Abstract
Purpose
Maternal nutrition during early development and paternal nutrition pre-conception can programme offspring health status. Hypothalamus adipose axis is a target of developmental programming, and paternal and maternal high-fat, high-sugar diet (HFS) may be an important factor that predisposes offspring to develop obesity later in life. This study aims to investigate Wistar rats’ maternal and paternal HFS differential contribution on the development, adiposity, and hypothalamic inflammation in male offspring from weaning until adulthood.
Methods
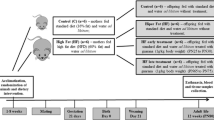
Male progenitors were fed a control diet (CD) or HFS for 10 weeks before mating. After mating, dams were fed CD or HFS only during pregnancy and lactation. Forming the following male offspring groups: CD—maternal and paternal CD; MH—maternal HFS and paternal CD; PH—maternal CD and paternal HFS; PMH—maternal and paternal HFS. After weaning, male offspring were fed CD until adulthood.
Results
Maternal HFS diet increased weight, visceral adiposity, and serum total cholesterol levels, and decreased hypothalamic weight in weanling male rats. In adult male offspring, maternal HFS increased weight, glucose levels, and hypothalamic NFκBp65. Paternal HFS diet lowered hypothalamic insulin receptor levels in weanling offspring and glucose and insulin levels in adult offspring. The combined effects of maternal and paternal HFS diets increased triacylglycerol, leptin levels, and hypothalamic inflammation in weanling rats, and increased visceral adiposity in adulthood.
Conclusion
Male offspring intake of CD diet after weaning reversed part of the effects of parental HFS diet during the perinatal period. However, maternal and paternal HFS diet affected adiposity and hypothalamic inflammation, which remained until adulthood.




Similar content being viewed by others
Change history
08 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00394-021-02725-7
References
Barker DJ (1991) The intrauterine environment and adult cardiovascular disease. Ciba Found Symp 156:3–6
Ravelli ACJ, Van Der Meulen JHP, Osmond C et al (1999) Obesity at the age of 50 year in men and women exposed to famine prenatally. Am J Clin Nutr 70:811–816. https://doi.org/10.1093/ajcn/70.5.811
Barker DJ, Gluckman PD, Godfrey KM et al (1993) Fetal nutrition and cardiovascular disease in adult life. Lancet (London, England) 341:938–941
Mennitti LV, Oyama LM, Santamarina AB et al (2018) Early exposure to distinct sources of lipids affects differently the development and hepatic inflammatory profiles of 21-day-old rat offspring. J Inflamm Res 11:11–24. https://doi.org/10.2147/JIR.S152326
Mennitti LV, Oyama LM, de Oliveira JL et al (2014) Oligofructose supplementation during pregnancy and lactation impairs offspring development and alters the intestinal properties of 21-d-old pups. Lipids Health Dis 13:26. https://doi.org/10.1186/1476-511X-13-26
Mennitti LV, Oyama LM, Santamarina AB et al (2018) Influence of maternal consumption of different types of fatty acids during pregnancy and lactation on lipid and glucose metabolism of the 21-day-old male offspring in rats. Prostaglandins Leukot Essent Fatty Acids 135:54–62. https://doi.org/10.1016/j.plefa.2018.07.001
Mennitti LV, Oliveira JL, Morais CA et al (2015) Type of fatty acids in maternal diets during pregnancy and/or lactation and metabolic consequences of the offspring. J Nutr Biochem 26:99–111. https://doi.org/10.1016/j.jnutbio.2014.10.001
Mendes-da-Silva C, Giriko CÁ, Mennitti LV et al (2014) Maternal high-fat diet during pregnancy or lactation changes the somatic and neurological development of the offspring. Arq Neuropsiquiatr 72:136–144. https://doi.org/10.1590/0004-282X20130220
Gawlińska K, Gawliński D, Filip M, Przegaliński E (2020) Relationship of maternal high-fat diet during pregnancy and lactation to offspring health. Nutr Rev. https://doi.org/10.1093/nutrit/nuaa020
Sferruzzi-Perri AN, Vaughan OR, Haro M et al (2013) An obesogenic diet during mouse pregnancy modifies maternal nutrient partitioning and the fetal growth trajectory. FASEB J 27:3928–3937. https://doi.org/10.1096/fj.13-234823
