Abstract
Purpose
Previous observational studies have shown that green tea consumption is associated with a reduced incidence of digestive system cancers (DSCs). However, the observed association could be due to confounding factors. Therefore, we used a two-sample Mendelian randomization (MR) approach to assess the causal effect of green tea intake on the risk of five common DSCs.
Methods
Independent genetic variants strongly associated with green tea consumption in European and East Asian populations were selected as instrumental variables in genome-wide association studies involving up to 64,949 European individuals and 152,653 East Asian individuals, respectively. The associations between genetic variants and DSCs were extracted from the FinnGen study and the Japan Biobank. The primary analysis was performed using random-effects inverse variance weighting (IVW). Other MR analyses, including weighted mode-based estimate, weighted-median, MR-Egger regression, Mendelian Randomization-Pleiotropy Residual Sum and Outlier (MR-PRESSO) analysis, were used for sensitivity analyses. In addition, a multivariate MR design was performed to adjust for smoking and alcohol consumption.
Results
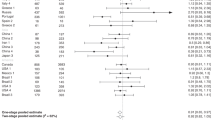
The IVW results showed no causal relationship between tea intake and DSCs risk in European population (esophagus cancer: odds ratio (OR) = 1.044, 95% confidence interval (CI) 0.992–1.099, p = 0.096; stomach cancer: OR = 0.988, 95% CI 0.963–1.014, p = 0.368; colorectal cancer: OR = 1.003, 95% CI 0.992–1.015, p = 0.588; liver cancer: OR = 0.996, 95% CI 0.960–1.032, p = 0.808; pancreatic cancer: OR = 0.990, 95% CI 0.965–1.015, p = 0.432). The MR-Egger regression, MR-PRESSO analysis and other methods also confirmed the reliability of the conclusion. Similarly, no significant association was found between green tea consumption and the incidence of DSCs among East Asians. This relationship is not significant even after adjusting for smoking and alcohol consumption (P > 0.05).
Conclusion
Our study provides evidence that genetically predicted green tea intake is not causally associated with the development of DSCs in the European and East Asian population.


Similar content being viewed by others
Data availability
The data that support the findings of this study are openly available in FinnGen (https://www.finngen.fi/en), UK Biobank (http://www.nealelab.is/uk-biobank) and BioBank Japan studies (http://jenger.riken.jp/en/).
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-A Cancer J Clin 71(3):209–249
Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, Bray F (2020) Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159(1):335
Eisenstein M (2019) Tea’s value as a cancer therapy is steeped in uncertainty. Nature 566(7742):S6–S7
Yang CS, Zhang J (2019) Studies on the prevention of cancer and cardiometabolic diseases by tea: issues on mechanisms, effective doses, and toxicities. J Agric Food Chem 67(19):5446–5456
Liu K, Zhou R, Wang B, Chen K, Shi L-Y, Zhu T-D, Mi M-T (2013) Effect of green tea on glucose control and insulin sensitivity: a meta-analysis of 17 randomized controlled trials. Am J Clin Nutr 98(2):340–348
Yu J, Song P, Perry R, Penfold C, Cooper AR (2017) The effectiveness of green tea or green tea extract on insulin resistance and glycemic control in type 2 diabetes mellitus: a meta-analysis. Diabetes Metab J 41(4):251–262
Iwasaki M, Mizusawa J, Kasuga Y, Yokoyama S, Onuma H, Nishimura H, Kusama R, Tsugane S (2014) Green tea consumption and breast cancer risk in Japanese women: a case–control study. Nutr Cancer 66(1):57–67
Sheerah H, Keyang L, Eshak ES, Cui R, Shirai K, Muraki I, Iso H, Tamakoshi A (2020) Association of tea consumption and the risk of gastric cancer in Japanese adults: the Japan Collaborative Cohort Study. BMJ Open 10(10):e038243
Lin Y, Kikuchi S, Tamakoshi A, Yagyu K, Obata Y, Kurosawa M, Inaba Y, Kawamura T, Motohashi Y, Ishibashi T (2008) Green tea consumption and the risk of pancreatic cancer in Japanese adults. Pancreas 37(1):25–30
Yi Y, Liang H, Jing H, Jian Z, Guang Y, Jun Z, Zhu H, Jian L (2020) Green tea consumption and esophageal cancer risk: a meta-analysis. Nutr Cancer Int J 72(3):513–521
