Abstract
Purpose
There have been no reports on the application of salivary iodine concentration (SIC) in evaluating iodine nutrition in pregnant women. This study aimed to clarify the relationship between SIC and indicators of iodine nutritional status and thyroid function during pregnancy, to investigate whether salivary iodine can be applied to the evaluation of iodine nutritional status in pregnant women, and to provide a reference basis for establishing a normal range of salivary iodine values during pregnancy.
Methods
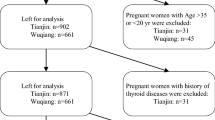
Pregnant women were enrolled in the Department of Obstetrics, the people’s hospital of Yuncheng Country, Shandong Province, from July 2021 to December 2022, using random cluster sampling. Saliva, urine, and blood samples were collected from pregnant women to assess iodine nutritional status, and venous blood was collected to determine thyroid function.
Results
A total of 609 pregnant women were included in this study. The median spot urinary iodine concentration (SUIC) was 261 μg/L. The median SIC was 297 μg/L. SIC was positively correlated with SUIC (r = 0.46, P < 0.0001), 24-h UIC (r = 0.30, P < 0.0001), 24-h urinary iodine excretion (24-h UIE) (r = 0.41, P < 0.0001), and estimated iodine intake (EII) (r = 0.52, P < 0.0001). After adjusting for confounders, there was a weak correlation between SIC and serum total iodine and serum non-protein-bound iodine (P = 0.02, P = 0.04, respectively). Pregnant women with a SIC < 176 μg/L had a higher risk of insufficient iodine status (OR = 2.07, 95% CI 1.35–3.19) and thyroid dysfunction (OR = 2.71, 95% CI 1.18–6.21) compared to those with higher SIC. Those having SIC > 529 μg/L were more likely to have excessive iodine status (OR = 2.82, 95% CI 1.81–4.38) and thyroid dysfunction (OR = 3.04, 95% CI 1.36–6.78) than those with lower SIC values.
Conclusion
SIC is associated with urinary iodine concentration and thyroid function in pregnant women. SIC < 176 μg/L was associated with an increased risk for iodine deficiency and hypothyroxinemia, while SIC > 529 μg/L was related to excess and thyrotoxicosis. SIC can be used as a reference indicator for evaluating the iodine nutrition status of pregnant women, but it needs further investigation and verification.
Trial registration
NCT04492657(Aug 9, 2022).



Similar content being viewed by others
Data availability
All data are available by reasonable request from the corresponding author.
References
Swanson CA, Zimmermann MB, Skeaff S, Pearce EN, Dwyer JT, Trumbo PR, Zehaluk C, Andrews KW, Carriquiry A, Caldwell KL, Egan SK, Long SE, Bailey RL, Sullivan KM, Holden JM, Betz JM, Phinney KW, Brooks SP, Johnson CL, Haggans CJ (2012) Summary of an NIH workshop to identify research needs to improve the monitoring of iodine status in the United States and to inform the DRI. J Nutr 142(6):1175–1185. https://doi.org/10.3945/jn.111.156448
Zimmermann MB, Boelaert K (2015) Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 3(4):286–295. https://doi.org/10.1016/s2213-8587(14)70225-6
Chen W, Sang Z, Tan L, Zhang S, Dong F, Chu Z, Wei W, Zhao N, Zhang G, Yao Z, Shen J, Zhang W (2015) Neonatal thyroid function born to mothers living with long-term excessive iodine intake from drinking water. Clin Endocrinol 83(3):399–404. https://doi.org/10.1111/cen.12625
Tan L, Sang Z, Shen J, Liu H, Chen W, Zhao N, Wei W, Zhang G, Zhang W (2015) Prevalence of thyroid dysfunction with adequate and excessive iodine intake in Hebei Province, People’s Republic of China. Public Health Nutr 18(9):1692–1697. https://doi.org/10.1017/s1368980014002237
Zimmermann MB (2016) The importance of adequate iodine during pregnancy and infancy. World Rev Nutr Dietetics 115:118–124. https://doi.org/10.1159/000442078
Markhus MW, Dahl L, Moe V, Abel MH, Brantsæter AL, Øyen J, Meltzer HM, Stormark KM, Graff IE, Smith L, Kjellevold M (2018) Maternal iodine status is associated with offspring language skills in infancy and toddlerhood. Nutrients. https://doi.org/10.3390/nu10091270
Yarrington C, Pearce EN (2011) Iodine and pregnancy. J Thyroid Res 2011:934104. https://doi.org/10.4061/2011/934104
Nishiyama S, Mikeda T, Okada T, Nakamura K, Kotani T, Hishinuma A (2004) Transient hypothyroidism or persistent hyperthyrotropinemia in neonates born to mothers with excessive iodine intake. Thyroid 14(12):1077–1083. https://doi.org/10.1089/thy.2004.14.1077
