Abstract
Purpose
Although emphasis has recently been placed on the importance of diet high in plant-based foods, the association between plant-based diet and long-term risk of overall and cause-specific mortality has been less studied. We aimed to investigate whether plant-based diet was associated with lower death risk.
Methods
This prospective cohort study used data from the US National Health and Nutrition Examination Survey. Diet was assessed using 24 h dietary recalls. We created three plant-based diet indices including an overall plant-based diet index (PDI), a healthful plant-based diet index (hPDI), and an unhealthful plant-based diet index (uPDI). Deaths from baseline until December 31, 2015, were identified. Multivariable-adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using Cox regression.
Results
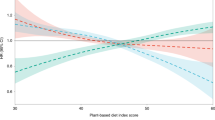
We documented 4904 deaths among 40,074 participants after a median follow-up of 7.8 years. Greater adherence to PDI was associated with lower risk of overall (HR comparing extreme quintiles 0.80, 95% CI 0.73, 0.89, ptrend < 0.001) and cancer-specific (HR = 0.68, 95% CI 0.55, 0.85, ptrend < 0.001) mortality. These inverse associations remained for hPDI and overall mortality with a HR of 0.86 (95% CI 0.77, 0.95, ptrend = 0.001), but not for cancer or CVD mortality. Conversely, uPDI was associated with higher risk of total (HR = 1.33, 95% CI 1.19, 1.48, ptrend < 0.001) and CVD-specific (HR = 1.42, 95% CI 1.12, 1.79, ptrend = 0.015) mortality.
Conclusions
Increased intake of a plant-based diet rich in healthier plant foods is associated with lower mortality risk, whereas a plant-based diet that emphasizes less-healthy plant foods is associated with high mortality risk among US adults.



Similar content being viewed by others
Availability of data and material
Data described in the manuscript, codebook, and analytic code will be made publicly and freely available without restriction at [https://www.cdc.gov/nchs/nhanes/index.htm].
Code availability
SAS version 9.4.
References
Collaborators USBoD, Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, Kasaeian A, Werdecker A, Carter A, Zipkin B, Sartorius B, Serdar B, Sykes BL, Troeger C, Fitzmaurice C, Rehm CD, Santomauro D, Kim D, Colombara D, Schwebel DC, Tsoi D, Kolte D, Nsoesie E, Nichols E, Oren E, Charlson FJ, Patton GC, Roth GA, Hosgood HD, Whiteford HA, Kyu H, Erskine HE, Huang H, Martopullo I, Singh JA, Nachega JB, Sanabria JR, Abbas K, Ong K, Tabb K, Krohn KJ, Cornaby L, Degenhardt L, Moses M, Farvid M, Griswold M, Criqui M, Bell M, Nguyen M, Wallin M, Mirarefin M, Qorbani M, Younis M, Fullman N, Liu P, Briant P, Gona P, Havmoller R, Leung R, Kimokoti R, Bazargan-Hejazi S, Hay SI, Yadgir S, Biryukov S, Vollset SE, Alam T, Frank T, Farid T, Miller T, Vos T, Barnighausen T, Gebrehiwot TT, Yano Y, Al-Aly Z, Mehari A, Handal A, Kandel A, Anderson B, Biroscak B, Mozaffarian D, Dorsey ER, Ding EL, Park EK, Wagner G, Hu G, Chen H, Sunshine JE, Khubchandani J, Leasher J, Leung J, Salomon J, Unutzer J, Cahill L, Cooper L, Horino M, Brauer M, Breitborde N, Hotez P, Topor-Madry R, Soneji S, Stranges S, James S, Amrock S, Jayaraman S, Patel T, Akinyemiju T, Skirbekk V, Kinfu Y, Bhutta Z, Jonas JB, Murray CJL (2018) The State of US Health, 1990–2016: burden of diseases, injuries, and risk factors among US States. JAMA 319(14):1444–1472. https://doi.org/10.1001/jama.2018.0158
Millen BE, Abrams S, Adams-Campbell L, Anderson CA, Brenna JT, Campbell WW, Clinton S, Hu F, Nelson M, Neuhouser ML, Perez-Escamilla R, Siega-Riz AM, Story M, Lichtenstein AH (2016) The 2015 dietary guidelines advisory committee scientific report: development and major conclusions. Adv Nutr 7(3):438–444. https://doi.org/10.3945/an.116.012120
Nelson ME, Hamm MW, Hu FB, Abrams SA, Griffin TS (2016) Alignment of healthy dietary patterns and environmental sustainability: a systematic review. Adv Nutr 7(6):1005–1025. https://doi.org/10.3945/an.116.012567
Kinlen LJ, Hermon C, Smith PG (1983) A proportionate study of cancer mortality among members of a vegetarian society. Br J Cancer 48(3):355–361. https://doi.org/10.1038/bjc.1983.200