Sang LX, Chang B, Li XH, Jiang M (2013) Green tea consumption and risk of esophageal cancer: a meta-analysis of published epidemiological studies. Nutr Cancer 65(6):802–812. https://doi.org/10.1080/01635581.2013.805423
Zhao H, Mei K, Yang L, Liu X, Xie L (2021) Green tea consumption and risk for esophageal cancer: a systematic review and dose-response meta-analysis. Nutrition. https://doi.org/10.1016/j.nut.2021.111197
Huang Y, Chen H, Zhou L, Li G, Yi D, Zhang Y, Wu Y, Liu X, Wu X, Song Q, Liu L, Yi D (2017) Association between green tea intake and risk of gastric cancer: a systematic review and dose-response meta-analysis of observational studies. Public Health Nutr 20(17):3183–3192
Myung SK, Bae WK, Oh SM, Kim Y, Ju W, Sung J, Lee YJ, Ko JA, Song JI, Choi HJ (2009) Green tea consumption and risk of stomach cancer: a meta-analysis of epidemiologic studies. Int J Cancer 124(3):670–677
Yang G, Zheng W, Xiang YB, Gao J, Li HL, Zhang X, Gao YT, Shu XO (2011) Green tea consumption and colorectal cancer risk: a report from the Shanghai Men’s Health Study. Carcinogenesis 32(11):1684–1688. https://doi.org/10.1093/carcin/bgr186
Yang WS, Zeng XF, Liu ZN, Zhao QH, Tan YT, Gao J, Li HL, Xiang YB (2020) Diet and liver cancer risk: a narrative review of epidemiological evidence. Br J Nutr 124(3):330–340
Huang YQ, Lu X, Min H, Wu QQ, Shi XT, Bian KQ, Zou XP (2016) Green tea and liver cancer risk: a meta-analysis of prospective cohort studies in Asian populations. Nutrition 32(1):3–8
Zeng JL, Li ZH, Wang ZC, Zhang HL (2014) Green tea consumption and risk of pancreatic cancer: a meta-analysis. Nutrients 6(11):4640–4650
Thompson SG, Burgess S (2015) Mendelian randomization :methods for using genetic variants in causal estimation. Chapman and Hall/CRC, New York
Skrivankova VW, Richmond RC, Woolf BAR, Yarmolinsky J, Davies NM, Swanson SA, VanderWeele TJ, Higgins JPT, Timpson NJ, Dimou N, Langenberg C, Golub RM, Loder EW, Gallo V, Tybjaerg-Hansen A, Davey SG, Egger M, Richards JB (2021) Strengthening the reporting of observational studies in epidemiology using Mendelian randomization: the STROBE-MR statement. JAMA 326(16):1614–1621
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R (2015) UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12(3):e1001779. https://doi.org/10.1371/journal.pmed.1001779
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner K, Reeve MP, Laivuori H, Aavikko M, Kaunisto MA (2022) FinnGen: unique genetic insights from combining isolated population and national health register data. medRxiv. https://doi.org/10.1101/2022.03.03.22271360
Liu M, Jiang Y, Wedow R, Li Y, Brazel DM, Chen F, Datta G, Davila-Velderrain J, McGuire D, Tian C, Zhan X, Research T, Psychiatry HAI, Choquet H, Docherty AR, Faul JD, Foerster JR, Fritsche LG, Gabrielsen ME, Gordon SD, Haessler J, Hottenga JJ, Huang H, Jang SK, Jansen PR, Ling Y, Magi R, Matoba N, McMahon G, Mulas A, Orru V, Palviainen T, Pandit A, Reginsson GW, Skogholt AH, Smith JA, Taylor AE, Turman C, Willemsen G, Young H, Young KA, Zajac GJM, Zhao W, Zhou W, Bjornsdottir G, Boardman JD, Boehnke M, Boomsma DI, Chen C, Cucca F, Davies GE, Eaton CB, Ehringer MA, Esko T, Fiorillo E, Gillespie NA, Gudbjartsson DF, Haller T, Harris KM, Heath AC, Hewitt JK, Hickie IB, Hokanson JE, Hopfer CJ, Hunter DJ, Iacono WG, Johnson EO, Kamatani Y, Kardia SLR, Keller MC, Kellis M, Kooperberg C, Kraft P, Krauter KS, Laakso M, Lind PA, Loukola A, Lutz SM, Madden PAF, Martin NG, McGue M, McQueen MB, Medland SE, Metspalu A, Mohlke KL, Nielsen JB, Okada Y, Peters U, Polderman TJC, Posthuma D, Reiner AP, Rice JP, Rimm E, Rose RJ, Runarsdottir V, Stallings MC, Stancakova A, Stefansson H, Thai KK, Tindle HA, Tyrfingsson T, Wall TL, Weir DR, Weisner C, Whitfield JB, Winsvold BS, Yin J, Zuccolo L, Bierut LJ, Hveem K, Lee JJ, Munafo MR, Saccone NL, Willer CJ, Cornelis MC, David SP, Hinds DA, Jorgenson E, Kaprio J, Stitzel JA, Stefansson K, Thorgeirsson TE, Abecasis G, Liu DJ, Vrieze S (2019). Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet 51(2): 237–244