Musial B, Vaughan OR, Fernandez-Twinn DS et al (2017) A Western-style obesogenic diet alters maternal metabolic physiology with consequences for fetal nutrient acquisition in mice. J Physiol 595:4875–4892. https://doi.org/10.1113/JP273684
Warner MJ, Ozanne SE (2010) Mechanisms involved in the developmental programming of adulthood disease. Biochem J 427:333–347. https://doi.org/10.1042/BJ20091861
Nicholas LM, Morrison JL, Rattanatray L et al (2016) The early origins of obesity and insulin resistance: timing, programming and mechanisms. Int J Obes 40:229–238. https://doi.org/10.1038/ijo.2015.178
Xavier S, Gili J, McGowan P et al (2021) High maternal omega-3 supplementation dysregulates body weight and leptin in newborn male and female rats: implications for hypothalamic developmental programming. Nutrients. https://doi.org/10.3390/nu13010089
McPherson NO, Bell VG, Zander-Fox DL et al (2015) When two obese parents are worse than one! Impacts on embryo and fetal development. Am J Physiol Metab 309:E568–E581. https://doi.org/10.1152/ajpendo.00230.2015
Klastrup LK, Bak ST, Nielsen AL (2019) The influence of paternal diet on sncRNA-mediated epigenetic inheritance. Mol Genet Genomics 294:1–11. https://doi.org/10.1007/s00438-018-1492-8
Keleher MR, Zaidi R, Shah S et al (2018) Maternal high-fat diet associated with altered gene expression, DNA methylation, and obesity risk in mouse offspring. PLoS ONE. https://doi.org/10.1371/journal.pone.0192606
Schagdarsurengin U, Steger K (2016) Epigenetics in male reproduction: effect of paternal diet on sperm quality and offspring health. Nat Rev Urol 13:584–595
Wattez JS, Delahaye F, Lukaszewski MA et al (2013) Perinatal nutrition programs the hypothalamic melanocortin system in offspring. Horm Metab Res 45:980–990
Breton C (2013) The hypothalamus-adipose axis is a key target of developmental programming by maternal nutritional manipulation. J Endocrinol 216:R19-31. https://doi.org/10.1530/JOE-12-0157
Cesar HC, Pisani LP (2017) Fatty-acid-mediated hypothalamic inflammation and epigenetic programming. J Nutr Biochem 42:1–6. https://doi.org/10.1016/j.jnutbio.2016.08.008
Thaler JP, Yi C-X, Schur EA et al (2012) Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest 122:153–162. https://doi.org/10.1172/JCI59660
Valdearcos M, Robblee MM, Benjamin DI et al (2014) Microglia Dictate the impact of saturated fat consumption on hypothalamic inflammation and neuronal function. Cell Rep 9:2124–2138. https://doi.org/10.1016/j.celrep.2014.11.018
Lemes SF, de Souza ACP, Payolla TB et al (2018) Maternal consumption of high-fat diet in mice alters hypothalamic notch pathway, NPY cell population and food intake in offspring. Neuroscience 371:1–15. https://doi.org/10.1016/j.neuroscience.2017.11.043
Chang G-Q, Gaysinskaya V, Karatayev O, Leibowitz SF (2008) Maternal high-fat diet and fetal programming: increased proliferation of hypothalamic peptide-producing neurons that increase risk for overeating and obesity. J Neurosci 28:12107–12119. https://doi.org/10.1523/JNEUROSCI.2642-08.2008
Rajia S, Chen H, Morris MJ (2010) Maternal overnutrition impacts offspring adiposity and brain appetite markers-modulation by postweaning diet. J Neuroendocrinol 22:905–914. https://doi.org/10.1111/j.1365-2826.2010.02005.x
Ornellas F, Souza-Mello V, Mandarim-de-Lacerda CA, Aguila MB (2016) Combined parental obesity augments single-parent obesity effects on hypothalamus inflammation, leptin signaling (JAK/STAT), hyperphagia, and obesity in the adult mice offspring. Physiol Behav 153:47–55. https://doi.org/10.1016/j.physbeh.2015.10.019
Chen Y-P, Xiao X-M, Li J et al (2012) Paternal body mass index (BMI) is associated with offspring intrauterine growth in a gender dependent manner. PLoS ONE 7:e36329. https://doi.org/10.1371/journal.pone.0036329
Freeman E, Fletcher R, Collins CE et al (2012) Preventing and treating childhood obesity: time to target fathers. Int J Obes (Lond) 36:12–15. https://doi.org/10.1038/ijo.2011.198
Sanchez-Garrido MA, Ruiz-Pino F, Velasco I et al (2018) Intergenerational influence of paternal obesity on metabolic and reproductive health parameters of the offspring: male-preferential impact and involvement of kiss1-mediated pathways. Endocrinology 159:1005–1018. https://doi.org/10.1210/en.2017-00705
