Abstract
Purpose
Saturated fat has long been associated with cardiovascular disease in multiple prospective studies, and randomized controlled trials. Few studies have assessed the relative associations between saturated fat and other macronutrients with hypertension, a major risk factor for cardiovascular disease. The aim of this study was to assess the relative associations between saturated fat, other macronutrients such as monounsaturated and polyunsaturated fat, proteins, and carbohydrates, and incident hypertension in a large prospective cohort of French women.
Methods
This study used data from the E3N cohort study, including participants free of hypertension at baseline. A food frequency questionnaire was used to determine dietary intakes of saturated fat (SFA), monounsaturated fat (MUFA), polyunsaturated fat (PUFA), animal protein (AP), vegetable protein (VP), carbohydrates (CH) and various foods. Cases of hypertension were based on self-report, validated by drug reimbursement data. Covariates were based on self-report. Cox proportional hazard models were used to estimate the relative associations between different macronutrients and hypertension risk, using the ‘substitution’ framework. Bootstrapping was used to generate 95% confidence intervals.
Results
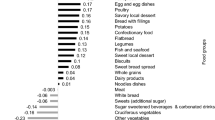
This study included 45,854 women free of hypertension at baseline. During 708,887 person-years of follow-up, 12,338 incident cases of hypertension were identified. Compared to saturated fat, higher consumption of all other macronutrients was associated with a lower risk of hypertension (HRMUFA = 0.74 [0.67: 0.81], HRPUFA = 0.84 [0.77: 0.92], HRCH = 0.83 [0.77: 0.88], HRAP = 0.91 [0.85: 0.97], HRVP = 0.93 [0.83: 1.03]).
Conclusion
This study finds that relative to other macronutrients such as monounsaturated or polyunsaturated fat, higher intake of saturated fat is associated with a higher risk of hypertension among women.
Similar content being viewed by others
Data availability
Data described in the manuscript, code book, and analytic code can be made available upon request by qualified researchers.
References
Keys A (1970) Coronary heart disease in seven countries. Circulation 41:186–195
Jakobsen MU, O’Reilly EJ, Heitmann BL et al (2009) Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr 89:1425–1432. https://doi.org/10.3945/ajcn.2008.27124
Farvid MS, Ding M, Pan A et al (2014) Dietary linoleic acid and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Circulation 130:1568–1578. https://doi.org/10.1161/CIRCULATIONAHA.114.010236
Harcombe Z, Baker JS, Davies B (2017) Evidence from prospective cohort studies does not support current dietary fat guidelines: a systematic review and meta-analysis. Br J Sports Med 51:1743–1749. https://doi.org/10.1136/bjsports-2016-096550
de Souza RJ, Mente A, Maroleanu A et al (2015) Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ 351:h3978. https://doi.org/10.1136/bmj.h3978
Zhu Y, Bo Y, Liu Y (2019) Dietary total fat, fatty acids intake, and risk of cardiovascular disease: a dose–response meta-analysis of cohort studies. Lipids Health Dis 18:91. https://doi.org/10.1186/s12944-019-1035-2
Mozaffarian D, Benjamin EJ, Go AS et al (2016) Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. https://doi.org/10.1161/CIR.0000000000000350
Hooper L, Summerbell CD, Thompson R et al (2011) Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD002137.pub2
Hooper L, Martin N, Jimoh OF et al (2020) Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD011737.pub3
Harcombe Z, Baker JS, DiNicolantonio JJ et al (2016) Evidence from randomised controlled trials does not support current dietary fat guidelines: a systematic review and meta-analysis. Open Heart 3:e000409. https://doi.org/10.1136/openhrt-2016-000409
Schwingshackl L, Hoffmann G (2014) Dietary fatty acids in the secondary prevention of coronary heart disease: a systematic review, meta-analysis and meta-regression. BMJ Open 4:e004487. https://doi.org/10.1136/bmjopen-2013-004487
Hamley S (2017) The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials. Nutr J 16:30. https://doi.org/10.1186/s12937-017-0254-5