Chang-Claude J, Frentzel-Beyme R, Eilber U (1992) Mortality pattern of German vegetarians after 11 years of follow-up. Epidemiology 3(5):395–401. https://doi.org/10.1097/00001648-199209000-00003
Key TJ, Thorogood M, Appleby PN, Burr ML (1996) Dietary habits and mortality in 11,000 vegetarians and health conscious people: results of a 17 year follow up. BMJ 313(7060):775–779. https://doi.org/10.1136/bmj.313.7060.775
Key TJ, Appleby PN, Davey GK, Allen NE, Spencer EA, Travis RC (2003) Mortality in British vegetarians: review and preliminary results from EPIC-Oxford. Am J Clin Nutr 78(3 Suppl):533s–538s. https://doi.org/10.1093/ajcn/78.3.533S
Orlich MJ, Singh PN, Sabate J, Jaceldo-Siegl K, Fan J, Knutsen S, Beeson WL, Fraser GE (2013) Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med 173(13):1230–1238. https://doi.org/10.1001/jamainternmed.2013.6473
Appleby PN, Crowe FL, Bradbury KE, Travis RC, Key TJ (2016) Mortality in vegetarians and comparable nonvegetarians in the United Kingdom. Am J Clin Nutr 103(1):218–230. https://doi.org/10.3945/ajcn.115.119461
Bao Y, Han J, Hu FB, Giovannucci EL, Stampfer MJ, Willett WC, Fuchs CS (2013) Association of nut consumption with total and cause-specific mortality. N Engl J Med 369(21):2001–2011. https://doi.org/10.1056/NEJMoa1307352
Aune D, Keum N, Giovannucci E, Fadnes LT, Boffetta P, Greenwood DC, Tonstad S, Vatten LJ, Riboli E, Norat T (2016) Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ 353:i2716. https://doi.org/10.1136/bmj.i2716
Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (2014) Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 349:g4490. https://doi.org/10.1136/bmj.g4490
Muraki I, Rimm EB, Willett WC, Manson JE, Hu FB, Sun Q (2016) Potato consumption and risk of type 2 diabetes: results from three prospective cohort studies. Diabetes Care 39(3):376–384. https://doi.org/10.2337/dc15-0547
Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB (2014) Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med 174(4):516–524. https://doi.org/10.1001/jamainternmed.2013.13563
Veronese N, Stubbs B, Noale M, Solmi M, Vaona A, Demurtas J, Nicetto D, Crepaldi G, Schofield P, Koyanagi A, Maggi S, Fontana L (2017) Fried potato consumption is associated with elevated mortality: an 8 y longitudinal cohort study. Am J Clin Nutr 106(1):162–167. https://doi.org/10.3945/ajcn.117.154872
Malik VS, Li Y, Pan A, De Koning L, Schernhammer E, Willett WC, Hu FB (2019) Long-term consumption of sugar-sweetened and artificially sweetened beverages and risk of mortality in US Adults. Circulation 139(18):2113–2125. https://doi.org/10.1161/CIRCULATIONAHA.118.037401
Steffen LM, Jacobs DR Jr, Stevens J, Shahar E, Carithers T, Folsom AR (2003) Associations of whole-grain, refined-grain, and fruit and vegetable consumption with risks of all-cause mortality and incident coronary artery disease and ischemic stroke: the atherosclerosis risk in communities (ARIC) Study. Am J Clin Nutr 78(3):383–390. https://doi.org/10.1093/ajcn/78.3.383
Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, Willett WC, Manson JE, Sun Q, Hu FB (2016) Plant-based dietary patterns and incidence of type 2 diabetes in us men and women: results from three prospective cohort studies. PLoS Med. https://doi.org/10.1371/journal.pmed.1002039
Martinez-Gonzalez MA, Sanchez-Tainta A, Corella D, Salas-Salvado J, Ros E, Aros F, Gomez-Gracia E, Fiol M, Lamuela-Raventos RM, Schroder H, Lapetra J, Serra-Majem L, Pinto X, Ruiz-Gutierrez V, Estruch R, Group P (2014) A provegetarian food pattern and reduction in total mortality in the Prevencion con Dieta Mediterranea (PREDIMED) study. Am J Clin Nutr 100(Suppl 1):320S-328S. https://doi.org/10.3945/ajcn.113.071431
Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Coresh J, Rebholz CM (2019) Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. J Am Heart Assoc. https://doi.org/10.1161/jaha.119.012865
Kim H, Caulfield LE, Rebholz CM (2018) Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J Nutr 148(4):624–631. https://doi.org/10.1093/jn/nxy019
