Abstract
Purpose
Diet pattern (DP) is a key modifiable and cost-effective factor in hypertension (HTN) management. The current study aimed to identify and compare the hypertension-protective DPs among Chinese adults.
Methods
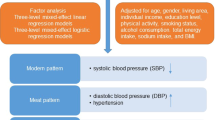
52,648 participants aged over 18 years were included from China Nutrition and Health Surveillance (CNHS) 2015–2017. Reduced rank regression (RRR) and partial least square regression (PLS) was applied to identify the DPs. Multivariable-adjusted logistic regression was used to assess the association between the DPs and HTN.
Results
DPs derived by RRR and PLS were both featured by higher consumption of fresh vegetables and fruits, mushrooms and edible fungi, seaweeds, soybeans and related products, mixed legumes, dairy products, fresh eggs, and lower of refined grain consumption. Compared to the lowest quintile, participants in the highest quintile had lower odds of HTN (RRR-DP: OR = 0.77, 95% CI = 0.72–0.83; PLS-DP: OR = 0.76, 95% CI = 0.71–0.82; all p < 0.0001). Simplified DP scores were observed the same protective tendencies (Simplified RRR-DP: OR = 0.81, 95% CI = 0.75–0.87; Simplified PLS-DP: OR = 0.79, 95% CI = 0.74–0.85; all p < 0.0001) and showed effective extrapolation in subgroups defined by gender, age, location, lifestyle, and different metabolic conditions.
Conclusions
The identified DPs had high conformity with East Asian dietary habits, and significantly negative associations with HTN among Chinese adults. The simplified DP technique also indicated the potential for improving the extrapolation of the results of DP analysis related to HTN.





Similar content being viewed by others
Availability of data and materials
According to the confidentiality provisions of the National Institute for Nutrition and Health, China CDC, the data of CNHS 2015–2017 are not allowed to be accessed without official permission.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- CNHS:
-
China nutrition and health surveillance
- CNY:
-
Chinese yuan
- CVD:
-
Cardiovascular disease
- DASH:
-
Dietary approach to stop hypertension
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- DP:
-
Dietary pattern
- DRIs:
-
Dietary reference intakes
- FFQ:
-
Food frequency questionnaire
- HDL-C:
-
High density lipoprotein-cholesterol
- HTN:
-
Hypertension
- LDL-C:
-
Low density lipoprotein-cholesterol
- LMIC:
-
Low- and middle-income country
- MUFA:
-
Monounsaturated fatty acids
- NCD:
-
Non-communicable disease
- OR:
-
Odds ratio
- PLS:
-
Partial least square
- PUFA:
-
Polyunsaturated fatty acid
- RCS:
-
Restricted cubic splines
- RCT:
-
Randomized controlled trial
- RRR:
-
Reduced rank regression
- SBP:
-
Systolic blood pressure
- SFA:
-
Saturated fatty acid
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
References
Mills KT, Stefanescu A, He J (2020) The global epidemiology of hypertension. Nat Rev Nephrol 16(4):223–237. https://doi.org/10.1038/s41581-019-0244-2
Katalambula LK, Meyer DN, Ngoma T, Buza J, Mpolya E, Mtumwa AH, Petrucka P (2017) Dietary pattern and other lifestyle factors as potential contributors to hypertension prevalence in Arusha City, Tanzania: a population-based descriptive study. BMC Public Health 17(1):659. https://doi.org/10.1186/s12889-017-4679-8
Park JE, Jung H, Lee JE (2014) Dietary pattern and hypertension in Korean adults. Public Health Nutr 17(3):597–606. https://doi.org/10.1017/S1368980013000219