Ng S-F, Lin RCY, Laybutt DR et al (2010) Chronic high-fat diet in fathers programs β-cell dysfunction in female rat offspring. Nature 467:963
Masuyama H, Mitsui T, Eguchi T et al (2016) The effects of paternal high-fat diet exposure on offspring metabolism with epigenetic changes in the mouse adiponectin and leptin gene promoters. Am J Physiol Endocrinol Metab 311:E236–E245. https://doi.org/10.1152/ajpendo.00095.2016
Chowdhury S, Lecomte V, Erlich J et al (2016) Paternal high fat diet in rats leads to renal accumulation of lipid and tubular changes in adult offspring. Nutrients 8:521. https://doi.org/10.3390/nu8090521
Zhang X, Dong Y, Sun G et al (2019) Paternal programming of liver function and lipid profile induced by a paternal pre-conceptional unhealthy diet: potential association with altered gut microbiome composition. Kidney Blood Press Res 44:133–148. https://doi.org/10.1159/000497487
Zheng J, Xiao X, Zhang Q, Yu M (2014) DNA methylation: the pivotal interaction between early-life nutrition and glucose metabolism in later life. Br J Nutr 112:1850–1857. https://doi.org/10.1017/S0007114514002827
Samuelsson A-M, Matthews PA, Argenton M et al (2007) Diet-induced obesity in female mice leads to offspring hyperphagia, adiposity, hypertension, and insulin resistance. Hypertension 51:383–392. https://doi.org/10.1161/hypertensionaha.107.101477
Subcommittee on Laboratory Animal Nutrition; Committee on Animal Nutrition; Board on Agriculture; National Research Council (1995) Nutrient requirements of laboratory animals, 4th edn. The National Academies Press, Washington
Mitchell JA, Hutchins M, Schindler WJ, Critchlow V (1973) Increases in plasma growth hormone concentration and naso-anal length in rats following isolation of the medial basal hypothalamus. Neuroendocrinology 12:161–173. https://doi.org/10.1159/000122230
Nunez AA, Kannan K, Giesy JP et al (2001) Effects of bisphenol A on energy balance and accumulation in brown adipose tissue in rats. Chemosphere 42:917–922. https://doi.org/10.1016/S0045-6535(00)00196-X
Wells JCK (2018) Understanding developmental plasticity as adaptation requires an inter-generational perspective. Evol Med public Heal 2017:185–187. https://doi.org/10.1093/emph/eox023
O’Reilly JR, Reynolds RM (2013) The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf) 78:9–16
Falcão-Tebas F, Marin EC, Kuang J et al (2020) Maternal exercise attenuates the lower skeletal muscle glucose uptake and insulin secretion caused by paternal obesity in female adult rat offspring. J Physiol. https://doi.org/10.1113/jp279582
Arentson-Lantz EJ, Buhman KK, Ajuwon K, Donkin SS (2014) Excess pregnancy weight gain leads to early indications of metabolic syndrome in a swine model of fetal programming. Nutr Res 34:241–249. https://doi.org/10.1016/j.nutres.2014.01.001
Cavalcanti-de-Albuquerque JP, Bober J, Zimmer MR, Dietrich MO (2019) Regulation of substrate utilization and adiposity by Agrp neurons. Nat Commun. https://doi.org/10.1038/s41467-018-08239-x
Carew LB Jr, Hill FW (1964) Effect of corn oil on metabolic efficiency of energy utilization by chicks. J Nutr 83:293–299. https://doi.org/10.1093/jn/83.4.293
Crescenzo R, Bianco F, Falcone I et al (2012) Hepatic mitochondrial energetics during catch-up fat with high-fat diets rich in lard or safflower oil. Obesity 20:1763–1772. https://doi.org/10.1038/oby.2011.167
Iossa S, Lionetti L, Mollica MP et al (2003) Effect of high-fat feeding on metabolic efficiency and mitochondrial oxidative capacity in adult rats. Br J Nutr 90:953–960. https://doi.org/10.1079/BJN2003000968
Calonne J, Isacco L, Miles-Chan J et al (2019) Reduced skeletal muscle protein turnover and thyroid hormone metabolism in adaptive thermogenesis that facilitates body fat recovery during weight regain. Front Endocrinol (Lausanne) 10:119. https://doi.org/10.3389/fendo.2019.00119
Zhang X, Chen W, Shao S et al (2018) A high-fat diet rich in saturated and mono-unsaturated fatty acids induces disturbance of thyroid lipid profile and hypothyroxinemia in male rats. Mol Nutr Food Res 62:1700599. https://doi.org/10.1002/mnfr.201700599