Sang Z, Wei W, Zhao N, Zhang G, Chen W, Liu H, Shen J, Liu J, Yan Y, Zhang W (2012) Thyroid dysfunction during late gestation is associated with excessive iodine intake in pregnant women. J Clin Endocrinol Metab 97(8):E1363–E1369. https://doi.org/10.1210/jc.2011-3438
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB (2016) Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr 104(Suppl 3):918s–923s. https://doi.org/10.3945/ajcn.115.110429
König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB (2011) Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J Nutr 141(11):2049–2054. https://doi.org/10.3945/jn.111.144071
Rohner F, Zimmermann M, Jooste P, Pandav C, Caldwell K, Raghavan R, Raiten DJ (2014) Biomarkers of nutrition for development–iodine review. J Nutr 144(8):1322s–1342s. https://doi.org/10.3945/jn.113.181974
O’Kane SM, Mulhern MS, Pourshahidi LK, Strain JJ, Yeates AJ (2018) Micronutrients, iodine status and concentrations of thyroid hormones: a systematic review. Nutr Rev 76(6):418–431. https://doi.org/10.1093/nutrit/nuy008
Venturi S, Venturi M (2009) Iodine in evolution of salivary glands and in oral health. Nutrition and health 20 (2):119–134. https://doi:https://doi.org/10.1177/026010600902000204
Gates GA, Work WP (1967) Radioisotope scanning of the salivary glands. A preliminary report. Laryngoscope 77(5):861–875. https://doi.org/10.1288/00005537-196705000-00013
Mishkin FS (1981) Radionuclide salivary gland imaging. Seminars Nuclear Med 11(4):258–265. https://doi.org/10.1016/s0001-2998(81)80023-2
Mandel SJ, Mandel L (2003) Radioactive iodine and the salivary glands. Thyroid 13(3):265–271. https://doi.org/10.1089/105072503321582060
Zhang JSJ, Gao J, Zhao W, Jiao J, Lou J, Chen Z (2002) Iodine determination in salivary samples and the relationship between iodine concentration in saliva and urine. (In Chinese). Chin J Ctrl Endem Dis 5:257–260. https://doi.org/10.3969/j.issn.1001-1889.2002.05.002
Vought RL, London WT (1965) Effect of dietary iodine on serum inorganic and salivary iodine. Metabolism 14:699–707. https://doi.org/10.1016/0026-0495(65)90053-3
Dekker BL, Touw DJ, van der Horst-Schrivers ANA, Vos MJ, Links TP, Dijck-Brouwer DAJ, Kobold ACM (2021) Use of salivary iodine concentrations to estimate the iodine status of adults in clinical practice. J Nutr 151(12):3671–3677. https://doi.org/10.1093/jn/nxab303
Gulaboglul M, Akgul HM, Akgul N, Cetin M (2012) Urine and saliva iodine levels in patients with dental caries and normal healthy volunteers. Trace Elem Electrolytes 29(1):28–33. https://doi.org/10.5414/tex01186
Guo W, Pan Z, Zhang Y, Jin Y, Dong S, Wu W, Chen W, Zhang W (2020) Saliva iodine concentration in children and its association with iodine status and thyroid function. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgaa471
Guo W, Dong S, Jin Y, Pan Z, Pearce EN, Wu W, Zhang Y, Chen W, Zhang W (2021) Evaluation of variation of saliva iodine and recommendations for sample size and sampling time: implications for assessing iodine nutritional status. Clin Nutr (Edinburgh, Scotland) 40(5):3559–3566. https://doi.org/10.1016/j.clnu.2020.12.010
Jahreis G, Hausmann W, Kiessling G, Franke K, Leiterer M (2001) Bioavailability of iodine from normal diets rich in dairy products–results of balance studies in women. Exp Clin Endocrinol Diabetes 109(3):163–167. https://doi.org/10.1055/s-2001-14840
Institute of Medicine (2001) Dietary reference intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academies Press (US), Washington
Papadopoulos S, MacFarlane S, Harden RM, Mason DK, Alexander WD (1966) Iodine excretion in urine, saliva, gastric juice and sweat in dehalogenase deficiency. J Endocrinol 36(4):341–346. https://doi.org/10.1677/joe.0.0360341
Liu JSL (2010) Research on the diagnostic application of saliva. (In Chinese). Int J Med Parasit Dis 37:43–48. https://doi.org/10.3760/cma.j.issn.1673-4122.2010.01.009
Mesko MF, Costa VC, Picoloto RS, Bizzi CA, Mello PA (2016) Halogen determination in food and biological materials using plasma-based techniques: challenges and trends of sample preparation. J Anal At Spectrom 31(6):1243–1261. https://doi.org/10.1039/c5ja00488h