Baden MY, Liu G, Satija A, Li Y, Sun Q, Fung TT, Rimm EB, Willett WC, Hu FB, Bhupathiraju SN (2019) Changes in plant-based diet quality and total and cause-specific mortality. Circulation 140(12):979–991. https://doi.org/10.1161/circulationaha.119.041014
Molina-Montes E, Salamanca-Fernández E, Garcia-Villanova B, Sánchez MJ (2020) The impact of plant-based dietary patterns on cancer-related outcomes: a rapid review and meta-analysis. Nutrients. https://doi.org/10.3390/nu12072010
Kant AK, Graubard BI, Schatzkin A (2004) Dietary patterns predict mortality in a national cohort: the National Health Interview Surveys, 1987 and 1992. J Nutr 134(7):1793–1799. https://doi.org/10.1093/jn/134.7.1793
Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB (2008) Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation 118(3):230–237. https://doi.org/10.1161/CIRCULATIONAHA.108.771881
Stewart RA, Wallentin L, Benatar J, Danchin N, Hagstrom E, Held C, Husted S, Lonn E, Stebbins A, Chiswell K, Vedin O, Watson D, White HD, Investigators S (2016) Dietary patterns and the risk of major adverse cardiovascular events in a global study of high-risk patients with stable coronary heart disease. Eur Heart J 37(25):1993–2001. https://doi.org/10.1093/eurheartj/ehw125
Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) (2017) About the National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed on 11 March 2021
Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C (2016) Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr 7(1):121–134. https://doi.org/10.3945/an.115.009258
Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V (2006) A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc 106(10):1575–1587. https://doi.org/10.1016/j.jada.2006.07.003
Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, Rexrode KM, Rimm EB, Hu FB (2017) Healthful and unhealthful plant based diets and the risk of coronary heart disease in U. S. Adults. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2017.05.047
Guasch-Ferre M, Hu FB (2019) Are fruit juices just as unhealthy as sugar-sweetened beverages? JAMA Netw Open 2(5):e193109. https://doi.org/10.1001/jamanetworkopen.2019.3109
Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) (2021) NHANES Laboratory Data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Laboratory. Accessed on 11 March 2021
Schwingshackl L, Schwedhelm C, Hoffmann G, Lampousi AM, Knuppel S, Iqbal K, Bechthold A, Schlesinger S, Boeing H (2017) Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr 105(6):1462–1473. https://doi.org/10.3945/ajcn.117.153148
Ruby MB (2012) Vegetarianism A blossoming field of study. Appetite 58(1):141–150. https://doi.org/10.1016/j.appet.2011.09.019
Liese AD, Krebs-Smith SM, Subar AF, George SM, Harmon BE, Neuhouser ML, Boushey CJ, Schap TE, Reedy J (2015) The dietary patterns methods project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr 145(3):393–402. https://doi.org/10.3945/jn.114.205336
Gardener H, Rundek T, Wright CB, Elkind MS, Sacco RL (2013) Coffee and tea consumption are inversely associated with mortality in a multiethnic urban population. J Nutr 143(8):1299–1308. https://doi.org/10.3945/jn.112.173807
Ding M, Satija A, Bhupathiraju SN, Hu Y, Sun Q, Han J, Lopez-Garcia E, Willett W, van Dam RM, Hu FB (2015) Association of coffee consumption with total and cause-specific mortality in 3 large prospective cohorts. Circulation 132(24):2305–2315. https://doi.org/10.1161/circulationaha.115.017341
Ma Y, Hebert JR, Li W, Bertone-Johnson ER, Olendzki B, Pagoto SL, Tinker L, Rosal MC, Ockene IS, Ockene JK, Griffith JA, Liu S (2008) Association between dietary fiber and markers of systemic inflammation in the Women’s Health Initiative Observational Study. Nutrition 24(10):941–949. https://doi.org/10.1016/j.nut.2008.04.005
Cassidy A, Rogers G, Peterson JJ, Dwyer JT, Lin H, Jacques PF (2015) Higher dietary anthocyanin and flavonol intakes are associated with anti-inflammatory effects in a population of US adults. Am J Clin Nutr 102(1):172–181. https://doi.org/10.3945/ajcn.115.108555
