Abstract
Purpose
Plant-based diets, particularly when rich in healthy plant foods, have been associated with a lower risk of type 2 diabetes and cardiovascular disease. However, the impact of plant-based diets that distinguish between healthy and unhealthy plant foods on cardiometabolic biomarkers remains unclear.
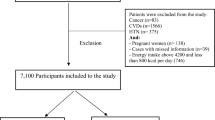
Methods
Dietary information was collected by two 24-h recalls among 34,785 adults from a nationwide cross-sectional study. Plasma levels of insulin, C-peptide, glucose, C-reactive protein (CRP), white blood cell (WBC) count, triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C) were measured. Linear regression was used to evaluate the percentage difference in plasma marker concentrations by three plant-based diet indices, namely the overall plant-based diet index (PDI), the healthful PDI (hPDI), and the unhealthful PDI (uPDI).
Results
Greater hPDI-adherence scores (comparing extreme quartiles) were associated with lower levels of insulin, Homeostatic Model Assessment of Insulin Resistance (HOMA-IR), TG/HDL-C ratio, CRP, WBC count, and TG, and higher levels of HDL-C, with the percentage differences of – 14.55, – 15.72, – 11.57, – 14.95, – 5.26, – 7.10, and 5.01, respectively (all Ptrend ≤ 0.001). Conversely, uPDI was associated with higher levels of insulin, C-peptide, HOMA-IR, TG/HDL-C ratio, CRP, WBC count, and TG, but lower HDL-C, with the percentage differences of 13.71, 14.00, 14.10, 10.43, 3.32, 8.00, and – 4.98 (all Ptrend ≤ 0.001), respectively. Overall PDI was only associated with lower levels of CRP and WBC count (all Ptrend ≤ 0.001).
Conclusion
Our findings suggest that hPDI may have positive, whereas uPDI may have negative impacts on multiple cardiometabolic risk markers, and underscore the need to consider the quality of plant foods in future PDI studies.
Similar content being viewed by others
Availability of data and material
Data described in the manuscript can be made publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm.
References
Baden MY, Liu G, Satija A, Li Y, Sun Q, Fung TT, Rimm EB, Willett WC, Hu FB, Bhupathiraju SN (2019) Changes in plant-based diet quality and total and cause-specific mortality. Circulation 140(12):979–991. https://doi.org/10.1161/CIRCULATIONAHA.119.041014
Kim J, Kim H, Giovannucci EL (2021) Plant-based diet quality and the risk of total and disease-specific mortality: a population-based prospective study. Clin Nutr 40(12):5718–5725. https://doi.org/10.1016/j.clnu.2021.10.013
Li H, Zeng X, Wang Y, Zhang Z, Zhu Y, Li X, Hu A, Zhao Q, Yang W (2022) A prospective study of healthful and unhealthful plant-based diet and risk of overall and cause-specific mortality. Eur J Nutr 61(1):387–398. https://doi.org/10.1007/s00394-021-02660-7
Chen Z, Drouin-Chartier JP, Li Y, Baden MY, Manson JE, Willett WC, Voortman T, Hu FB, Bhupathiraju SN (2021) Changes in plant-based diet indices and subsequent risk of type 2 diabetes in women and men: Three U.S. prospective cohorts. Diabetes Care 44(3):663–671. https://doi.org/10.2337/dc20-1636
Yang X, Li Y, Wang C, Mao Z, Chen Y, Ren P, Fan M, Cui S, Niu K, Gu R, Li L (2021) Association of plant-based diet and type 2 diabetes mellitus in Chinese rural adults: The Henan Rural Cohort Study. J Diabetes Investig 12(9):1569–1576. https://doi.org/10.1111/jdi.13522
Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, Willett WC, Manson JE, Sun Q, Hu FB (2016) Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med 13(6):e1002039. https://doi.org/10.1371/journal.pmed.1002039
