Abstract
Purpose
In previous studies, short-chain fatty acids (SCFAs) have been found to regulate gut microbiota and change gut barrier status, and the potential positive effects of SCFAs on inflammatory bowel disease (IBD), type 1 diabetes mellitus (T1D), and non-alcoholic fatty liver disease (NAFLD) have also been found, but the role of SCFAs in these three diseases is not clear. This review aims to summarize existing evidence on the effects of SCFAs on IBD, T1D, and NHFLD, and correlates them with gut barrier and gut microbiota (gut microbiota barrier).
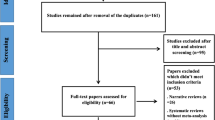
Methods
A literature search in PubMed, Web of Science, Springer, and Wiley Online Library up to October 2020 was conducted for all relevant studies published.
Results
This is a retrospective review of 150 applied research articles or reviews. The destruction of gut barrier may promote the development of IBD, T1D, and NAFLD. SCFAs seem to maintain the gut barrier by promoting the growth of intestinal epithelial cells, strengthening the intestinal tight connection, and regulating the activities of gut microbiota and immune cells, which might result possible beneficial effects on the above three diseases at a certain dose.
Conclusions
Influencing gut barrier health may be a bridge for SCFAs (especially butyrate) to have positive effects on IBD, T1D, and NAFLD. It is expected that this article can provide new ideas for the subsequent research on the treatment of diseases by SCFAs and help SCFAs be better applied to precise and personalized treatment.


Similar content being viewed by others
Abbreviations
- SCFAs:
-
Short-chain fatty acids
- IBD:
-
Inflammatory bowel disease
- T1D:
-
Type 1 diabetes mellitus
- NAFLD:
-
Non-alcoholic fatty liver disease
- HDAC:
-
Inhibiting histone deacetylase
- GPR:
-
G protein-coupled receptors on cells
- IECs:
-
Intestinal epithelial cells
- TJ:
-
Tight junction
- AJ:
-
Adhesion junction
- Treg:
-
Regulatory T cell
- Th:
-
T helper cell
- IL-x:
-
Interleukin-x
- IFN-γ:
-
Interferon-γ
- TLR2:
-
Toll-like receptor 2
- TRAF6:
-
TNF receptor-related factor 6
- MCD:
-
Methionine choline deficiency
- ERK:
-
Extracellular-regulated protein kinases
- NASH:
-
Non-alcoholic steatohepatitis
- DSS:
-
Dextran sulfate sodium
- NF-κ b:
-
Nuclear factor-κ b
References
Scheppach W (1994) Effects of short chain fatty acids on gut morphology and function. Gut 35(1 Suppl):S35-38. https://doi.org/10.1136/gut.35.1_suppl.s35
Cummings JH, Pomare EW, Branch WJ, Naylor CP, Macfarlane GT (1987) Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut 28(10):1221–1227. https://doi.org/10.1136/gut.28.10.1221
Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, Serino M, Tilg H, Watson A, Wells JM (2014) Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterol 14:189. https://doi.org/10.1186/s12876-014-0189-7
Postler TS, Ghosh S (2017) Understanding the holobiont: how microbial metabolites affect human health and shape the immune system. Cell Metab 26(1):110–130
Donohoe DR, Collins LB, Wali A, Bigler R, Sun W, Bultman SJ (2012) The warburg effect dictates the mechanism of butyrate-mediated histone acetylation and cell proliferation. Mol Cell 48(4):612–626
Gurav A, Sivaprakasam S, Bhutia YD, Boettger T, Singh N, Ganapathy V (2015) Slc5a8, a Na+-coupled high-affinity transporter for short-chain fatty acids, is a conditional tumour suppressor in colon that protects against colitis and colon cancer under low-fibre dietary conditions. Biochem J 469:267–278
Kaisar MMM, Pelgrom LR, van der Ham AJ, Yazdanbakhsh M, Everts B (2017) Butyrate conditions human Dendritic cells to Prime Type 1 regulatory T cells via both histone Deacetylase inhibition and G Protein-coupled receptor 109A signaling. Front Immunol 8:1429. https://doi.org/10.3389/fimmu.2017.01429
Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ (2003) The Orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem 278(13):11312–11319. https://doi.org/10.1074/jbc.M211609200
Namkung H, Yu H, Gong J, Leeson S (2011) Antimicrobial activity of butyrate glycerides toward salmonella typhimurium and clostridium perfringens. Poult Sci 90(10):2217–2222. https://doi.org/10.3382/ps.2011-01498