Matoba N, Akiyama M, Ishigaki K, Kanai M, Takahashi A, Momozawa Y, Ikegawa S, Ikeda M, Iwata N, Hirata M, Matsuda K, Murakami Y, Kubo M, Kamatani Y, Okada Y (2020) GWAS of 165,084 Japanese individuals identified nine loci associated with dietary habits. Nat Hum Behav 4(3):308–316. https://doi.org/10.1038/s41562-019-0805-1
Ishigaki K, Akiyama M, Kanai M, Takahashi A, Kawakami E, Sugishita H, Sakaue S, Matoba N, Low SK, Okada Y, Terao C, Amariuta T, Gazal S, Kochi Y, Horikoshi M, Suzuki K, Ito K, Koyama S, Ozaki K, Niida S, Sakata Y, Sakata Y, Kohno T, Shiraishi K, Momozawa Y, Hirata M, Matsuda K, Ikeda M, Iwata N, Ikegawa S, Kou I, Tanaka T, Nakagawa H, Suzuki A, Hirota T, Tamari M, Chayama K, Miki D, Mori M, Nagayama S, Daigo Y, Miki Y, Katagiri T, Ogawa O, Obara W, Ito H, Yoshida T, Imoto I, Takahashi T, Tanikawa C, Suzuki T, Sinozaki N, Minami S, Yamaguchi H, Asai S, Takahashi Y, Yamaji K, Takahashi K, Fujioka T, Takata R, Yanai H, Masumoto A, Koretsune Y, Kutsumi H, Higashiyama M, Murayama S, Minegishi N, Suzuki K, Tanno K, Shimizu A, Yamaji T, Iwasaki M, Sawada N, Uemura H, Tanaka K, Naito M, Sasaki M, Wakai K, Tsugane S, Yamamoto M, Yamamoto K, Murakami Y, Nakamura Y, Raychaudhuri S, Inazawa J, Yamauchi T, Kadowaki T, Kubo M, Kamatani Y (2020) Large-scale genome-wide association study in a Japanese population identifies novel susceptibility loci across different diseases. Nat Genet 52(7):669–679. https://doi.org/10.1038/s41588-020-0640-3
Matoba N, Akiyama M, Ishigaki K, Kanai M, Takahashi A, Momozawa Y, Ikegawa S, Ikeda M, Iwata N, Hirata M, Matsuda K, Kubo M, Okada Y, Kamatani Y (2019) GWAS of smoking behaviour in 165,436 Japanese people reveals seven new loci and shared genetic architecture. Nat Hum Behav 3(5):471–477. https://doi.org/10.1038/s41562-019-0557-y
Kamat MA, Blackshaw JA, Young R, Surendran P, Burgess S, Danesh J, Butterworth AS, Staley JR (2019) PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics 35(22):4851–4853
Shim H, Chasman DI, Smith JD, Mora S, Ridker PM, Nickerson DA, Krauss RM, Stephens M (2015) A multivariate genome-wide association analysis of 10 LDL subfractions, and their response to statin treatment, in 1868 Caucasians. PLoS ONE 10(4):e0120758
Burgess S, Thompson SG (2011) Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol 40(3):755–764
Bowden J, Davey SG, Haycock PC, Burgess S (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314
Bowden J, Davey SG, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–525
Sanderson E, Davey Smith G, Windmeijer F, Bowden J (2019) An examination of multivariable Mendelian randomization in the single-sample and two-sample summary data settings. Int J Epidemiol 48(3):713–727. https://doi.org/10.1093/ije/dyy262
Burgess S, Thompson SG (2015) Multivariable Mendelian randomization: the use of pleiotropic genetic variants to estimate causal effects. Am J Epidemiol 181(4):251–260. https://doi.org/10.1093/aje/kwu283
Li M, Duan Y, Wang Y, Chen L, Abdelrahim MEA, Yan J (2022) The effect of Green green tea consumption on body mass index, lipoprotein, liver enzymes, and liver cancer: An updated systemic review incorporating a meta-analysis. Crit Rev Food Sci Nutr. https://doi.org/10.1080/10408398.2022.2113360
Tanaka K, Tamakoshi A, Sugawara Y, Mizoue T, Inoue M, Sawada N, Matsuo K, Ito H, Naito M, Nagata C, Kitamura Y, Sadakane A, Tsugane S, Shimazu T, Research Group for the D, Evaluation of Cancer Prevention Strategies in J (2019) Coffee, green tea and liver cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol 49(10):972–984. https://doi.org/10.1093/jjco/hyz097
Filippini T, Malavolti M, Borrelli F, Izzo AA, Fairweather-Tait SJ, Horneber M, Vinceti M (2020) Green tea (Camellia sinensis) for the prevention of cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005004.pub3
Wang Z-H, Gao Q-Y, Fang J-Y (2012) Green tea and incidence of colorectal cancer: evidence from prospective cohort studies. Nutr Cancer 64(8):1143–1152
Wang X-J, Zeng X-T, Duan X-L, Zeng H-C, Shen R, Zhou P (2012) Association between green tea and colorectal cancer risk: a meta-analysis of 13 case-control studies. Asian Pac J Cancer Prev 13(7):3123–3127