Sacks FM, Lichtenstein AH, Wu JHY et al (2017) Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 136:e1–e23. https://doi.org/10.1161/CIR.0000000000000510
Wenger NK, Arnold A, Bairey Merz CN, Cooper-DeHoff RM, Ferdinand KC, Fleg JL, Gulati M, Isiadinso I, Itchhaporia D, Light-McGroary K, Lindley KJ, Mieres JH, Rosser ML, Saade GR, Walsh MN, Pepine CJ (2018) Hypertension across a woman’s life cycle. J Am Coll Cardiol 71(16):1797–1813. https://doi.org/10.1016/j.jacc.2018.02.033 (PMID: 29673470; PMCID: PMC6005390)
Clavel-Chapelon F, van Liere MJ, Giubout C et al (1997) E3N, a French cohort study on cancer risk factors. E3N Group. Etude Epidémiologique auprès de femmes de l’Education Nationale. Eur J Cancer Prev Off J Eur Cancer Prev Organ ECP 6:473–478
van Liere MJ, Lucas F, Clavel F et al (1997) Relative validity and reproducibility of a French dietary history questionnaire. Int J Epidemiol 26(Suppl 1):S128–S136. https://doi.org/10.1093/ije/26.suppl_1.s128
Slimani N, Kaaks R, Ferrari P et al (2002) European Prospective Investigation into Cancer and Nutrition (EPIC) calibration study: rationale, design and population characteristics. Public Health Nutr 5:1125–1145. https://doi.org/10.1079/PHN2002395
Répertoire général des aliments : table de composition=Composition tables-fdi:010009113-Horizon. https://www.documentation.ird.fr/hor/fdi:010009113. Accessed 11 Mar 2022
Thiébaut ACM, Rotival M, Gauthier E et al (2009) Correlation between serum phospholipid fatty acids and dietary intakes assessed a few years earlier. Nutr Cancer 61:500–509. https://doi.org/10.1080/01635580802710717
Hercberg S (coordinator) (2005) Table de composition SU.VI.MAX des aliments. Les 330; éditions INSERM/Economica, Paris, 182 p
Astorg P, Arnault N, Czernichow S, Noisette N, Galan P, Hercberg S (2004) Dietary intakes and food sources of n−6 and n−3 PUFA in french adult men and women. Lipids 39:527–535. https://doi.org/10.1007/s11745-004-1259-6
Lajous M, Bijon A, Fagherazzi G et al (2014) Processed and unprocessed red meat consumption and hypertension in women. Am J Clin Nutr 100:948–952. https://doi.org/10.3945/ajcn.113.080598
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett Jr DR, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS (2011) Compendium of physical activities: a second update of codes and met values. Med Sci Sport Exerc 43(8):1575–1581
Tehard B, van Liere MJ, Com Nougué C, Clavel-Chapelon F (2002) Anthropometric measurements and body silhouette of women: validity and perception. J Am Diet Assoc 102(12):1779–1784. https://doi.org/10.1016/s0002-8223(02)90381-0 (PMID: 12487540; PMCID: PMC2020514)
Ibsen DB, Laursen ASD, Würtz AML et al (2021) Food substitution models for nutritional epidemiology. Am J Clin Nutr 113:294–303. https://doi.org/10.1093/ajcn/nqaa315
Tomova GD, Arnold KF, Gilthorpe MS, Tennant PWG (2022) Adjustment for energy intake in nutritional research: a causal inference perspective. Am J Clin Nutr 115:189–198. https://doi.org/10.1093/ajcn/nqab266
Wang L, Manson JE, Forman JP et al (2010) Dietary fatty acids and the risk of hypertension in middle-aged and older women. Hypertension 56:598–604. https://doi.org/10.1161/HYPERTENSIONAHA.110.154187
Witteman JC, Willett WC, Stampfer MJ et al (1989) A prospective study of nutritional factors and hypertension among US women. Circulation 80:1320–1327. https://doi.org/10.1161/01.CIR.80.5.1320
Matsumoto C, Yoruk A, Wang L et al (2019) Fish and omega-3 fatty acid consumption and risk of hypertension. J Hypertens 37:1223–1229. https://doi.org/10.1097/HJH.0000000000002062
Appel LJ, Moore TJ, Obarzanek E et al (1997) A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 336:1117–1124. https://doi.org/10.1056/NEJM199704173361601
Chiu S, Bergeron N, Williams PT et al (2016) Comparison of the DASH (Dietary Approaches to Stop Hypertension) diet and a higher-fat DASH diet on blood pressure and lipids and lipoproteins: a randomized controlled trial123. Am J Clin Nutr 103:341–347. https://doi.org/10.3945/ajcn.115.123281