Ishikawa T, Suzukawa M, Ito T, Yoshida H, Ayaori M, Nishiwaki M, Yonemura A, Hara Y, Nakamura H (1997) Effect of tea flavonoid supplementation on the susceptibility of low-density lipoprotein to oxidative modification. Am J Clin Nutr 66(2):261–266. https://doi.org/10.1093/ajcn/66.2.261
Mozaffarian D, Wu JH (2011) Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol 58(20):2047–2067. https://doi.org/10.1016/j.jacc.2011.06.063
van Dam RM, Hu FB (2005) Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA 294(1):97–104. https://doi.org/10.1001/jama.294.1.97
Kroenke CH, Kwan ML, Sweeney C, Castillo A, Caan BJ (2013) High- and low-fat dairy intake, recurrence, and mortality after breast cancer diagnosis. J Natl Cancer Inst 105(9):616–623. https://doi.org/10.1093/jnci/djt027
Lu W, Chen H, Niu Y, Wu H, Xia D, Wu Y (2016) Dairy products intake and cancer mortality risk: a meta-analysis of 11 population-based cohort studies. Nutr J 15(1):91. https://doi.org/10.1186/s12937-016-0210-9
Huang J, Liao LM, Weinstein SJ, Sinha R, Graubard BI, Albanes D (2020) Association between plant and animal protein intake and overall and cause-specific mortality. JAMA Intern Med 180(9):1173–1184. https://doi.org/10.1001/jamainternmed.2020.2790
Holmes MD, Pollak MN, Willett WC, Hankinson SE (2002) Dietary correlates of plasma insulin-like growth factor I and insulin-like growth factor binding protein 3 concentrations. Cancer Epidemiol Biomarkers Prev 11(9):852–861
Allen NE, Appleby PN, Davey GK, Kaaks R, Rinaldi S, Key TJ (2002) The associations of diet with serum insulin-like growth factor I and its main binding proteins in 292 women meat-eaters, vegetarians, and vegans. Cancer Epidemiol Biomarkers Prev 11(11):1441–1448. https://doi.org/10.1001/jamainternmed.2013.6473
Smith CJ, Scott SM, Wagner BM (1998) The necessary role of the autopsy in cardiovascular epidemiology. Hum Pathol 29(12):1469–1479. https://doi.org/10.1016/s0046-8177(98)90018-1
Pagidipati NJ, Gaziano TA (2013) Estimating deaths from cardiovascular disease: a review of global methodologies of mortality measurement. Circulation 127(6):749–756. https://doi.org/10.1161/CIRCULATIONAHA.112.128413
Jurek AM, Greenland S, Maldonado G, Church TR (2005) Proper interpretation of non-differential misclassification effects: expectations vs observations. Int J Epidemiol 34(3):680–687. https://doi.org/10.1093/ije/dyi060
Acknowledgements
Drs Li and Yang had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Yang and Li. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: Li and Yang. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: Li and Zhu. Obtained funding: Yang. Administrative, technical, or material support: Yang. Study supervision: Yang.
Funding
This work was supported by the National Natural Science Foundation of China (82073651), Anhui Provincial Natural Science Foundation (2008085MH262), and a grant of the Scientific Research of BSKY from Anhui Medical University (XJ201935).
Author information
Authors and Affiliations
Contributions
Hairong Li and Wanshui Yang had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Wanshui Yang and Hairong Li Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: Hairong Li and Wanshui Yang. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: Hairong Li and Yu Zhu. Obtained funding: Wanshui Yang. Administrative, technical, or material support: Wanshui Yang. Study supervision: Wanshui Yang.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical approval
The National Centers for Health Statistics approved the NHANES study protocol. The Institutional Review Board at our institute determined that this analysis used a public dataset, so human subjects’ approval was waived.
Consent to participate
All participants provided the written informed consent.
Consent for publication
All of the authors have read and approved the final version of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, H., Zeng, X., Wang, Y. et al. A prospective study of healthful and unhealthful plant-based diet and risk of overall and cause-specific mortality. Eur J Nutr 61, 387–398 (2022). https://doi.org/10.1007/s00394-021-02660-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02660-7