Heianza Y, Zhou T, Sun D, Hu FB, Qi L (2021) Healthful plant-based dietary patterns, genetic risk of obesity, and cardiovascular risk in the UK biobank study. Clin Nutr 40(7):4694–4701. https://doi.org/10.1016/j.clnu.2021.06.018
Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, Rexrode KM, Rimm EB, Hu FB (2017) Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol 70(4):411–422. https://doi.org/10.1016/j.jacc.2017.05.047
Loeb S, Fu BC, Bauer SR, Pernar CH, Chan JM, Van Blarigan EL, Giovannucci EL, Kenfield SA, Mucci LA (2022) Association of plant-based diet index with prostate cancer risk. Am J Clin Nutr 115(3):662–670. https://doi.org/10.1093/ajcn/nqab365
Romanos-Nanclares A, Willett WC, Rosner BA, Collins LC, Hu FB, Toledo E, Eliassen AH (2021) Healthful and unhealthful plant-based diets and risk of breast cancer in U.S. women: results from the nurses’ health studies. Cancer Epidemiol Biomarkers Prev 30(10):1921–1931. https://doi.org/10.1158/1055-9965.EPI-21-0352
Willett W, Rockstrom J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood A, Jonell M, Clark M, Gordon LJ, Fanzo J, Hawkes C, Zurayk R, Rivera JA, De Vries W, Majele Sibanda L, Afshin A, Chaudhary A, Herrero M, Agustina R, Branca F, Lartey A, Fan S, Crona B, Fox E, Bignet V, Troell M, Lindahl T, Singh S, Cornell SE, Srinath Reddy K, Narain S, Nishtar S, Murray CJL (2019) Food in the anthropocene: the EAT-lancet commission on healthy diets from sustainable food systems. Lancet 393(10170):447–492. https://doi.org/10.1016/S0140-6736(18)31788-4
English LK, Ard JD, Bailey RL, Bates M, Bazzano LA, Boushey CJ, Brown C, Butera G, Callahan EH, de Jesus J, Mattes RD, Mayer-Davis EJ, Novotny R, Obbagy JE, Rahavi EB, Sabate J, Snetselaar LG, Stoody EE, Van Horn LV, Venkatramanan S, Heymsfield SB (2021) Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open 4(8):e2122277. https://doi.org/10.1001/jamanetworkopen.2021.22277
Schwingshackl L, Schwedhelm C, Hoffmann G, Lampousi AM, Knuppel S, Iqbal K, Bechthold A, Schlesinger S, Boeing H (2017) Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr 105(6):1462–1473. https://doi.org/10.3945/ajcn.117.153148
Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (2014) Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. https://doi.org/10.1136/bmj.g4490
Aune D, Norat T, Romundstad P, Vatten LJ (2013) Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol 28(11):845–858. https://doi.org/10.1007/s10654-013-9852-5
Muraki I, Rimm EB, Willett WC, Manson JE, Hu FB, Sun Q (2016) Potato consumption and risk of type 2 diabetes: results from three prospective cohort studies. Diabetes Care 39(3):376–384. https://doi.org/10.2337/dc15-0547
Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB (2014) Added sugar intake and cardiovascular diseases mortality among US adults. Jama Intern Med 174(4):516–524. https://doi.org/10.1001/jamainternmed.2013.13563
Li X, Zhang T, Li H, Zhou Z, Li M, Zeng X, Yang H, Zhang M, Huang Y, Zhu Y, Zhang Z, Ma Y, Yang W (2022) Associations between intake of starchy and non-starchy vegetables and risk of hepatic steatosis and fibrosis. Hepatol Int 16(4):846–857. https://doi.org/10.1007/s12072-022-10368-x
Kinlen LJ, Hermon C, Smith PG (1983) A proportionate study of cancer mortality among members of a vegetarian society. Br J Cancer 48(3):355–361. https://doi.org/10.1038/bjc.1983.200
Chang-Claude J, Frentzel-Beyme R, Eilber U (1992) Mortality pattern of German vegetarians after 11 years of follow-up. Epidemiology 3(5):395–401. https://doi.org/10.1097/00001648-199209000-00003