Shen Y, Chang C, Zhang J, Jiang Y, Ni B, Wang Y (2017) Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: a cross-sectional study. Environ Health Prev Med 22(1):19. https://doi.org/10.1186/s12199-017-0634-7
Yi Q, Zha M, Yang Q, Zhang Y, Hou L, Ye X, Chen G, Shao J, Xia W, Song P (2021) Trends in the prevalence of hypertension according to severity and phenotype in Chinese adults over two decades (1991–2015). J Clin Hypertens (Greenwich) 23(7):1302–1315. https://doi.org/10.1111/jch.14306
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, Su M, Zhao H, Spatz ES, Spertus JA, Masoudi FA, Krumholz HM, Jiang L (2017) Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 390(10112):2549–2558. https://doi.org/10.1016/S0140-6736(17)32478-9
Sun Y, Mu J, Wang DW, Ouyang N, Xing L, Guo X, Zhao C, Ren G, Ye N, Zhou Y, Wang J, Li Z, Sun G, Yang R, Chen CS, He J, Group CS (2022) A village doctor-led multifaceted intervention for blood pressure control in rural China: an open, cluster randomised trial. Lancet 399(10339):1964–1975. https://doi.org/10.1016/S0140-6736(22)00325-7
Widmer RJ, Flammer AJ, Lerman LO, Lerman A (2015) The Mediterranean diet, its components, and cardiovascular disease. Am J Med 128(3):229–238. https://doi.org/10.1016/j.amjmed.2014.10.014
Yi SY, Steffen LM, Haring B, Rebholz CM, Mosley TH, Shah AM (2021) Associations of the Dietary Approaches to Stop Hypertension dietary pattern with cardiac structure and function. Nutr Metab Cardiovasc Dis 31(12):3345–3351. https://doi.org/10.1016/j.numecd.2021.08.050
Xiao X, Qin Z, Lv X, Dai Y, Ciren Z, Yangla Y, Zeng P, Ma Y, Li X, Wang L, Hu Y, Yang F, Fan C, Tang D, Dai S, Zhang N, Xie X, Yin J, Zhao X (2021) Dietary patterns and cardiometabolic risks in diverse less-developed ethnic minority regions: results from the China Multi-Ethnic Cohort (CMEC) Study. Lancet Reg Health West Pac 15:100252. https://doi.org/10.1016/j.lanwpc.2021.100252
Wang Y, Feng L, Zeng G, Zhu H, Sun J, Gao P, Yuan J, Lan X, Li S, Zhao Y, Chen X, Dong H, Chen S, Li Z, Zhu Y, Li M, Li X, Yang Z, Li H, Fang H, Xie G, Lin PH, Chen J, Wu Y (2022) Effects of cuisine-based chinese heart-healthy diet in lowering blood pressure among adults in china: multicenter, single-blind, randomized, parallel controlled feeding trial. Circulation 146(4):303–315. https://doi.org/10.1161/CIRCULATIONAHA.122.059045
Lee SA, Cai H, Yang G, Xu WH, Zheng W, Li H, Gao YT, Xiang YB, Shu XO (2010) Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br J Nutr 104(2):265–275. https://doi.org/10.1017/S0007114510000383
Wang D, He Y, Li Y, Luan D, Yang X, Zhai F, Ma G (2011) Dietary patterns and hypertension among Chinese adults: a nationally representative cross-sectional study. BMC Public Health 11:925. https://doi.org/10.1186/1471-2458-11-925
Hoffmann K, Schulze MB, Schienkiewitz A, Nothlings U, Boeing H (2004) Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am J Epidemiol 159(10):935–944. https://doi.org/10.1093/aje/kwh134
Kurniawan AL, Hsu CY, Lee HA, Rau HH, Paramastri R, Syauqy A, Chao JC (2020) Comparing two methods for deriving dietary patterns associated with risk of metabolic syndrome among middle-aged and elderly Taiwanese adults with impaired kidney function. BMC Med Res Methodol 20(1):255. https://doi.org/10.1186/s12874-020-01142-4