Parada Venegas D, De la Fuente MK, Landskron G, Gonzalez MJ, Quera R, Dijkstra G, Harmsen HJM, Faber KN, Hermoso MA (2019) Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol 10:277. https://doi.org/10.3389/fimmu.2019.00277
Dou X, Gao N, Lan J, Han J, Yang Y, Shan A (2020) TLR2/EGFR are two sensors for pBD3 and pEP2C induction by sodium butyrate independent of HDAC inhibition. J Agric Food Chem 68(2):512–522. https://doi.org/10.1021/acs.jafc.9b06569
Sanchez HN, Moroney JB, Gan H, Shen T, Im JL, Li T, Taylor JR, Zan H, Casali P (2020) B cell-intrinsic epigenetic modulation of antibody responses by dietary fiber-derived short-chain fatty acids. Nature Commun 11(1):60. https://doi.org/10.1038/s41467-019-13603-6
Wu W, Xiao ZB, An WY, Dong YY, Zhang BK (2018) Dietary sodium butyrate improves intestinal development and function by modulating the microbial community in broilers. Plos One 13(5):e0197762. https://doi.org/10.1371/journal.pone.0197762
Oh TJ, Sul WJ, Oh HN, Lee YK, Lim HL, Choi SH, Park KS, Jang HC (2019) Butyrate attenuated fat gain through gut microbiota modulation in db/db mice following dapagliflozin treatment. Sci Rep 9:20300. https://doi.org/10.1038/s41598-019-56684-5
Jia JL, Nie L, Liu Y (2020) Butyrate alleviates inflammatory response and NF-kappa B activation in human degenerated intervertebral disc tissues. Int Immunopharmacol 78:106004. https://doi.org/10.1038/s41598-019-56684-5
Artis D (2008) Epithelial-cell recognition of commensal bacteria and maintenance of immune homeostasis in the gut. Nat Rev Immunol 8(6):411–420. https://doi.org/10.1038/nri2316
Rees WD, Sly LM, Steiner TS (2020) How do immune and mesenchymal cells influence the intestinal epithelial cell compartment in inflammatory bowel disease? Let’s crosstalk about it! J Leukoc Biol. https://doi.org/10.1002/jlb.3mir0120-567r
Salvo Romero E, Alonso Cotoner C, Pardo Camacho C, Casado Bedmar M, Vicario M (2015) The intestinal barrier function and its involvement in digestive disease. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva 107(11):686–696. https://doi.org/10.17235/reed.2015.3846/2015
Scaldaferri F, Pizzoferrato M, Gerardi V, Lopetuso L, Gasbarrini A (2012) The gut barrier: new acquisitions and therapeutic approaches. J Clin Gastroenterol 46(Suppl):S12-17. https://doi.org/10.1097/MCG.0b013e31826ae849
Peng LY, Li ZR, Green RS, Holzman IR, Lin J (2009) Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr 139(9):1619–1625
Huang XZ, Li ZR, Zhu LB, Huang HY, Hou LL, Lin J (2014) Inhibition of p38 mitogen-activated protein kinase attenuates butyrate-induced intestinal barrier impairment in a Caco-2 cell monolayer model. J Pediatr Gastr Nutr 59(2):264–269
Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer RJ (2008) Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther 27(2):104–119. https://doi.org/10.1111/j.1365-2036.2007.03562.x
Liu H, Wang J, He T, Becker S, Zhang GL, Li DF, Ma X (2018) Butyrate: a double-edged sword for health? Adv Nutr 9(1):21–29
Baumgart DC, Sandborn WJ (2007) Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet 369(9573):1641–1657. https://doi.org/10.1016/S0140-6736(07)60751-X
Michielan A, D’Inca R (2015) Intestinal Permeability in Inflammatory Bowel Disease: Pathogenesis, Clinical Evaluation, and Therapy of Leaky Gut. Mediat Inflamm. https://doi.org/10.1155/2015/628157
Salim SY, Soderholm JD (2011) Importance of disrupted intestinal barrier in inflammatory bowel diseases. Inflamm Bowel Dis 17(1):362–381. https://doi.org/10.1002/ibd.21403
Noth R, Stüber E, Häsler R, Nikolaus S, Kühbacher T, Hampe J, Bewig B, Schreiber S, Arlt A (2012) Anti-TNF-α antibodies improve intestinal barrier function in Crohn’s disease. J Crohn’s Colitis 6(4):464–469. https://doi.org/10.1016/j.crohns.2011.10.004
Chen GX, Ran X, Li B, Li YH, He DW, Huang BX, Fu SP, Liu JX, Wang W (2018) Sodium butyrate inhibits inflammation and maintains epithelium barrier integrity in a TNBS-induced inflammatory bowel disease mice model. Ebiomedicine 30:317–325
Zou X, Ji J, Qu H, Wang J, Shu DM, Wang Y, Liu TF, Li Y, Luo CL (2019) Effects of sodium butyrate on intestinal health and gut microbiota composition during intestinal inflammation progression in broilers. Poult Sci 98(10):4449–4456. https://doi.org/10.3382/ps/pez279