Key TJ, Thorogood M, Appleby PN, Burr ML (1996) Dietary habits and mortality in 11,000 vegetarians and health conscious people: results of a 17 year follow up. BMJ 313(7060):775–779. https://doi.org/10.1136/bmj.313.7060.775
Key TJ, Appleby PN, Davey GK, Allen NE, Spencer EA, Travis RC (2003) Mortality in British vegetarians: review and preliminary results from EPIC-Oxford. Am J Clin Nutr 78(3 Suppl):533s–538s. https://doi.org/10.1093/ajcn/78.3.533S
Orlich MJ, Singh PN, Sabate J, Jaceldo-Siegl K, Fan J, Knutsen S, Beeson WL, Fraser GE (2013) Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med 173(13):1230–1238. https://doi.org/10.1001/jamainternmed.2013.6473
Appleby PN, Crowe FL, Bradbury KE, Travis RC, Key TJ (2016) Mortality in vegetarians and comparable nonvegetarians in the United Kingdom. Am J Clin Nutr 103(1):218–230. https://doi.org/10.3945/ajcn.115.119461
Martinez-Gonzalez MA, Sanchez-Tainta A, Corella D, Salas-Salvado J, Ros E, Aros F, Gomez-Gracia E, Fiol M, Lamuela-Raventos RM, Schroder H, Lapetra J, Serra-Majem L, Pinto X, Ruiz-Gutierrez V, Estruch R, Group P (2014) A provegetarian food pattern and reduction in total mortality in the Prevencion con Dieta Mediterranea (PREDIMED) study. Am J Clin Nutr 100(Suppl 1):320S-328S. https://doi.org/10.3945/ajcn.113.071431
Baden MY, Satija A, Hu FB, Huang T (2019) Change in plant-based diet quality is associated with changes in plasma adiposity-associated biomarker concentrations in women. J Nutr 149(4):676–686. https://doi.org/10.1093/jn/nxy301
Pourreza S, Khademi Z, Mirzababaei A, Yekaninejad MS, Sadeghniiat-Haghighi K, Naghshi S, Mirzaei K (2021) Association of plant-based diet index with inflammatory markers and sleep quality in overweight and obese female adults: A cross-sectional study. Int J Clin Pract 75(9):e14429. https://doi.org/10.1111/ijcp.14429
Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) About the National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed 11 September 2021
Centers for Disease Control and Prevention.National Health and Nutrition Examination Survey (NHANES) Module 3: Weighting. https://wwwn.cdc.gov/nchs/nhanes/tutorials/module3.aspx. Accessed 16 November 2021
Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ (2006) The USDA automated multiple-pass method accurately estimates group total energy and nutrient intake. J Nutr 136(10):2594–2599. https://doi.org/10.1093/jn/136.10.2594
Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V (2006) A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc 106(10):1575–1587. https://doi.org/10.1016/j.jada.2006.07.003
Riccardi G, Giosue A, Calabrese I, Vaccaro O (2022) Dietary recommendations for prevention of atherosclerosis. Cardiovasc Res 118(5):1188–1204. https://doi.org/10.1093/cvr/cvab173
Schwingshackl L, Hoffmann G, Iqbal K, Schwedhelm C, Boeing H (2018) Food groups and intermediate disease markers: a systematic review and network meta-analysis of randomized trials. Am J Clin Nutr 108(3):576–586. https://doi.org/10.1093/ajcn/nqy151
Kim H, Lee K, Rebholz CM, Kim J (2020) Plant-based diets and incident metabolic syndrome: Results from a South Korean prospective cohort study. PLoS Med 17(11):e1003371. https://doi.org/10.1371/journal.pmed.1003371
Imamura F, Micha R, Wu JH, de Oliveira Otto MC, Otite FO, Abioye AI, Mozaffarian D (2016) Effects of saturated fat, polyunsaturated fat, monounsaturated fat, and carbohydrate on glucose-insulin homeostasis: a systematic review and meta-analysis of randomised controlled feeding trials. PLoS Med 13(7):e1002087. https://doi.org/10.1371/journal.pmed.1002087