Schulze MB, Hoffmann K, Kroke A, Boeing H (2003) An approach to construct simplified measures of dietary patterns from exploratory factor analysis. Br J Nutr 89(3):409–419. https://doi.org/10.1079/BJN2002778
Lazarova SV, Jessri M (2022) Associations between dietary patterns and cardiovascular disease risk in Canadian adults: a comparison of partial least squares, reduced rank regression, and the simplified dietary pattern technique. Am J Clin Nutr 116(2):362–377. https://doi.org/10.1093/ajcn/nqac117
Ng AP, Jessri M, L’Abbe MR (2021) Using partial least squares to identify a dietary pattern associated with obesity in a nationally-representative sample of Canadian adults: Results from the Canadian Community Health Survey-Nutrition 2015. PLoS ONE 16(8):e0255415. https://doi.org/10.1371/journal.pone.0255415
He Y, Zhao W, Zhang J, Zhao L, Yang Z, Huo J, Yang L, Wang J, He L, Sun J, Piao J, Yang X, Ge K, Ding G (2019) Data resource profile: china national nutrition surveys. Int J Epidemiol 48(2):368–368f. https://doi.org/10.1093/ije/dyy289
Yu D, Zhao L, Zhang J, Yang Z, Yang L, Huang J, Fang H, Guo Q, Xu X, Ju L, Ding G (2021) China nutrition and health surveys (1982–2017). China CDC Wkly 3(9):193–195. https://doi.org/10.46234/ccdcw2021.058
Yang Y, Yu D, Piao W, Huang K, Zhao L (2022) Nutrient-derived beneficial for blood pressure dietary pattern associated with hypertension prevention and control: based on china nutrition and health surveillance 2015–2017. Nutrients 14(15):3108. https://doi.org/10.3390/nu14153108
Chau CA, Pan WH, Chen HJ (2017) Employment status and temporal patterns of energy intake: Nutrition and Health Survey in Taiwan, 2005–2008. Public Health Nutr 20(18):3295–3303. https://doi.org/10.1017/S1368980017002476
Zhao W-H, Huang Z-P, Zhang X, He L, Willett W, Wang J-L, Hasegawa K, Chen J-S (2010) Reproducibility and validity of a Chinese food frequency questionnaire. Biomed Environ Sci 23:1–38. https://doi.org/10.1016/S0895-3988(11)60014-7
Yang YX (2018) China food composition table, standard edition. Peking University Medical Press, Beijing
Yang YX, Wang GY, Pan XC (2009) China food composition tables, 2nd edition. Peking University Medical Press, Beijing
Chinese Nutrition Society (2022) Dietary guidelines for Chinese Residents. People’s Medical Publishing House, Beijing, pp 343–344
Liang J, Zhao JK, Wang JP, Wang T (2021) Association between animal source foods consumption and risk of hypertension: a cohort study. Eur J Nutr 60(5):2469–2483. https://doi.org/10.1007/s00394-020-02423-w
Ning G, Bloomgarden Z (2013) Diabetes in China: prevalence, diagnosis, and control. J Diabetes 5(4):372. https://doi.org/10.1111/1753-0407.12088
Lu Y, Zhang H, Lu J, Ding Q, Li X, Wang X, Sun D, Tan L, Mu L, Liu J, Feng F, Yang H, Zhao H, Schulz WL, Krumholz HM, Pan X, Li J, China Patient-Centered Evaluative Assessment of Cardiac Events Million Persons Project Collaborative G (2021) Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China. JAMA Netw Open 4(9):e2127573. https://doi.org/10.1001/jamanetworkopen.2021.27573
Shakya PR, Melaku YA, Page A, Gill TK (2020) Association between dietary patterns and adult depression symptoms based on principal component analysis, reduced-rank regression and partial least-squares. Clin Nutr 39(9):2811–2823. https://doi.org/10.1016/j.clnu.2019.12.011
