Abstract
Purpose
Recent findings revealed a potential effect of a probiotic in improving quality of life (QoL) in ulcerative colitis (UC). In Jordan, there is scarce data about UC patients and QoL.
Methods
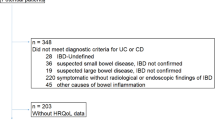
Twenty-four UC patients were included in the study and were randomly allocated into probiotic (3 × 1010 probiotic capsules containing nine Lactobacillus and five Bifidobacterium species) and placebo control groups (containing polysaccharide supplied in an identical bottle) 3 times daily/6 weeks. A short inflammatory bowel disease questionnaire (SIBDQ) was used to assess the change in the quality of life in both groups at the beginning and the end of the intervention; The study was completed during the COVID-19 pandemic.
Results
Patients treated with probiotics showed a higher score of social (6.92 ± 0.29, p = 0.019), bowel (6.31 ± 0.46, p = 0.001), emotional (6.47 ± 0.46, p < 0.001), and total SIBDQ scores (6.54 ± 0.29, p < 0.001) compared to the placebo group (5.75 ± 1.57, 4.72 ± 1.34, 4.42 ± 1.67 and 4.96 ± 1.27; respectively). Also, the probiotic group had significantly better scores in the systemic, social, bowel, emotional, and total SIBDQ scores in terms of pre- to post-treatment (p < 0.001).
Conclusions
The use of probiotic therapy containing Lactobacillus and Bifidobacterium species had significantly improved the quality of life among UC patients, this was shown by the improvement in the scores of the systemic domain, social domain, bowel domain, emotional domain, and total SIBDQ. This study is part of a registered study at ClinicalTrials.gov with the number NCT04223479.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available upon reasonable request.
Abbreviations
- 5-ASA:
-
5-Aminosalicylic acid
- CD:
-
Crohn’s disease
- HRQoL:
-
Health-related quality of life
- IBD:
-
Inflammatory bowel disease
- IBDQ:
-
Inflammatory Bowel Disease Questionnaire
- ITT:
-
Intention-to-treat
- PMS:
-
Partial Mayo Score
- PP:
-
Per-protocol
- QoL:
-
Quality of life
- SIBDQ:
-
Short Inflammatory Bowel Disease Questionnaire
- UC:
-
Ulcerative colitis
References
Guan Q (2019) A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. https://doi.org/10.1155/2019/7247238
Kaplan GG, Windsor JW (2021) The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol 18(1):56–66
Sairenji T, Collins KL, Evans DV (2017) An update on inflammatory bowel disease. Prim Care 44(4):673–692
Alatab S, Sepanlou SG, Ikuta K, Vahedi H, Bisignano C, Safiri S, Sadeghi A, Nixon MR, Abdoli A, Abolhassani H (2020) The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 5(1):17–30
Omran S, Barakat H, Muliira JK, McMillan S (2017) Dietary and lifestyle risk factors for colorectal cancer in apparently healthy adults in Jordanian hospitals. J Cancer Educ 32:447–453
Kemp K, Griffiths J, Lovell K (2012) Understanding the health and social care needs of people living with IBD: a meta-synthesis of the evidence. World J Gastroenterol 18(43):6240
Jones JL, Nguyen GC, Benchimol EI, Bernstein CN, Bitton A, Kaplan GG, Murthy SK, Lee K, Cooke-Lauder J, Otley AR (2019) The impact of inflammatory bowel disease in Canada 2018: quality of life. J Can Assoc Gastroenterol 2(Supplement_1):S42–S48
Sajadinejad MS, Asgari K, Molavi H, Kalantari M, Adibi P (2012) Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. https://doi.org/10.1155/2012/106502
Knowles SR, Graff LA, Wilding H, Hewitt C, Keefer L, Mikocka-Walus A (2018) Quality of life in inflammatory bowel disease: a systematic review and meta-analyses—part I. Inflamm Bowel Dis 24(4):742–751
Byrne G, Rosenfeld G, Leung Y, Qian H, Raudzus J, Nunez C, Bressler B (2017) Prevalence of anxiety and depression in patients with inflammatory bowel disease. Can J Gastroenterol Hepatol. https://doi.org/10.1155/2017/6496727
Choi K, Chun J, Han K, Park S, Soh H, Kim J, Lee J, Lee HJ, Im JP, Kim JS (2019) Risk of anxiety and depression in patients with inflammatory bowel disease: a nationwide, population-based study. J Clin Med 8(5):654
Mikocka-Walus A, Knowles SR, Keefer L, Graff L (2016) Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis 22(3):752–762
Zahn A, Hinz U, Karner M, Ehehalt R, Stremmel W (2006) Health-related quality of life correlates with clinical and endoscopic activity indexes but not with demographic features in patients with ulcerative colitis. Inflamm Bowel Dis 12(11):1058–1067
Haapamäki J, Turunen U, Roine RP, Färkkilä MA, Arkkila PE (2009) Impact of demographic factors, medication and symptoms on disease-specific quality of life in inflammatory bowel disease. Qual Life Res 18:961–969
Klag T, Mazurak N, Fantasia L, Schwille-Kiuntke J, Kirschniak A, Falch C, Goetz M, Malek NP, Enck P, Wehkamp J (2017) High demand for psychotherapy in patients with inflammatory bowel disease. Inflamm Bowel Dis 23(10):1796–1802