Chen Y, Wu Y, Du M, Chu H, Zhu L, Tong N, Zhang Z, Wang M, Gu D, Chen J (2017) An inverse association between tea consumption and colorectal cancer risk. Oncotarget 8(23):37367–37376. https://doi.org/10.18632/oncotarget.16959
Ishikawa A, Kuriyama S, Tsubono Y, Fukao A, Takahashi H, Tachiya H, Tsuji I (2006) Smoking, alcohol drinking, green tea consumption and the risk of esophageal cancer in Japanese men. J Epidemiol 16(5):185–192. https://doi.org/10.2188/jea.16.185
Kang H, Rha SY, Oh KW, Nam CM (2010) Green tea consumption and stomach cancer risk: a meta-analysis. Epidemiol Health 32:e2010001
Higdon JV, Frei B (2003) Tea catechins and polyphenols: health effects, metabolism, and antioxidant functions. Crit Rev Food Sci Nutr 43(1):89–143. https://doi.org/10.1080/10408690390826464
Trisha AT, Shakil MH, Talukdar S, Rovina K, Huda N, Zzaman W (2022) Tea polyphenols and their preventive measures against cancer: current trends and directions. Foods. https://doi.org/10.3390/foods11213349
Rashidi B, Malekzadeh M, Goodarzi M, Masoudifar A, Mirzaei H (2017) Green tea and its anti-angiogenesis effects. Biomed Pharmacother 89:949–956. https://doi.org/10.1016/j.biopha.2017.01.161
Zhao H, Zhang M, Zhao L, Ge YK, Sheng J, Shi W (2011) Changes of constituents and activity to apoptosis and cell cycle during fermentation of tea. Int J Mol Sci 12(3):1862–1875. https://doi.org/10.3390/ijms12031862
Shirakami Y, Shimizu M (2018) Possible mechanisms of green tea and its constituents against cancer. Molecules. https://doi.org/10.3390/molecules23092284
Henning SM, Wang P, Carpenter CL, Heber D (2013) Epigenetic effects of green tea polyphenols in cancer. Epigenomics 5(6):729–741. https://doi.org/10.2217/epi.13.57
Yang CS, Wang X, Lu G, Picinich SC (2009) Cancer prevention by tea: animal studies, molecular mechanisms and human relevance. Nat Rev Cancer 9(6):429–439. https://doi.org/10.1038/nrc2641
Garabedian LF, Chu P, Toh S, Zaslavsky AM, Soumerai SB (2014) Potential bias of instrumental variable analyses for observational comparative effectiveness research. Ann Intern Med 161(2):131–138. https://doi.org/10.7326/M13-1887
Burgess S, Davies NM, Thompson SG (2016) Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol 40(7):597–608. https://doi.org/10.1002/gepi.21998
Jiang T, Gill D, Butterworth AS, Burgess S (2023) An empirical investigation into the impact of winner’s curse on estimates from Mendelian randomization. Int J Epidemiol 52(4):1209–1219. https://doi.org/10.1093/ije/dyac233
Acknowledgements
The authors thank the participants and investigators of the FinnGen, UK Biobank and BioBank Japan study. We also thank Home for Researchers editorial team (www.home-for-researchers.com) for language editing service.
Funding
The study was funded by Key Discipline Project on Chinese Pharmacology of Hunan University of Chinese Medicine [202302] and General Program of Hunan Provincial Administration of Traditional Chinese Medicine [B2023010].
Author information
Authors and Affiliations
Contributions
Conceptualization: D.N., S. L. and F.X.; methodology: H.Z., D. D, F.H. and X.N.; software: D.N, X.H., R. L. and H. Z.; formal analysis: H. Z., X. H. and X. N.; writing—original draft preparation: H. Z. and X. N., D. N; writing—review and editing, D.N., X. H., F.X., and S.L.; all the authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors claim that there were no potential conflicts of interest in the study due to business or financial relationships.
Institutional review board statement
Since our data are publicly available and all subjects have obtained informed consent to participate in the corresponding research, this study no longer requires ethical review.
Informed consent statement
All subjects obtained informed consent to participate in the corresponding study, so it was not required for this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, D., He, X., Zheng, H. et al. Association between green tea intake and digestive system cancer risk in European and East Asian populations: a Mendelian randomization study. Eur J Nutr (2024). https://doi.org/10.1007/s00394-023-03312-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-023-03312-8