Bahari T, Uemura H, Katsuura-Kamano S, Yamaguchi M, Nakamoto M, Miki K, Ishizu M, Arisawa K (2018) Nutrient-derived dietary patterns and their association with metabolic syndrome in a japanese population. J Epidemiol 28(4):194–201. https://doi.org/10.2188/jea.JE20170010
Zheng B, Liu Q, Lyu J, Yu CQ (2022) Introduction of reduced rank regression and development of a user-written Stata package. Zhonghua Liu Xing Bing Xue Za Zhi 43(3):403–408. https://doi.org/10.3760/cma.j.cn112338-20210222-00136
Aleixandre A, Miguel M (2016) Dietary fiber and blood pressure control. Food Funct 7(4):1864–1871. https://doi.org/10.1039/c5fo00950b
Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A, Waters V, Williams CL (2009) Health benefits of dietary fiber. Nutr Rev 67(4):188–205. https://doi.org/10.1111/j.1753-4887.2009.00189.x
Cormick G, Ciapponi A, Cafferata ML, Cormick MS, Belizan JM (2021) Calcium supplementation for prevention of primary hypertension. Cochrane Database Syst Rev 8:CD010037. https://doi.org/10.1002/14651858.CD010037.pub3
DiNicolantonio JJ, Liu J, O’Keefe JH (2018) Thiamine and cardiovascular disease: a literature review. Prog Cardiovasc Dis 61(1):27–32. https://doi.org/10.1016/j.pcad.2018.01.009
Duc HN, Oh H, Yoon IM, Kim MS (2021) Association between levels of thiamine intake, diabetes, cardiovascular diseases and depression in Korea: a national cross-sectional study. J Nutr Sci 10:e31. https://doi.org/10.1017/jns.2021.23
Morelli MB, Gambardella J, Castellanos V, Trimarco V, Santulli G (2020) Vitamin C and cardiovascular disease: an update. Antioxidants (Basel) 9(12):1227. https://doi.org/10.3390/antiox9121227
Thakur K, Tomar SK, Singh AK, Mandal S, Arora S (2017) Riboflavin and health: a review of recent human research. Crit Rev Food Sci Nutr 57(17):3650–3660. https://doi.org/10.1080/10408398.2016.1145104
Volpe SL (2013) Magnesium in disease prevention and overall health. Adv Nutr 4(3):378S-383S. https://doi.org/10.3945/an.112.003483
Weaver CM (2013) Potassium and health. Adv Nutr 4(3):368S-377S. https://doi.org/10.3945/an.112.003533
Miki T, Kochi T, Kuwahara K, Eguchi M, Kurotani K, Tsuruoka H, Ito R, Kabe I, Kawakami N, Mizoue T, Nanri A (2015) Dietary patterns derived by reduced rank regression (RRR) and depressive symptoms in Japanese employees: the Furukawa nutrition and health study. Psychiatry Res 229(1–2):214–219. https://doi.org/10.1016/j.psychres.2015.07.033
Skipina TM, Soliman EZ, Upadhya B (2020) Association between secondhand smoke exposure and hypertension: nearly as large as smoking. J Hypertens 38(10):1899–1908. https://doi.org/10.1097/HJH.0000000000002478
Beunza JJ, Martinez-Gonzalez MA, Ebrahim S, Bes-Rastrollo M, Nunez J, Martinez JA, Alonso A (2007) Sedentary behaviors and the risk of incident hypertension: the SUN Cohort. Am J Hypertens 20(11):1156–1162. https://doi.org/10.1016/j.amjhyper.2007.06.007
Liss DT, Uchida T, Wilkes CL, Radakrishnan A, Linder JA (2021) General health checks in adult primary care: a review. JAMA 325(22):2294–2306. https://doi.org/10.1001/jama.2021.6524
Zhao L, Stamler J, Yan LL, Zhou B, Wu Y, Liu K, Daviglus ML, Dennis BH, Elliott P, Ueshima H, Yang J, Zhu L, Guo D, Group IR (2004) Blood pressure differences between northern and southern Chinese: role of dietary factors: the International Study on Macronutrients and Blood Pressure. Hypertension 43(6):1332–1337. https://doi.org/10.1161/01.HYP.0000128243.06502.bc
