Abstract
Aims
Overconsumption of sugar-sweetened beverages (SSBs) is associated with an increased risk of metabolic disorders, including obesity and diabetes. However, accumulating evidence also suggests the potential negative impact of consuming nonnutritive sweeteners (NNSs) on weight and glycaemic control. The metabolic effects of sucralose, the most widely used NNS, remain controversial. This study aimed to compare the impact of intake of dietary sucralose (acceptable daily intake dose, ADI dose) and sucrose-sweetened water (at the same sweetness level) on lipid and glucose metabolism in male mice.
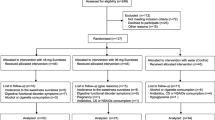
Materials and methods
Sucralose (0.1 mg/mL) or sucrose (60 mg/mL) was added to the drinking water of 8-week-old male C57BL/6 mice for 16 weeks, followed by oral glucose and intraperitoneal insulin tolerance tests, and measurements of bone mineral density, plasma lipids, and hormones. After the mice were sacrificed, the duodenum and ileum were used for examination of sweet taste receptors (STRs) and glucose transporters.
Results
A significant increase in fat mass was observed in the sucrose group of mice after 16 weeks of sweetened water drinking. Sucrose consumption also led to increased levels of plasma LDL, insulin, lipid deposition in the liver, and increased glucose intolerance in mice. Compared with the sucrose group, mice consuming sucralose showed much lower fat accumulation, hyperlipidaemia, liver steatosis, and glucose intolerance. In addition, the daily dose of sucralose only had a moderate effect on T1R2/3 in the intestine, without affecting glucose transporters and plasma insulin levels.
Conclusion
Compared with mice consuming sucrose-sweetened water, daily drinking of sucralose within the ADI dose had a much lower impact on glucose and lipid homeostasis.





Similar content being viewed by others
Abbreviations
- SSB:
-
Sugar-sweetened beverage
- NNS:
-
Nonnutritive sweetener
- ADI:
-
Acceptable daily intake
- STRs:
-
Sweet taste receptors
- FDA:
-
U.S. Food and Drug Administration
- ADME:
-
Absorption, distribution, metabolism, and excretion
- NOAEL:
-
No observed adverse effect level
- BMD:
-
Bone mineral density
- RER:
-
Respiratory exchange ratio
- PFA:
-
Paraformaldehyde
- GTT:
-
Glucose tolerance test
- ITT:
-
Insulin tolerance test
- TC:
-
Total plasma cholesterol
- TG:
-
Triglycerides
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- FPKM:
-
Fragments per kilobase of transcript per million mapped reads
- Hb1AC:
-
Blood haemoglobin A1c
- GLUT2:
-
Glucose transporter 2
- SGLT1:
-
Sodium/glucose cotransporter 1
- T1R2/3:
-
Taste receptor type 1 member 2/3
- GIP:
-
Glucose-dependent insulinotropic peptide
- GLP-1:
-
Glucagon-like peptide-1
- AHA:
-
American Heart Association
References
Burchfield JG, Kebede MA, Meoli CC, Stockli J, Whitworth PT, Wright AL, Hoffman NJ, Minard AY, Ma X, Krycer JR, Nelson ME, Tan SX, Yau B, Thomas KC, Wee NKY, Khor EC, Enriquez RF, Vissel B, Biden TJ, Baldock PA, Hoehn KL, Cantley J, Cooney GJ, James DE, Fazakerley DJ (2018) High dietary fat and sucrose results in an extensive and time-dependent deterioration in health of multiple physiological systems in mice. J Biol Chem 293(15):5731–5745. https://doi.org/10.1074/jbc.RA117.000808
Herman MA, Birnbaum MJ (2021) Molecular aspects of fructose metabolism and metabolic disease. Cell Metab 33(12):2329–2354. https://doi.org/10.1016/j.cmet.2021.09.010
Li XE, Lopetcharat K, Drake MA (2015) Parents’ and children’s acceptance of skim chocolate milks sweetened by monk fruit and stevia leaf extracts. J Food Sci 80(5):S1083-1092. https://doi.org/10.1111/1750-3841.12835
Gardner C, Wylie-Rosett J, Gidding SS, Steffen LM, Johnson RK, Reader D, Lichtenstein AH, American Heart association nutrition committee of the council on nutrition PA, metabolism CoAT, vascular biology CoCDitY, the American D (2012) Nonnutritive sweeteners: current use and health perspectives: a scientific statement from the American heart association and the American diabetes association. Circulation 126(4):509–519. https://doi.org/10.1161/CIR.0b013e31825c42ee