Toledo E, Hu FB, Estruch R et al (2013) Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial. BMC Med 11:207. https://doi.org/10.1186/1741-7015-11-207
Fritsche KL (2015) The science of fatty acids and inflammation. Adv Nutr Bethesda Md 6:293S-301S. https://doi.org/10.3945/an.114.006940
Schwartz EA, Zhang W-Y, Karnik SK et al (2010) Nutrient modification of the innate immune response. Arterioscler Thromb Vasc Biol 30:802–808. https://doi.org/10.1161/ATVBAHA.109.201681
de Heredia FP, Gómez-Martínez S, Marcos A (2012) Obesity, inflammation and the immune system. Proc Nutr Soc 71:332–338. https://doi.org/10.1017/S0029665112000092
Cani PD, Amar J, Iglesias MA et al (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772. https://doi.org/10.2337/db06-1491
Mani V, Hollis JH, Gabler NK (2013) Dietary oil composition differentially modulates intestinal endotoxin transport and postprandial endotoxemia. Nutr Metab 10:6. https://doi.org/10.1186/1743-7075-10-6
Voon PT, Ng TKW, Lee VKM, Nesaretnam K (2011) Diets high in palmitic acid (16:0), lauric and myristic acids (12:0 + 14:0), or oleic acid (18:1) do not alter postprandial or fasting plasma homocysteine and inflammatory markers in healthy Malaysian adults. Am J Clin Nutr 94:1451–1457. https://doi.org/10.3945/ajcn.111.020107
Sesso HD, Wang L, Buring JE et al (1979) (2007) Comparison of interleukin-6 and C-reactive protein for the risk of developing hypertension in women. Hypertens Dallas TX 49:304–310. https://doi.org/10.1161/01.HYP.0000252664.24294.ff
Mattace-Raso FUS, Verwoert GC, Hofman A, Witteman JCM (2010) Inflammation and incident-isolated systolic hypertension in older adults: the Rotterdam study. J Hypertens 28:892–895. https://doi.org/10.1097/HJH.0b013e328336ed26
Chiu Y-H (2022) Well-defined interventions for nutritional studies: from target trials to nutritional modeling. Am J Clin Nutr 115:3–5. https://doi.org/10.1093/ajcn/nqab343
Renaud S, de Lorgeril M (1992) Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 339(8808):1523–1526. https://doi.org/10.1016/0140-6736(92)91277-f (PMID: 1351198)
Steur M, Johnson L, Sharp SJ et al (2021) Dietary fatty acids, macronutrient substitutions, food sources and incidence of coronary heart disease: findings from the EPIC-CVD case-cohort study across nine European countries. J Am Heart Assoc 10:e019814. https://doi.org/10.1161/JAHA.120.019814
Acknowledgements
We gratefully acknowledge the contribution of all the participants in the E3N study for their diligence and their answers.
Funding
The E3N cohort is being carried out with the financial support of the “Mutuelle Générale de l’Education Nationale” (MGEN); European Community; French League against Cancer (LNCC); Gustave Roussy Institute (IGR); French Institute of Health and Medical Research (INSERM). This present study was also supported by the French Research Agency (Agence Nationale de la Recherche) via an “Investissement d’Avenir” grant (investment for the future grant, ANR-10-COHO-0006). CJM is supported by funding from the Federation Française de Cardiologie. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
ALM—designed research, conducted research, wrote paper. CMV—designed research, conducted research. GS—designed research, conducted research. MCBR—designed research, conducted research, wrote paper. CJM—designed research, conducted research, analyzed data, wrote paper, had primary responsibility for final content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethics approval
The E3N study was authorized by the French National Commission for Data Protection and Privacy (CNIL no 106.246). E3N data enrichment with the MGEN database was granted ethical approval (CCTIRS no 13.794) and was authorized by the CNIL (no. 327346V14).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
MacDonald, C.J., Madkia, AL., Mounier-Vehier, C. et al. Associations between saturated fat intake and other dietary macronutrients and incident hypertension in a prospective study of French women. Eur J Nutr 62, 1207–1215 (2023). https://doi.org/10.1007/s00394-022-03053-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-03053-0