 19(3):555–565. https://doi.org/10.1007/s10433-021-00659-x
Estivaleti JM, Guzman-Habinger J, Lobos J, Azeredo CM, Claro R, Ferrari G, Adami F, Rezende LFM (2022) Time trends and projected obesity epidemic in Brazilian adults between 2006 and 2030. Sci Rep 12(1):12699. https://doi.org/10.1038/s41598-022-16934-5
Wang X, Song J, Gao Y, Wu C, Zhang X, Li T, Cui J, Song L, Xu W, Yang Y, Zhang H, Lu J, Li X, Liu J, Zheng X (2021) Association between weight gain from young to middle adulthood and metabolic syndrome across different BMI categories at young adulthood. Front Endocrinol (Lausanne) 12:812104. https://doi.org/10.3389/fendo.2021.812104
de Mutsert R, Sun Q, Willett WC, Hu FB, van Dam RM (2014) Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: a cohort study. Am J Epidemiol 179(11):1353–1365. https://doi.org/10.1093/aje/kwu052
Zheng Y, Manson JE, Yuan C, Liang MH, Grodstein F, Stampfer MJ, Willett WC, Hu FB (2017) Associations of weight gain from early to middle adulthood with major health outcomes later in life. JAMA 318(3):255–269. https://doi.org/10.1001/jama.2017.7092
Kim MS, Kim WJ, Khera AV, Kim JY, Yon DK, Lee SW, Shin JI, Won H-H (2021) Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J 42(34):3388–3403. https://doi.org/10.1093/eurheartj/ehab454
Global BMIMC, Di Angelantonio E, Bhupathiraju Sh N, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, Cairns BJ, Huxley R, Jackson Ch L, Joshy G, Lewington S, Manson JE, Murphy N, Patel AV, Samet JM, Woodward M, Zheng W, Zhou M, Bansal N, Barricarte A, Carter B, Cerhan JR, Smith GD, Fang X, Franco OH, Green J, Halsey J, Hildebrand JS, Jung KJ, Korda RJ, McLerran DF, Moore SC, O’Keeffe LM, Paige E, Ramond A, Reeves GK, Rolland B, Sacerdote C, Sattar N, Sofianopoulou E, Stevens J, Thun M, Ueshima H, Yang L, Yun YD, Willeit P, Banks E, Beral V, Chen Z, Gapstur SM, Gunter MJ, Hartge P, Jee SH, Lam TH, Peto R, Potter JD, Willett WC, Thompson SG, Danesh J, Hu FB (2016) Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388(10046):776–786. https://doi.org/10.1016/S0140-6736(16)30175-1
World Health O (2011) Global status report on noncommunicable diseases 2010. World Health Organization, Geneva
Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, Toplak H, Obesity Management Task Force of the European Association for the Study of O (2015) European guidelines for obesity management in adults. Obes Facts 8(6):402–424. https://doi.org/10.1159/000442721
Popkin BM (2006) Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr 84(2):289–298. https://doi.org/10.1093/ajcn/84.1.289
Collaboration NCDRF (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387(10026):1377–1396. https://doi.org/10.1016/S0140-6736(16)30054-X
Beslay M, Srour B, Mejean C, Alles B, Fiolet T, Debras C, Chazelas E, Deschasaux M, Wendeu-Foyet MG, Hercberg S, Galan P, Monteiro CA, Deschamps V, Calixto Andrade G, Kesse-Guyot E, Julia C, Touvier M (2020) Ultra-processed food intake in association with BMI change and risk of overweight and obesity: a prospective analysis of the French NutriNet-Sante cohort. PLoS Med 17(8):e1003256. https://doi.org/10.1371/journal.pmed.1003256
Canhada SL, Luft VC, Giatti L, Duncan BB, Chor D, Fonseca M, Matos SMA, Molina M, Barreto SM, Levy RB, Schmidt MI (2020) Ultra-processed foods, incident overweight and obesity, and longitudinal changes in weight and waist circumference: the Brazilian longitudinal study of adult health (ELSA-Brasil). Public Health Nutr 23(6):1076–1086. https://doi.org/10.1017/S1368980019002854