Kutschera M, Waldhör T, Gröchenig H, Haas T, Wenzl H, Steiner P, Koch R, Feichtenschlager T, Eckhardt G, Mayer A (2020) P308 The need for psychological and psychotherapeutic interventions in Austrian patients with inflammatory bowel disease. J Crohn’s Colitis 14(Supplement_1):S308–S309
Lores T, Goess C, Mikocka-Walus A, Collins KL, Burke AL, Chur-Hansen A, Delfabbro P, Andrews JM (2021) Integrated psychological care reduces health care costs at a hospital-based inflammatory bowel disease service. Clin Gastroenterol Hepatol 19(1):96–103 (e103)
Ağagündüz D, Gençer Bingöl F, Çelik E, Cemali Ö, Özenir Ç, Özoğul F, Capasso R (2022) Recent developments in the probiotics as live biotherapeutic products (LBPs) as modulators of gut brain axis related neurological conditions. J Transl Med 20(1):460
Ağagündüz D, Kocaadam-Bozkurt B, Bozkurt O, Sharma H, Esposito R, Özoğul F, Capasso R (2022) Microbiota alteration and modulation in Alzheimer’s disease by gerobiotics: the gut-health axis for a good mind. Biomed Pharmacother 153:113430
Celiberto LS, Bedani R, Rossi EA, Cavallini DCU (2017) Probiotics: the scientific evidence in the context of inflammatory bowel disease. Crit Rev Food Sci Nutr 57(9):1759–1768
Food, Organization AOWH (2001) Report of a joint FAO/WHO expert consultation on evaluation of health and nutritional properties of probiotics in food including powder milk with live lactic acid bacteria. FAO/WHO Cordoba, Argentina
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S (2014) Expert consensus document: the International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. https://doi.org/10.1038/nrgastro.2014.66
Javanmard A, Ashtari S, Sabet B, Davoodi SH, Rostami-Nejad M, Akbari ME, Niaz A, Mortazavian AM (2018) Probiotics and their role in gastrointestinal cancers prevention and treatment; an overview. Gastroenterol Hepatol Bed Bench 11(4):284
Grumezescu AM, Holban AM (2018) Diet, microbiome and health, vol 11. Academic Press
Markowiak P, Śliżewska K (2017) Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients 9(9):1021
Sánchez B, Delgado S, Blanco-Míguez A, Lourenço A, Gueimonde M, Margolles A (2017) Probiotics, gut microbiota, and their influence on host health and disease. Mol Nutr Food Res 61(1):1600240
Shokryazdan P, Faseleh Jahromi M, Liang JB, Ho YW (2017) Probiotics: from isolation to application. J Am College Nutr 36(8):666–676
Fong FLY, Shah NP, Kirjavainen P, El-Nezami H (2016) Mechanism of action of probiotic bacteria on intestinal and systemic immunities and antigen-presenting cells. Int Rev Immunol 35(3):179–188
Bibiloni R, Fedorak RN, Tannock GW, Madsen KL, Gionchetti P, Campieri M, De Simone C, Sartor RB (2005) VSL# 3 probiotic-mixture induces remission in patients with active ulcerative colitis. Offic J Am College Gastroenterol 100(7):1539–1546
Fujimori S, Gudis K, Mitsui K, Seo T, Yonezawa M, Tanaka S, Tatsuguchi A, Sakamoto C (2009) A randomized controlled trial on the efficacy of synbiotic versus probiotic or prebiotic treatment to improve the quality of life in patients with ulcerative colitis. Nutrition 25(5):520–525
Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A (2009) Effect of a probiotic preparation (VSL# 3) on induction and maintenance of remission in children with ulcerative colitis. Offic J Am College Gastroenterol 104(2):437–443
Van Der Geest A, Besseling-Van der Vaart I, Schellinger-de Goede E, Van der Waal M, Claassen E, Flach J, Van de Burgwal L (2021) Multispecies probiotics promote perceived human health and wellbeing: insights into the value of retrospective studies on user experiences. Benef Microbes 12(5):413–430
Dhillon P, Singh K (2020) Therapeutic applications of probiotics in ulcerative colitis: an updated review. PharmaNutrition 13:100194
Gionchetti P, Rizzello F, Helwig U, Venturi A, Lammers KM, Brigidi P, Vitali B, Poggioli G, Miglioli M, Campieri M (2003) Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology 124(5):1202–1209
Haddad MA, Yamani M, Abu-Alruz K (2015) Development of a Probiotic Soft White Jordanian Cheese. Am-Eurasian J Agric Environ Sci Sci 15(7):1382–1391
AL-Awwad NJ, Takruri HR, Yamani MI (2014) Effect of probiotic hummus on blood lipids of rats. Jordan J Biol Sci 7(4):261–267
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JC, Chan FK (2017) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. The Lancet 390(10114):2769–2778
Palumbo VD, Romeo M, Marino Gammazza A, Carini F, Damiani P, Damiano G, Buscemi S, Ignazio A, Monte L, Gerges-Geagea A (2016) The long-term effects of probiotics in the therapy of ulcerative colitis: a clinical study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 160(3):372–377