Mu L, Liu J, Zhou G, Wu C, Chen B, Lu Y, Lu J, Yan X, Zhu Z, Nasir K, Spatz ES, Krumholz HM, Zheng X (2021) Obesity prevalence and risks among chinese adults: findings from the China PEACE million persons project, 2014–2018. Circ Cardiovasc Qual Outcomes 14(6):e007292. https://doi.org/10.1161/CIRCOUTCOMES.120.007292
Wang M, Huang Y, Song Y, Chen J, Liu X (2021) Study on environmental and lifestyle factors for the north-south differential of cardiovascular disease in China. Front Public Health 9:615152. https://doi.org/10.3389/fpubh.2021.615152
Yao F, Bo Y, Zhao L, Li Y, Ju L, Fang H, Piao W, Yu D, Lao X (2021) Prevalence and influencing factors of metabolic syndrome among adults in China from 2015 to 2017. Nutrients 13(12):4475. https://doi.org/10.3390/nu13124475
Fan M, Lyu J, He P (2014) Chinese guidelines for data processing and analysis concerning the International Physical Activity Questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi 35(8):961–964
Glenn AJ, Hernandez-Alonso P, Kendall CWC, Martinez-Gonzalez MA, Corella D, Fito M, Martinez JA, Alonso-Gomez AM, Warnberg J, Vioque J, Romaguera D, Lopez-Miranda J, Estruch R, Tinahones FJ, Lapetra J, Serra-Majem JL, Bueno-Cavanillas A, Tur JA, Celada SR, Pinto X, Delgado-Rodriguez M, Matia-Martin P, Vidal J, Mas-Fontao S, Daimiel L, Ros E, Jenkins DJA, Toledo E, Sorli JV, Castaner O, Abete I, Rodriguez AM, Barcelo OF, Oncina-Canovas A, Konieczna J, Garcia-Rios A, Casas R, Gomez-Perez AM, Santos-Lozano JM, Vazquez-Ruiz Z, Portoles O, Schroder H, Zulet MA, Eguaras S, Lete IS, Zomeno MD, Sievenpiper JL, Salas-Salvado J (2021) Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study. Clin Nutr 40(5):2825–2836. https://doi.org/10.1016/j.clnu.2021.03.016
DiBello JR, Kraft P, McGarvey ST, Goldberg R, Campos H, Baylin A (2008) Comparison of 3 methods for identifying dietary patterns associated with risk of disease. Am J Epidemiol 168(12):1433–1443. https://doi.org/10.1093/aje/kwn274
Shimazu T, Kuriyama S, Hozawa A, Ohmori K, Sato Y, Nakaya N, Nishino Y, Tsubono Y, Tsuji I (2007) Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int J Epidemiol 36(3):600–609. https://doi.org/10.1093/ije/dym005
Zheng PF, Shu L, Zhang XY, Si CJ, Yu XL, Gao W, Tong XQ, Zhang L (2016) Association between dietary patterns and the risk of hypertension among Chinese: a cross-sectional study. Nutrients 8(4):239. https://doi.org/10.3390/nu8040239
Sadler MJ, Gibson S, Whelan K, Ha MA, Lovegrove J, Higgs J (2019) Dried fruit and public health—what does the evidence tell us? Int J Food Sci Nutr 70(6):675–687. https://doi.org/10.1080/09637486.2019.1568398
Alasalvar C, Salvado JS, Ros E (2020) Bioactives and health benefits of nuts and dried fruits. Food Chem 314:126192. https://doi.org/10.1016/j.foodchem.2020.126192
Peng Y, Dong B, Wang Z (2016) Serum folate concentrations and all-cause, cardiovascular disease and cancer mortality: a cohort study based on 1999–2010 National Health and Nutrition Examination Survey (NHANES). Int J Cardiol 219:136–142. https://doi.org/10.1016/j.ijcard.2016.06.024
Liang Q, Wang K, Shariful I, Ye X, Zhang C (2020) Folate content and retention in wheat grains and wheat-based foods: effects of storage, processing, and cooking methods. Food Chem 333:127459. https://doi.org/10.1016/j.foodchem.2020.127459