González-Morales R, Canto-Osorio F, Stern D, Sánchez-Romero LM, Torres-Ibarra L, Hernández-López R, Rivera-Paredez B, Vidaña-Pérez D, Ramírez-Palacios P, Salmerón J, Popkin BM, Barrientos-Gutiérrez T (2020) Soft drink intake is associated with weight gain, regardless of physical activity levels: the health workers cohort study. Int J Behav Nutr Phys Act 17(1):60. https://doi.org/10.1186/s12966-020-00963-2
Konieczna J, Romaguera D, Pereira V, Fiol M, Razquin C, Estruch R, Asensio EM, Babio N, Fitó M, Gómez-Gracia E, Ros E, Lapetra J, Arós F, Serra-Majem L, Pintó X, Toledo E, Sorlí JV, Bulló M, Schröder H, Martínez-González MA (2019) Longitudinal association of changes in diet with changes in body weight and waist circumference in subjects at high cardiovascular risk: the PREDIMED trial. Int J Behav Nutr Phys Act 16(1):139. https://doi.org/10.1186/s12966-019-0893-3
Castro MA, Baltar VT, Marchioni DM, Fisberg RM (2016) Examining associations between dietary patterns and metabolic CVD risk factors: a novel use of structural equation modelling. Br J Nutr 115(9):1586–1597. https://doi.org/10.1017/s0007114516000556
Silveira BKS, de Novaes JF, Reis NA, Lourenco LP, Capobiango AHM, Vieira SA, Hermsdorff HHM (2018) Traditional and healthy dietary patterns are associated with low cardiometabolic risk in Brazilian subjects. Cardiol Res Pract 2018:4585412. https://doi.org/10.1155/2018/4585412
de Oliveira Santos R, Vieira D, Miranda AAM, Fisberg RM, Marchioni DM, Baltar VT (2017) The traditional lunch pattern is inversely correlated with body mass index in a population-based study in Brazil. BMC Public Health 18(1):33. https://doi.org/10.1186/s12889-017-4582-3
Lin H, Bermudez OI, Tucker KL (2003) Dietary patterns of hispanic elders are associated with acculturation and obesity. J Nutr 133(11):3651–3657. https://doi.org/10.1093/jn/133.11.3651
Park SY, Murphy SP, Wilkens LR, Yamamoto JF, Sharma S, Hankin JH, Henderson BE, Kolonel LN (2005) Dietary patterns using the food guide pyramid groups are associated with sociodemographic and lifestyle factors: the multiethnic cohort study. J Nutr 135(4):843–849. https://doi.org/10.1093/jn/135.4.843
Carioca AAF, Gorgulho B, Teixeira JA, Fisberg RM, Marchioni DM (2017) Dietary patterns in internal migrants in a continental country: a population-based study. PLoS ONE 12(10):e0185882. https://doi.org/10.1371/journal.pone.0185882
de Almeida Alves M, Molina M, da Fonseca MJM, Lotufo PA, Bensenor IM, Marchioni DML (2022) Different statistical methods identify similar population-specific dietary patterns: an analysis of longitudinal study of adult health (ELSA-Brasil). Br J Nutr 128(11):2249–2257. https://doi.org/10.1017/S0007114522000253
Aquino EM, Araujo MJ, Almeida Mda C, Conceicao P, Andrade CR, Cade NV, Carvalho M, Figueiredo RC, Fonseca Mde J, Giatti L, Menezes GM, Nunes MA, Souza AG, Vasconcellos-Silva PR, Vigo A (2013) Participants recruitment in ELSA-Brasil (Brazilian Longitudinal Study for Adult Health). Rev Saude Publica 47(Suppl 2):10–18. https://doi.org/10.1590/s0034-8910.2013047003953
Aquino EM, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB, Lotufo PA, Mill JG, Molina Mdel C, Mota EL, Passos VM, Schmidt MI, Szklo M (2012) Brazilian longitudinal study of adult health (ELSA-Brasil): objectives and design. Am J Epidemiol 175(4):315–324. https://doi.org/10.1093/aje/kwr294