Hunter SR, Reister EJ, Cheon E, Mattes RD (2019) Low calorie sweeteners differ in their physiological effects in humans. Nutrients. https://doi.org/10.3390/nu11112717
Peters JC, Wyatt HR, Foster GD, Pan Z, Wojtanowski AC, Vander Veur SS, Herring SJ, Brill C, Hill JO (2014) The effects of water and non-nutritive sweetened beverages on weight loss during a 12-week weight loss treatment program. Obesity (Silver Spring) 22(6):1415–1421. https://doi.org/10.1002/oby.20737
Ahmad SY, Friel JK, MacKay DS (2020) The effect of the artificial sweeteners on glucose metabolism in healthy adults: a randomized, double-blinded, crossover clinical trial. Appl Physiol Nutr Metab 45(6):606–612. https://doi.org/10.1139/apnm-2019-0359
Azad MB, Abou-Setta AM, Chauhan BF, Rabbani R, Lys J, Copstein L, Mann A, Jeyaraman MM, Reid AE, Fiander M, MacKay DS, McGavock J, Wicklow B, Zarychanski R (2017) Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ 189(28):E929–E939. https://doi.org/10.1503/cmaj.161390
Lutsey PL, Steffen LM, Stevens J (2008) Dietary intake and the development of the metabolic syndrome: the atherosclerosis risk in communities study. Circulation 117(6):754–761. https://doi.org/10.1161/CIRCULATIONAHA.107.716159
Nettleton JA, Lutsey PL, Wang Y, Lima JA, Michos ED, Jacobs DR Jr (2009) Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the multi-ethnic study of atherosclerosis (MESA). Diabetes Care 32(4):688–694. https://doi.org/10.2337/dc08-1799
Fagherazzi G, Vilier A, Saes Sartorelli D, Lajous M, Balkau B, Clavel-Chapelon F (2013) Consumption of artificially and sugar-sweetened beverages and incident type 2 diabetes in the etude epidemiologique aupres des femmes de la mutuelle generale de l’Education nationale-European prospective investigation into cancer and nutrition cohort. Am J Clin Nutr 97(3):517–523. https://doi.org/10.3945/ajcn.112.050997
Basson AR, Rodriguez-Palacios A, Cominelli F (2021) Artificial sweeteners: history and new concepts on inflammation. Front Nutr 8:746247. https://doi.org/10.3389/fnut.2021.746247
Ahmad SY, Friel JK, Mackay DS (2020) Effect of sucralose and aspartame on glucose metabolism and gut hormones. Nutr Rev 78(9):725–746. https://doi.org/10.1093/nutrit/nuz099
Meng Y, Li S, Khan J, Dai Z, Li C, Hu X, Shen Q, Xue Y (2021) Sugar- and artificially sweetened beverages consumption linked to type 2 diabetes, cardiovascular diseases, and all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Nutrients. https://doi.org/10.3390/nu13082636
Rulis AM, Levitt JA (2009) FDA’S food ingredient approval process: safety assurance based on scientific assessment. Regul Toxicol Pharmacol 53(1):20–31. https://doi.org/10.1016/j.yrtph.2008.10.003
Magnuson BA, Roberts A, Nestmann ER (2017) Critical review of the current literature on the safety of sucralose. Food Chem Toxicol 106:324–355. https://doi.org/10.1016/j.fct.2017.05.047
Plaza-Diaz J, Pastor-Villaescusa B, Rueda-Robles A, Abadia-Molina F, Ruiz-Ojeda FJ (2020) Plausible biological interactions of low- and non-calorie sweeteners with the intestinal microbiota: an update of recent studies. Nutrients. https://doi.org/10.3390/nu12041153
Jang HJ, Kokrashvili Z, Theodorakis MJ, Carlson OD, Kim BJ, Zhou J, Kim HH, Xu X, Chan SL, Juhaszova M, Bernier M, Mosinger B, Margolskee RF, Egan JM (2007) Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc Natl Acad Sci U S A 104(38):15069–15074. https://doi.org/10.1073/pnas.0706890104
Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, Israeli D, Zmora N, Gilad S, Weinberger A, Kuperman Y, Harmelin A, Kolodkin-Gal I, Shapiro H, Halpern Z, Segal E, Elinav E (2014) Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514(7521):181–186. https://doi.org/10.1038/nature13793
Uebanso T, Ohnishi A, Kitayama R, Yoshimoto A, Nakahashi M, Shimohata T, Mawatari K, Takahashi A (2017) Effects of low-dose non-caloric sweetener consumption on gut microbiota in mice. Nutrients. https://doi.org/10.3390/nu9060560
Pepino MY, Tiemann CD, Patterson BW, Wice BM, Klein S (2013) Sucralose affects glycemic and hormonal responses to an oral glucose load. Diabetes Care 36(9):2530–2535. https://doi.org/10.2337/dc12-2221