Wang F, Baden MY, Hu FB (2022) Branding foods as “healthy” or “unhealthy” based on marginal data calls findings into question. Reply to Kanter M [letter]. Diabetologia 65(10):1753–1754. https://doi.org/10.1007/s00125-022-05766-7
National Center for Health Statistics (2021) NHANES laboratory data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Laboratory. Accessed 26 September 2021
Wang Y, Chen B, Zhang J, Li H, Zeng X, Zhang Z, Zhu Y, Li X, Hu A, Zhao Q, Yang W (2022) Diets with higher insulinaemic potential are associated with increased risk of overall and cardiovascular disease-specific mortality. Br J Nutr 128(10):2011–2020. https://doi.org/10.1017/S0007114521004815
Zhu Y, Peng Z, Lu Y, Li H, Zeng X, Zhang Z, Li X, Hu C, Hu A, Zhao Q, Wang H, Yang W (2022) Higher dietary insulinaemic potential is associated with increased risk of liver steatosis and fibrosis. Liver Int 42(1):69–79. https://doi.org/10.1111/liv.15057
MW F (2006) Lipid metabolism and coronary artery disease. Principles of molecular medicine. Humana Press, Totowa
Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D’Andrea F, Giugliano D (2004) Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 292(12):1440–1446. https://doi.org/10.1001/jama.292.12.1440
Shirani F, Salehi-Abargouei A, Azadbakht L (2013) Effects of dietary approaches to stop hypertension (DASH) diet on some risk for developing type 2 diabetes: a systematic review and meta-analysis on controlled clinical trials. Nutrition 29(7–8):939–947. https://doi.org/10.1016/j.nut.2012.12.021
Soltani S, Chitsazi MJ, Salehi-Abargouei A (2018) The effect of dietary approaches to stop hypertension (DASH) on serum inflammatory markers: a systematic review and meta-analysis of randomized trials. Clin Nutr 37(2):542–550. https://doi.org/10.1016/j.clnu.2017.02.018
Fargnoli JL, Fung TT, Olenczuk DM, Chamberland JP, Hu FB, Mantzoros CS (2008) Adherence to healthy eating patterns is associated with higher circulating total and high-molecular-weight adiponectin and lower resistin concentrations in women from the Nurses’ Health Study. Am J Clin Nutr 88(5):1213–1224. https://doi.org/10.3945/ajcn.2008.26480
Li X, Peng Z, Li M, Zeng X, Li H, Zhu Y, Chen H, Hu A, Zhao Q, Zhang Z, Wang H, Yuan C, Yang W (2022) A healthful plant-based diet is associated with lower odds of nonalcoholic fatty liver disease. Nutrients 14(19):4099. https://doi.org/10.3390/nu14194099
Dahl WJ, Stewart ML (2015) Position of the academy of nutrition and dietetics: health implications of dietary fiber. J Acad Nutr Diet 115(11):1861–1870. https://doi.org/10.1016/j.jand.2015.09.003
Cassidy A, Rogers G, Peterson JJ, Dwyer JT, Lin H, Jacques PF (2015) Higher dietary anthocyanin and flavonol intakes are associated with anti-inflammatory effects in a population of US adults. Am J Clin Nutr 102(1):172–181. https://doi.org/10.3945/ajcn.115.108555
Ma Y, Hebert JR, Li W, Bertone-Johnson ER, Olendzki B, Pagoto SL, Tinker L, Rosal MC, Ockene IS, Ockene JK, Griffith JA, Liu S (2008) Association between dietary fiber and markers of systemic inflammation in the Women’s health initiative observational study. Nutrition 24(10):941–949. https://doi.org/10.1016/j.nut.2008.04.005
Mozaffarian D, Wu JH (2011) Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol 58(20):2047–2067. https://doi.org/10.1016/j.jacc.2011.06.063