Bensenor IM, Griep RH, Pinto KA, Faria CP, Felisbino-Mendes M, Caetano EI, Albuquerque Lda S, Schmidt MI (2013) Routines of organization of clinical tests and interviews in the ELSA-Brasil investigation center. Rev Saude Publica 47(Suppl 2):37–47. https://doi.org/10.1590/s0034-8910.2013047003780
Aquino EM, Vasconcellos-Silva PR, Coeli CM, Araujo MJ, Santos SM, Figueiredo RC, Duncan BB (2013) Ethical issues in longitudinal studies: the case of ELSA-Brasil. Rev Saude Publica 47(Suppl 2):19–26. https://doi.org/10.1590/s0034-8910.2013047003804
McCrory MA, McCrory MA, Hajduk CL, Roberts SB (2002) Procedures for screening out inaccurate reports of dietary energy intake. Public Health Nutr 5(6A):873–882. https://doi.org/10.1079/PHN2002387
Molina Mdel C, Bensenor IM, Cardoso Lde O, Velasquez-Melendez G, Drehmer M, Pereira TS, Faria CP, Melere C, Manato L, Gomes AL, Fonseca Mde J, Sichieri R (2013) Reproducibility and relative validity of the food frequency questionnaire used in the ELSA-Brasil. Cad Saude Publica 29(2):379–389
Molina MCB, CPd F, Cardoso LO, Drehmer M, Velasquez-Meléndez JG, Gomes ALC, Melere C, Diniz MFHS, Sichieri R, Benseñor IJM (2013) Diet assessment in the Brazilian longitudinal study of adult health (ELSA-Brasil): development of a food frequency questionnaire. Revista de Nutrição 26
Lohman TGRA, Martorell R (1988) Anthropometric standardization reference manual. Human Kinetics Books
Schmidt MI, Griep RH, Passos VM, Luft VC, Goulart AC, Menezes GM, Molina Mdel C, Vigo A, Nunes MA (2013) Strategies and development of quality assurance and control in the ELSA-Brasil. Rev Saude Publica 47(Suppl 2):105–112. https://doi.org/10.1590/s0034-8910.2013047003889
Resende CB, Luft VC, Duncan B, Griep RH, Molina M, Barreto SM, Schmidt MI (2021) Birth weight and body fat mass in adults assessed by bioimpedance in the ELSA-Brasil study. Cad Saude Publica 37(2):e00061619. https://doi.org/10.1590/0102-311X00061619
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB
Akaike H (1998) Information theory and an extension of the maximum likelihood principle. In: Parzen E, Tanabe K, Kitagawa G (eds) Selected papers of Hirotugu Akaike. Springer New York, New York, NY, pp 199–213. https://doi.org/10.1007/978-1-4612-1694-0_15
Liu J, Steele EM, Li Y, Yi SS, Monteiro CA, Mozaffarian D (2023) Consumption of ultraprocessed foods and body fat distribution among U.S. adults. Am J Prev Med. https://doi.org/10.1016/j.amepre.2023.03.012
Machado PP, Steele EM, Levy RB, da Costa Louzada ML, Rangan A, Woods J, Gill T, Scrinis G, Monteiro CA (2020) Ultra-processed food consumption and obesity in the Australian adult population. Nutr Diabetes 10(1):39. https://doi.org/10.1038/s41387-020-00141-0
Monteiro CA, Ricardo CZ, Calixto G, Machado P, Martins C, Steele EM, Baraldi LG, Garzillo JMF, Sattamini I, Cannon G, Levy RB, Moubarac JC, Jaime PC, Martins AP, Canella DS, Louzada MLC, Parra D (2016) NOVA. The star shines bright. World Nutr 7(1–3):28–38
Longo GZ, Ordaz KD, da Silva DCG, Hinnig PF, Roberto DMT, Reinert C, Pot GK, Palla L (2022) Dietary patterns and cardiovascular risk factors among brazilians: a population-based study in Viçosa. Minas Gerais Nutr 98:111626. https://doi.org/10.1016/j.nut.2022.111626