Shi Q, Zhu X, Zhou J, Chen L (2018) Low intake of digestible carbohydrates ameliorates the duodenal absorption of carbohydrates in mice with glucose metabolic disorders induced by sucralose. Food Funct 9(12):6236–6244. https://doi.org/10.1039/c8fo02029a
Kim JY, Prescott J, Kim KO (2017) Emotional responses to sweet foods according to sweet liker status. Food Qual Prefer 59:1–7. https://doi.org/10.1016/j.foodqual.2017.01.013
Glendinning JI, Hart S, Lee H, Maleh J, Ortiz G, Ryu YS, Sanchez A, Shelling S, Williams N (2020) Low-calorie sweeteners cause only limited metabolic effects in mice. Am J Physiol Regul Integr Comp Physiol 318(1):R70–R80. https://doi.org/10.1152/ajpregu.00245.2019
Shi Q, Zhu X, Deng S (2021) Sweet taste receptor expression and its activation by sucralose to regulate glucose absorption in mouse duodenum. J Food Sci 86(2):540–545. https://doi.org/10.1111/1750-3841.14586
Margolskee RF, Dyer J, Kokrashvili Z, Salmon KS, Ilegems E, Daly K, Maillet EL, Ninomiya Y, Mosinger B, Shirazi-Beechey SP (2007) T1R3 and gustducin in gut sense sugars to regulate expression of Na+-glucose cotransporter 1. Proc Natl Acad Sci U S A 104(38):15075–15080. https://doi.org/10.1073/pnas.0706678104
Kojima I, Nakagawa Y (2011) The role of the sweet taste receptor in enteroendocrine cells and pancreatic beta-cells. Diabetes Metab J 35(5):451–457. https://doi.org/10.4093/dmj.2011.35.5.451
Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J, American heart association nutrition committee of the council on nutrition PA, metabolism, the council on E, Prevention (2009) Dietary sugars intake and cardiovascular health: a scientific statement from the american heart association. Circulation 120(11):1011–1020. https://doi.org/10.1161/CIRCULATIONAHA.109.192627
Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, Kshirsagar AV (2010) Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int 77(7):609–616. https://doi.org/10.1038/ki.2009.500
Jurgens H, Haass W, Castaneda TR, Schurmann A, Koebnick C, Dombrowski F, Otto B, Nawrocki AR, Scherer PE, Spranger J, Ristow M, Joost HG, Havel PJ, Tschop MH (2005) Consuming fructose-sweetened beverages increases body adiposity in mice. Obes Res 13(7):1146–1156. https://doi.org/10.1038/oby.2005.136
Lindqvist A, de la Cour CD, Stegmark A, Håkanson R, Erlanson-Albertsson C (2005) Overeating of palatable food is associated with blunted leptin and ghrelin responses. Regul Pept 130(3):123–132. https://doi.org/10.1016/j.regpep.2005.05.002
Saltiel MY, Kuhre RE, Christiansen CB, Eliasen R, Conde-Frieboes KW, Rosenkilde MM, Holst JJ (2017) Sweet taste receptor activation in the Gut is of limited importance for glucose stimulated GLP1 and GIP secretion. Nutrients. https://doi.org/10.3390/nu9040418
Li X, Staszewski L, Xu H, Durick K, Zoller M, Adler E (2002) Human receptors for sweet and umami taste. Proc Natl Acad Sci U S A 99(7):4692–4696. https://doi.org/10.1073/pnas.072090199
Toft-Nielsen M-B, Damholt MB, Madsbad S, Hilsted LM, Hughes TE, Michelsen BK, Holst JJ (2001) Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 86(8):3717–3723. https://doi.org/10.1210/jcem.86.8.7750
Vollmer K, Holst JJ, Baller B, Ellrichmann M, Nauck MA, Schmidt WE, Meier JJ (2008) Predictors of incretin concentrations in subjects with normal, impaired, and diabetic glucose tolerance. Diabetes 57(3):678–687. https://doi.org/10.2337/db07-1124
Acknowledgements
None.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 31972912, 82030026, and 31771666) the Jiangsu Provincial Department of Science and Technology (No. BK20211153), and the Fundamental Research Funds for the Central Universities (No. 020814380173).
Author information
Authors and Affiliations
Contributions
Conceptualization: XJ, XW, LC and HW; investigation: XW, LC, HW, JX, ZZ, XJ, JW, HZ, YS, YT, QY and QL; writing of the manuscript: XJ, YZ, JL; funding acquisition: XJ, YZ, JL; supervision: XJ, YZ, JL.
Corresponding authors
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, X., Cui, L., Wang, H. et al. Impact of dietary sucralose and sucrose-sweetened water intake on lipid and glucose metabolism in male mice. Eur J Nutr 62, 199–211 (2023). https://doi.org/10.1007/s00394-022-02980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02980-2