Selem SS, Castro MA, Cesar CL, Marchioni DM, Fisberg RM (2014) Associations between dietary patterns and self-reported hypertension among Brazilian adults: a cross-sectional population-based study. J Acad Nutr Diet 114(8):1216–1222. https://doi.org/10.1016/j.jand.2014.01.007
Weber KS, Knebel B, Strassburger K, Kotzka J, Stehle P, Szendroedi J, Mussig K, Buyken AE, Roden M, Group GDS (2016) Associations between explorative dietary patterns and serum lipid levels and their interactions with ApoA5 and ApoE haplotype in patients with recently diagnosed type 2 diabetes. Cardiovasc Diabetol 15(1):138. https://doi.org/10.1186/s12933-016-0455-9
American Heart Association Nutrition C, Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J (2006) Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 114(1):82–96. https://doi.org/10.1161/CIRCULATIONAHA.106.176158
de Oliveira Otto MC, Mozaffarian D, Kromhout D, Bertoni AG, Sibley CT, Jacobs DR Jr, Nettleton JA (2012) Dietary intake of saturated fat by food source and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr 96(2):397–404. https://doi.org/10.3945/ajcn.112.037770
Unger AL, Torres-Gonzalez M, Kraft J (2019) Dairy fat consumption and the risk of metabolic syndrome: an examination of the saturated fatty acids in dairy. Nutrients 11(9):2200. https://doi.org/10.3390/nu11092200
Yuan M, Singer MR, Pickering RT, Moore LL (2022) Saturated fat from dairy sources is associated with lower cardiometabolic risk in the Framingham Offspring Study. Am J Clin Nutr 116(6):1682–1692. https://doi.org/10.1093/ajcn/nqac224
Nakamura H, Tsujiguchi H, Kambayashi Y, Hara A, Miyagi S, Yamada Y, Nguyen TTT, Shimizu Y, Hori D, Nakamura H (2019) Relationship between saturated fatty acid intake and hypertension and oxidative stress. Nutrition 61:8–15. https://doi.org/10.1016/j.nut.2018.10.020
Naja F, Itani L, Hwalla N, Sibai AM, Kharroubi SA (2019) Identification of dietary patterns associated with elevated blood pressure among Lebanese men: a comparison of principal component analysis with reduced rank regression and partial least square methods. PLoS ONE 14(8):e0220942. https://doi.org/10.1371/journal.pone.0220942
Hoffmann K, Zyriax BC, Boeing H, Windler E (2004) A dietary pattern derived to explain biomarker variation is strongly associated with the risk of coronary artery disease. Am J Clin Nutr 80(3):633–640. https://doi.org/10.1093/ajcn/80.3.633
Seah JYH, Ong CN, Koh WP, Yuan JM, van Dam RM (2019) A dietary pattern derived from reduced rank regression and fatty acid biomarkers is associated with lower risk of type 2 diabetes and coronary artery disease in chinese adults. J Nutr 149(11):2001–2010. https://doi.org/10.1093/jn/nxz164
Nazari SSH, Mokhayeri Y, Mansournia MA, Khodakarim S, Soori H (2018) Associations between dietary risk factors and ischemic stroke: a comparison of regression methods using data from the Multi-Ethnic Study of Atherosclerosis. Epidemiol Health 40:e2018021. https://doi.org/10.4178/epih.e2018021
Wang D, Karvonen-Gutierrez CA, Jackson EA, Elliott MR, Appelhans BM, Barinas-Mitchell E, Bielak LF, Huang MH, Baylin A (2020) Western dietary pattern derived by multiple statistical methods is prospectively associated with subclinical carotid atherosclerosis in midlife women. J Nutr 150(3):579–591. https://doi.org/10.1093/jn/nxz270