Tamaki H, Nakase H, Inoue S, Kawanami C, Itani T, Ohana M, Kusaka T, Uose S, Hisatsune H, Tojo M (2016) Efficacy of probiotic treatment with Bifidobacterium longum 536 for induction of remission in active ulcerative colitis: a randomized, double-blinded, placebo-controlled multicenter trial. Dig Endosc 28(1):67–74
Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH (2008) Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis 14(12):1660–1666
Fuller R (1989) Probiotics in man and animals. J Appl Bacteriol 66(5):365–378
Sood A, Midha V, Makharia GK, Ahuja V, Singal D, Goswami P, Tandon RK (2009) The probiotic preparation, VSL# 3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clin Gastroenterol Hepatol 7(11):1202–1209 (e1201)
Tursi A, Brandimarte G, Papa A, Giglio A, Elisei W, Giorgetti GM, Forti G, Morini S, Hassan C, Pistoia MA (2010) Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL# 3 as adjunctive to standard pharmaceutical treatment: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 105(10):2218
Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS Jr (1985) Physical activity assessment methodology in the Five-City Project. Am J Epidemiol 121(1):91–106
Mahalli AA, Alharthi HM (2017) Assessment of health-related quality of life of patients with inflammatory bowel diseases in Eastern Province, Saudi Arabia. J Infect Public Health 10(1):93–101
Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, Tompkins C (1989) A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 96(2):804–810
Agraib LM, Yamani MI, Tayyem R, Abu-Sneineh AT, Rayyan YM (2022) Probiotic supplementation induces remission and changes in the immunoglobulins and inflammatory response in active ulcerative colitis patients: a pilot, randomized, double-blind, placebo-controlled study. Clin Nutr ESPEN 51:83–91
Yoshimatsu Y, Yamada A, Furukawa R, Sono K, Osamura A, Nakamura K, Aoki H, Tsuda Y, Hosoe N, Takada N (2015) Effectiveness of probiotic therapy for the prevention of relapse in patients with inactive ulcerative colitis. World J Gastroenterol 21(19):5985
Kato K, Mizuno S, Umesaki Y, Ishii Y, Sugitani M, Imaoka A, Otsuka M, Hasunuma O, Kurihara R, Iwasaki A (2004) Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment Pharmacol Ther 20(10):1133–1141
Lee J, Park SB, Kim HW, Lee HS, Jee SR, Lee JH, Kim TO (2022) Clinical efficacy of probiotic therapy on bowel-related symptoms in patients with ulcerative colitis during endoscopic remission: an observational study. Gastroenterol Res Pract. https://doi.org/10.1155/2022/9872230
Agrawal M, Colombel J-F (2019) Treat-to-target in inflammatory bowel diseases, what is the target and how do we treat? Gastrointest Endosc Clin 29(3):421–436
van der Waal MB, Flach J, Browne PD, Besseling-van der Vaart I, Claassen E, van de Burgwal LH (2019) Probiotics for improving quality of life in ulcerative colitis: exploring the patient perspective. Pharma Nutr 7:100139
Bjarnason I, Sission G, Hayee BH (2019) A randomised, double-blind, placebo-controlled trial of a multi-strain probiotic in patients with asymptomatic ulcerative colitis and Crohn’s disease. Inflammopharmacology 27:465–473
Acknowledgements
We would like to thank the University of Jordan for its support, The medical staff of The Jordan University Hospital, and Al-Bashir Hospital for extending support and help. Also, we would like to thank the Al-Farabi drug store for its collaboration in providing the probiotics product.
Funding
This work was supported by the Deanship of Scientific Research of the University of Jordan.
Author information
Authors and Affiliations
Contributions
YMR and LMA data acquisition, statistical analysis, interpreted the results, and analysis of the data. YMR, LMA, and BA inducted and drafted the manuscript. MIY, YMR, and ATA-S were involved in the concept and design of the study, analyzed the data, and reviewed and provided inputs on the manuscript. All authors critically revised the manuscript, approved the final version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was approved by The Institutional Board Review Committee and reviewed at The University of Jordan and Jordan University Hospital (No. 49/2019/3740). This study is part of a registered study at ClinicalTrials.gov with the number NCT04223479.
Consent to participate
All participants were informed about the study objectives at the beginning of the questionnaire, then they expressed their informed consent to participate, and their data were anonymous.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rayyan, Y.M., Agraib, L.M., Alkhatib, B. et al. Does probiotic supplementation improve quality of life in mild-to-moderately active ulcerative colitis patients in Jordan? A secondary outcome of the randomized, double-blind, placebo-controlled study. Eur J Nutr 62, 3069–3077 (2023). https://doi.org/10.1007/s00394-023-03207-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03207-8