Ishikawa T, Suzukawa M, Ito T, Yoshida H, Ayaori M, Nishiwaki M, Yonemura A, Hara Y, Nakamura H (1997) Effect of tea flavonoid supplementation on the susceptibility of low-density lipoprotein to oxidative modification. Am J Clin Nutr 66(2):261–266. https://doi.org/10.1093/ajcn/66.2.261
van Dam RM, Hu FB (2005) Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA 294(1):97–104. https://doi.org/10.1001/jama.294.1.97
Allen NE, Appleby PN, Davey GK, Kaaks R, Rinaldi S, Key TJ (2002) The associations of diet with serum insulin-like growth factor I and its main binding proteins in 292 women meat-eaters, vegetarians, and vegans. Cancer Epidemiol Biomarkers Prev 11(11):1441–1448
Arya F, Egger S, Colquhoun D, Sullivan D, Pal S, Egger G (2010) Differences in postprandial inflammatory responses to a “modern” v. traditional meat meal: a preliminary study. Br J Nutr 104(5):724–728. https://doi.org/10.1017/S0007114510001042
Malik VS, Li Y, Tobias DK, Pan A, Hu FB (2016) Dietary protein intake and risk of type 2 diabetes in US men and women. Am J Epidemiol 183(8):715–728. https://doi.org/10.1093/aje/kwv268
Singh K, Chandra A, Sperry T, Joshi PH, Khera A, Virani SS, Ballantyne CM, Otvos JD, Dullaart RPF, Gruppen EG, Connelly MA, Ayers CR, Rohatgi A (2020) Associations between high-density lipoprotein particles and ischemic events by vascular domain, sex, and ethnicity: a pooled Cohort analysis. Circulation 142(7):657–669. https://doi.org/10.1161/CIRCULATIONAHA.120.045713
Dodson PM, Pacy PJ, Beevers M, Bal P, Fletcher RF, Taylor KG (1983) The effects of a high fibre, low fat and low sodium dietary regime on diabetic hypertensive patients of different ethnic groups. Postgrad Med J 59(696):641–644. https://doi.org/10.1136/pgmj.59.696.641
Dinwiddie GY, Zambrana RE, Doamekpor LA, Lopez L (2015) The impact of educational attainment on observed race/ethnic disparities in inflammatory risk in the 2001–2008 National Health and Nutrition Examination Survey. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph13010042
Pool LR, Ning H, Lloyd-Jones D, Allen NB (2017) Trends in racial/ethnic disparities in cardiovascular health among US adults From 1999–2012. J Am Heart Assoc 6(9):e006027. https://doi.org/10.1161/JAHA.117.006027
Funding
This work was supported by the National Natural Science Foundation of China (82073651), Anhui Provincial Natural Science Foundation (2008085MH262 and 2108085QH357), Anhui Provincial Education Department (gxyqZD2021099), and grants from Anhui Medical University (2021xkjT007, 2020lcxk033, XJ201935, and 2019xkj161).
Author information
Authors and Affiliations
Contributions
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: WY, YH. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: YH, WY. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: YH, XL. Obtained funding: WY, MT. Administrative, technical, or material support: WY. Study supervision: WY.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
The NCHS Research Ethics Review Board approved the NHANES study protocols (#98–12, #2005–06, and #2011–17).
Consent to participate
All participants provided the written informed consent.
Consent for publication
All of the authors have read and approved the final version of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, Y., Li, X., Zhang, T. et al. Associations of healthful and unhealthful plant-based diets with plasma markers of cardiometabolic risk. Eur J Nutr 62, 2567–2579 (2023). https://doi.org/10.1007/s00394-023-03170-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03170-4