Mello PA, Barin JS, Duarte FA, Bizzi CA, Diehl LO, Muller EI, Flores EM (2013) Analytical methods for the determination of halogens in bioanalytical sciences: a review. Anal Bioanal Chem 405(24):7615–7642. https://doi.org/10.1007/s00216-013-7077-9
Kaufman E, Lamster IB (2002) The diagnostic applications of saliva—a review. Crit Rev Oral Biol Med 13(2):197–212. https://doi.org/10.1177/154411130201300209
Navazesh M (1993) Methods for collecting saliva. Ann NY Acad Sci 694:72–77. https://doi.org/10.1111/j.1749-6632.1993.tb18343.x
Chen LYZ, Li R, Lin C, Zhang J, Chen W (2013) Influence of different sizes and concentrations of citric acid filter paper on salivary secretion and salivary alpha-amylase activity in healthy volunteers. (In Chinese). J Guangzhou Univ Trad Chin Med 30:186–190. https://doi.org/10.1335/j.cnki.gzxbtcm.2013.02.013
Zhang PLW, Liu S, Liu X, Sang M, Liu L, Lin H, Sang Z (2018) Study on iodine content in saliva of adults in different seasons. (In Chinese). J Tianjin Medical University 24:255–258
Zareba G, Cernichiari E, Goldsmith LA, Clarkson TW (1995) Biological monitoring of iodine, a water disinfectant for long-term space missions. Environ Health Perspect 103(11):1032–1035. https://doi.org/10.1289/ehp.951031032
Als C, Helbling A, Peter K, Haldimann M, Zimmerli B, Gerber H (2000) Urinary iodine concentration follows a circadian rhythm: a study with 3023 spot urine samples in adults and children. J Clin Endocrinol Metab 85(4):1367–1369. https://doi.org/10.1210/jcem.85.4.6496
Rasmussen LB, Ovesen L, Christiansen E (1999) Day-to-day and within-day variation in urinary iodine excretion. Eur J Clin Nutr 53(5):401–407. https://doi.org/10.1038/sj.ejcn.1600762
Busnardo B, Nacamulli D, Zambonin L, Mian C, Piccolo M, Girelli ME (2006) Restricted intraindividual urinary iodine concentration variability in nonfasting subjects. Eur J Clin Nutr 60(3):421–425. https://doi.org/10.1038/sj.ejcn.1602334
Als C, Haldimann M, Bürgi E, Donati F, Gerber H, Zimmerli B (2003) Swiss pilot study of individual seasonal fluctuations of urinary iodine concentration over two years: is age-dependency linked to the major source of dietary iodine? Eur J Clin Nutr 57(5):636–646. https://doi.org/10.1038/sj.ejcn.1601590
Delange F (1997) Neonatal screening for congenital hypothyroidism: results and perspectives. Hormone Res 48(2):51–61. https://doi.org/10.1159/000185485
Zimmermann MB, Aeberli I, Torresani T, Bürgi H (2005) Increasing the iodine concentration in the Swiss iodized salt program markedly improved iodine status in pregnant women and children: a 5-y prospective national study. Am J Clin Nutr 82(2):388–392. https://doi.org/10.1093/ajcn.82.2.388
World Health Organization (2001) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 2nd edn. World Health Organization, Geneva
Pan Z, Cui T, Chen W, Gao S, Pearce EN, Wang W, Chen Y, Guo W, Tan L, Shen J, Zhang W (2019) Serum iodine concentration in pregnant women and its association with urinary iodine concentration and thyroid function. Clin Endocrinol 90(5):711–718. https://doi.org/10.1111/cen.13945
Acknowledgements
The authors thank the Yuncheng County People’s Hospital for their support and help in field investigations. They appreciate the co-cooperation and participations of teachers, nurses, and pregnant women.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC Grant no. 81920108031 and 82230113).
Author information
Authors and Affiliations
Contributions
ZW designed the research. LS performed the field investigation, the data analysis, and wrote the paper. GW took part in the data analysis and paper writing. JQ, MQ, YR, FM, and WT performed the field investigation and collected the data. ZH, LD, and MX performed the laboratory analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was approved by the Ethics Committee of Tianjin Medical University (serial number: TMUhMEC2020033). All procedures performed in the studies were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participants provided an informed consent after receiving a full explanation of the purpose and procedure of the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, S., Guo, W., Jin, Q. et al. Salivary iodine concentration in pregnant women and its association with iodine status and thyroid function. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03332-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03332-y