Meyer J, Doring A, Herder C, Roden M, Koenig W, Thorand B (2011) Dietary patterns, subclinical inflammation, incident coronary heart disease and mortality in middle-aged men from the MONICA/KORA Augsburg cohort study. Eur J Clin Nutr 65(7):800–807. https://doi.org/10.1038/ejcn.2011.37
Jacobs S, Kroeger J, Schulze MB, Frank LK, Franke AA, Cheng I, Monroe KR, Haiman CA, Kolonel LN, Wilkens LR, Le Marchand L, Boushey CJ, Maskarinec G (2017) Dietary patterns derived by reduced rank regression are inversely associated with type 2 diabetes risk across 5 ethnic groups in the multiethnic cohort. Curr Dev Nutr 1(5):e000620. https://doi.org/10.3945/cdn.117.000620
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002
Newby PK, Tucker KL (2004) Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev 62(5):177–203. https://doi.org/10.1301/nr.2004.may.177-203
Ramezankhani A, Hosseini-Esfahani F, Mirmiran P, Azizi F, Hadaegh F (2021) The association of priori and posteriori dietary patterns with the risk of incident hypertension: Tehran Lipid and Glucose Study. J Transl Med 19(1):44. https://doi.org/10.1186/s12967-021-02704-w
Tiong XT, Nursara Shahirah A, Pun VC, Wong KY, Fong AYY, Sy RG, Castillo-Carandang NT, Nang EEK, Woodward M, van Dam RM, Tai ES, Venkataraman K (2018) The association of the dietary approach to stop hypertension (DASH) diet with blood pressure, glucose and lipid profiles in Malaysian and Philippines populations. Nutr Metab Cardiovasc Dis 28(8):856–863. https://doi.org/10.1016/j.numecd.2018.04.014
Wang F, Han L, Hu D (2017) Fasting insulin, insulin resistance and risk of hypertension in the general population: a meta-analysis. Clin Chim Acta 464:57–63. https://doi.org/10.1016/j.cca.2016.11.009
Xiao L, Harrison DG (2020) Inflammation in hypertension. Can J Cardiol 36(5):635–647. https://doi.org/10.1016/j.cjca.2020.01.013
Acknowledgements
We kindly thank all the CDC staffs, participants, and contributors involved in the preparation, investigation, data processing in CNHS 2015–2017.
Funding
This research was funded by Study of Diet and Nutrition Assessment and Intervention Technology (No.2020YFC2006300) from Active Health and Aging Technologic Solutions Major Project of National Key R&D Program; National Health Commission of the People’s Republic of China Medical Reform Major Program: China National Chronic Diseases and Nutrition Surveillance of Adults (2015–2017).
Author information
Authors and Affiliations
Contributions
Study concept and design: YY, LZ, and DY; acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: YY and DY; critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: YY and KH; administrative, technical, or material support: WP, LZ, and DY; study supervision: LZ and DY. LZ and DY contributed equally as corresponding co-authors. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Not applicable.
Ethics approval and consent to participate
CNHS 2015–2017 was approved by the Ethics Committee of National Institute for Nutrition and Health, CCDC (Protocol number: 201519-B, approved on 15/06/2015). All participants had signed informed consent before the study.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, Y., Piao, W., Cai, S. et al. Comparison of data-driven identified hypertension-protective dietary patterns among Chinese adults: based on a nationwide study. Eur J Nutr 62, 2805–2825 (2023). https://doi.org/10.1007/s00394-023-03195-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03195-9