Carvalho AM, Selem SS, Miranda AM, Marchioni DM (2016) Excessive red and processed meat intake: relations with health and environment in Brazil. Br J Nutr 115(11):2011–2016. https://doi.org/10.1017/S0007114516000969
de Carvalho AM, Cesar CL, Fisberg RM, Marchioni DM (2013) Excessive meat consumption in Brazil: diet quality and environmental impacts. Public Health Nutr 16(10):1893–1899. https://doi.org/10.1017/S1368980012003916
Papier K, Hartman L, Tong TYN, Key TJ, Knuppel A (2022) Higher meat intake is associated with higher inflammatory markers, mostly due to adiposity: results from UK Biobank. J Nutr 152(1):183–189. https://doi.org/10.1093/jn/nxab314
Havemeier S, Erickson J, Slavin J (2017) Dietary guidance for pulses: the challenge and opportunity to be part of both the vegetable and protein food groups. Ann N Y Acad Sci 1392(1):58–66. https://doi.org/10.1111/nyas.13308
Satija A, Hu FB (2018) Plant-based diets and cardiovascular health. Trends Cardiovasc Med 28(7):437–441. https://doi.org/10.1016/j.tcm.2018.02.004
Westerterp-Plantenga MS, Nieuwenhuizen A, Tome D, Soenen S, Westerterp KR (2009) Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr 29:21–41. https://doi.org/10.1146/annurev-nutr-080508-141056
Bray GA, Lovejoy JC, Smith SR, DeLany JP, Lefevre M, Hwang D, Ryan DH, York DA (2002) The influence of different fats and fatty acids on obesity, insulin resistance and inflammation. J Nutr 132(9):2488–2491. https://doi.org/10.1093/jn/132.9.2488
Watzl B, Kulling SE, Moseneder J, Barth SW, Bub A (2005) A 4-wk intervention with high intake of carotenoid-rich vegetables and fruit reduces plasma C-reactive protein in healthy, nonsmoking men. Am J Clin Nutr 82(5):1052–1058. https://doi.org/10.1093/ajcn/82.5.1052
Butcher JL, Beckstrand RL (2010) Fiber’s impact on high-sensitivity C-reactive protein levels in cardiovascular disease. J Am Acad Nurse Pract 22(11):566–572. https://doi.org/10.1111/j.1745-7599.2010.00555.x
Holscher HD, Caporaso JG, Hooda S, Brulc JM, Fahey GC Jr., Swanson KS (2015) Fiber supplementation influences phylogenetic structure and functional capacity of the human intestinal microbiome: follow-up of a randomized controlled trial. Am J Clin Nutr 101(1):55–64. https://doi.org/10.3945/ajcn.114.092064
Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, Aquino EM, Passos VM, Matos SM, Molina Mdel C, Carvalho MS, Bensenor IM (2015) Cohort profile: longitudinal study of adult health (ELSA-Brasil). Int J Epidemiol 44(1):68–75. https://doi.org/10.1093/ije/dyu027
Funding
The ELSA- Brasil study was supported by the Brazilian Ministry of Health, the Brazilian Ministry of Science and Technology and the Brazilian National Council for Scientific and Technological Development- CNPq. The research center of São Paulo was also supported by the São Paulo Research Foundation (FAPESP) (grant number 2011/12256-4). The Graduate Program of Public Health Nutrition is supported by the Coordination of Superior Level Staff Improvement (CAPES). M.A.A. received a scholarship from the São Paulo Research Foundation (FAPESP) (grant number 2019/13486-5). The funding agencies that supported the study had no role in the design, analysis or writing of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alves, M.A., Lotufo, P.A., Benseñor, I. et al. Dietary patterns and adiposity over time – analysis of the ELSA-Brasil. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03350-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03350-w