Broeders EPM, Vijgen GHEJ, Havekes B et al (2016) Thyroid hormone activates brown adipose tissue and increases non-shivering thermogenesis—a cohort study in a group of thyroid carcinoma patients. PLoS ONE 11:e0145049–e0145049. https://doi.org/10.1371/journal.pone.0145049
Bourguignon A, Rameau A, Toullec G et al (2017) Increased mitochondrial energy efficiency in skeletal muscle after long-term fasting: its relevance to animal performance. J Exp Biol 220:2445–2451. https://doi.org/10.1242/jeb.159087
Fromme T, Klingenspor M (2011) Uncoupling protein 1 expression and high-fat diets. Am J Physiol Regul Integr Comp Physiol 300:R1-8. https://doi.org/10.1152/ajpregu.00411.2010
Bond LM, Ntambi JM (2018) UCP1 deficiency increases adipose tissue monounsaturated fatty acid synthesis and trafficking to the liver. J Lipid Res 59:224–236. https://doi.org/10.1194/jlr.M078469
Ribaroff GA, Wastnedge E, Drake AJ et al (2017) Animal models of maternal high fat diet exposure and effects on metabolism in offspring: a meta-regression analysis. Obes Rev 18:673–686. https://doi.org/10.1111/obr.12524
Müller MJ, Bosy-Westphal A, Heymsfield SB (2010) Is there evidence for a set point that regulates human body weight? F100 Med Rep. https://doi.org/10.3410/M2-59
Sullivan EL, Smith MS, Grove KL (2011) Perinatal exposure to high-fat diet programs energy balance, metabolism and behavior in adulthood. Neuroendocrinology 93:1–8. https://doi.org/10.1159/000322038
Reinhardt M, Thearle MS, Ibrahim M et al (2015) A human thrifty phenotype associated with less weight loss during caloric restriction. Diabetes 64:2859–2867. https://doi.org/10.2337/db14-1881
Ghaben AL, Scherer PE (2019) Adipogenesis and metabolic health. Nat Rev Mol Cell Biol 20:242–258. https://doi.org/10.1038/s41580-018-0093-z
Reynolds AN, Akerman AP, Mann J (2020) Dietary fibre and whole grains in diabetes management: systematic review and meta-analyses. PLOS Med 17:e1003053. https://doi.org/10.1371/journal.pmed.1003053
Moraes JC, Coope A, Morari J et al (2009) High-fat diet induces apoptosis of hypothalamic neurons. PLoS ONE. https://doi.org/10.1371/journal.pone.0005045
Kim YJ (2006) What is fetal programming?: A lifetime health is under the control of in-utero health. Korean J Obs Gynecol 49:2055–2065
Lee CH, Suk K, Yu R, Kim M-S (2020) Cellular Contributors to hypothalamic inflammation in obesity. Mol Cells 43:431–437. https://doi.org/10.14348/molcells.2020.0055
Valdearcos M, Douglass JD, Robblee MM et al (2017) Microglial inflammatory signaling orchestrates the hypothalamic immune response to dietary excess and mediates obesity susceptibility. Cell Metab 26:185-197.e3. https://doi.org/10.1016/j.cmet.2017.05.015
Reynoso M, Geddis A, Mitrophanov A et al (2017) NFkB activation and cytokine output in LPS-treated RAW 264.7 macrophages. FASEB J. https://doi.org/10.1096/fasebj.31.1_supplement.lb146
Zhou H, Urso CJ, Jadeja V (2020) <p>saturated fatty acids in obesity-associated inflammation</p>. J Inflamm Res 13:1–14. https://doi.org/10.2147/JIR.S229691
Curtale G, Mirolo M, Renzi TA et al (2013) Negative regulation of toll-like receptor 4 signaling by IL-10-dependent microRNA-146b. Proc Natl Acad Sci U S A 110:11499–11504. https://doi.org/10.1073/pnas.1219852110
Clemenzi MN, Wellhauser L, Aljghami ME, Belsham DD (2019) Tumour necrosis factor α induces neuroinflammation and insulin resistance in immortalised hypothalamic neurones through independent pathways. J Neuroendocrinol 31:e12678. https://doi.org/10.1111/jne.12678
Hotamisligil GS, Murray DL, Choy LN, Spiegelman BM (1994) Tumor necrosis factor α inhibits signaling from the insulin receptor. Proc Natl Acad Sci U S A 91:4854–4858. https://doi.org/10.1073/pnas.91.11.4854
Aljada A, Ghanim H, Assian E, Dandona P (2002) Tumor necrosis factor-α inhibits insulin-induced increase in endothelial nitric oxide synthase and reduces insulin receptor content and phosphorylation in human aortic endothelial cells. Metabolism 51:487–491. https://doi.org/10.1053/meta.2002.31339
Obici S, Feng Z, Karkanias G et al (2002) Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci 5:566–572. https://doi.org/10.1038/nn0602-861
Richard AJ, Stephens JM (2019) Adipocyte-derived hormones. Hormonal signaling in biology and medicine: comprehensive modern endocrinology. Academic Press, Elsevier, pp 461–486
de Git KCG, Adan RAH (2015) Leptin resistance in diet-induced obesity: the role of hypothalamic inflammation. Obes Rev 16:207–224. https://doi.org/10.1111/obr.12243
Zhao S, Kusminski CM, Elmquist JK, Scherer PE (2020) Leptin: less is more. Diabetes 69:823–829. https://doi.org/10.2337/dbi19-0018
Bursać BN, Vasiljević AD, Nestorović NM et al (2014) High-fructose diet leads to visceral adiposity and hypothalamic leptin resistance in male rats—do glucocorticoids play a role? J Nutr Biochem 25:446–455. https://doi.org/10.1016/j.jnutbio.2013.12.005
Zhang Y, Scarpace PJ (2006) The role of leptin in leptin resistance and obesity. Physiol Behav 88:249–256. https://doi.org/10.1016/j.physbeh.2006.05.038
Casagrande B, Estadella D (2020) Withdrawing from obesogenic diets: benefits and barriers in the short- and long-term in rodent models. Am J Physiol Metab. https://doi.org/10.1152/ajpendo.00174.2020
Fullston T, McPherson NO, Owens JA et al (2015) Paternal obesity induces metabolic and sperm disturbances in male offspring that are exacerbated by their exposure to an “obesogenic” diet. Physiol Rep. https://doi.org/10.14814/phy2.12336
Funding
This study was supported by Fundação do Amparo à Pesquisa do Estado de São Paulo (FAPESP)—no. 2017/09646–1; 2019/09724–8, and financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001. LPP is recipient of National Council for Scientific and Technological Development (CNPq) fellowship and supported by FAPESP—no. 2019/09724–8.
Author information
Authors and Affiliations
Contributions
HC contributed with the animal care, experimental procedures, statistical analysis and writing. MNS, EAS, GJ, AS and AJ contributed to the animal care and experimental procedures. BC contributed with the statistical analysis. LPP contributed with the drafting and revising critical intellectual content. All authors have approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
394_2021_2690_MOESM1_ESM.tif
Supplementary file1 (TIF 571 kb) Paternal differences in body measurements, metabolic efficiency and adiposity between control diet (CD) and high-fat high-sugar (HFS) groups. A. Paternal body weight progress (g); B. Paternal weight gain (g) (Final weight – Initial weight); C. Paternal diet intake (g/week); D. Paternal metabolic efficiency weight gain (g)/ diet intake (g); E. Paternal Retroperitoneal Adipose Tissue (RET) relative weight (%); F. Paternal Total Visceral Adipose Tissue (VAT) relative weight (%); Data are expressed as mean ± SEM and *p≤0.05 was considered statistically significant compared to CD. Statistical test: ANOVA for repeated measures was used for A; U-Mann Whitney test (non-parametric data) was used for B and C, and unpaired T-test (parametric data) for D, E and F
394_2021_2690_MOESM2_ESM.tif
Supplementary file2 (TIF 604 kb) Maternal differences in body measurements, metabolic efficiency and adiposity between control diet (CD) and high-fat high-sugar (HFS) groups. A. Maternal body weight progress (g) during pregnancy and lactation; B. Maternal Weight gain (g) (Final weight – Initial weight) during pregnancy and lactation; C. Maternal diet intake (g) during pregnancy and lactation; D. Maternal metabolic efficiency (weight gain (g)/ diet intake (g) during pregnancy and lactation; E. Maternal Retroperitoneal Adipose Tissue (RET) relative weight (%); F. Maternal Total Visceral Adipose Tissue (VAT) relative weight (%); Data are expressed as mean ± SEM and *p≤0.05 was considered statistically significant compared to CD. Statistical test: ANOVA for repeated measures was used for A; U-Mann Whitney test (non-parametric data) was used for E and F, and unpaired T-test (parametric data) for B, C and D.
Rights and permissions
About this article
Cite this article
César, H., Sertorio, M.N., de Souza, E.A. et al. Parental high-fat high-sugar diet programming and hypothalamus adipose tissue axis in male Wistar rats. Eur J Nutr 61, 523–537 (2022). https://doi.org/10.1007/s00394-021-02690-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02690-1