Liu CS, Liang X, Wei XH, Jin Z, Chen FL, Tang QF, Tan XM (2019) Gegen qinlian decoction treats diarrhea in piglets by modulating gut microbiota and short-chain fatty acids. Front Microbiol 10:825. https://doi.org/10.3389/fmicb.2019.00825
Van Belle TL, Coppieters KT, Von Herrath MG (2011) Type 1 diabetes: etiology, immunology, and therapeutic strategies. Physiol Rev 91(1):79–118
de Kort S, Keszthelyi D, Masclee AAM (2011) Leaky gut and diabetes mellitus: what is the link? Obes Rev 12(6):449–458
Quesada-Vazquez S, Aragones G, Del Bas JM, Escote X (2020) Diet, gut microbiota and non-alcoholic fatty liver disease: Three parts of the same axis. Cells. https://doi.org/10.3390/cells9010176
Zhou D, Fan JG (2019) Microbial metabolites in non-alcoholic fatty liver disease. World J Gastroenterol 25(17):2019–2028. https://doi.org/10.3748/wjg.v25.i17.2019
Cui Y, Wang Q, Chang R, Zhou X, Xu C (2019) Intestinal barrier function-non-alcoholic fatty liver disease interactions and possible role of gut microbiota. J Agric Food Chem 67(10):2754–2762. https://doi.org/10.1021/acs.jafc.9b00080
Mandaliya DK, Seshadri S (2019) Short chain fatty acids, pancreatic dysfunction and type 2 diabetes (vol 19, pg 280, 2019). Pancreatology 19(4):616–616
Rosado CP, Rosa VHC, Martins BC, Soares AC, Santos IB, Monteiro EB, Moura-Nunes N, da Costa CA, Mulder ADP, Daleprane JB (2020) Resistant starch from green banana (Musa sp.) attenuates non-alcoholic fat liver accumulation and increases short-chain fatty acids production in high-fat diet-induced obesity in mice. Int J Biol Macromol 145:1066–1072
Vancamelbeke M, Vermeire S (2017) The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol 11(9):821–834. https://doi.org/10.1080/17474124.2017.1343143
Van der Sluis M, De Koning BA, De Bruijn AC, Velcich A, Meijerink JP, Van Goudoever JB, Buller HA, Dekker J, Van Seuningen I, Renes IB, Einerhand AW (2006) Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology 131(1):117–129. https://doi.org/10.1053/j.gastro.2006.04.020
Brandtzaeg P (1995) Molecular and cellular aspects of the secretory immunoglobulin system. APMIS : acta pathologica, microbiologica, et immunologica Scandinavica 103(1):1–19. https://doi.org/10.1111/j.1699-0463.1995.tb01073.x
Bevins CL, Salzman NH (2011) Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat Rev Microbiol 9(5):356–368. https://doi.org/10.1038/nrmicro2546
Jakobsson HE, Rodriguez-Pineiro AM, Schutte A, Ermund A, Boysen P, Bemark M, Sommer F, Backhed F, Hansson GC, Johansson ME (2015) The composition of the gut microbiota shapes the colon mucus barrier. EMBO Rep 16(2):164–177. https://doi.org/10.15252/embr.201439263
Pelaseyed T, Bergstrom JH, Gustafsson JK, Ermund A, Birchenough GM, Schutte A, van der Post S, Svensson F, Rodriguez-Pineiro AM, Nystrom EE, Wising C, Johansson ME, Hansson GC (2014) The mucus and mucins of the goblet cells and enterocytes provide the first defense line of the gastrointestinal tract and interact with the immune system. Immunol Rev 260(1):8–20. https://doi.org/10.1111/imr.12182
Ugolev AM, De Laey P (1973) Membrane digestion. A concept of enzyme hydrolysis on cell membranes. Biochimica et biophysica acta 300(2):105–128. https://doi.org/10.1016/0304-4157(73)90001-4
Park J, Kotani T, Konno T, Setiawan J, Kitamura Y, Imada S, Usui Y, Hatano N, Shinohara M, Saito Y, Murata Y, Matozaki T (2016) Promotion of intestinal epithelial cell turnover by commensal bacteria: role of short-chain fatty acids. PLoS ONE. https://doi.org/10.1371/journal.pone.0156334
Groschwitz KR, Hogan SP (2009) Intestinal barrier function: molecular regulation and disease pathogenesis. J Allergy Clin Immunol 124(1):3–20. https://doi.org/10.1016/j.jaci.2009.05.038
Kiesslich R, Goetz M, Angus EM, Hu Q, Guan Y, Potten C, Allen T, Neurath MF, Shroyer NF, Montrose MH, Watson AJ (2007) Identification of epithelial gaps in human small and large intestine by confocal endomicroscopy. Gastroenterology 133(6):1769–1778. https://doi.org/10.1053/j.gastro.2007.09.011
Eisenhoffer GT, Loftus PD, Yoshigi M, Otsuna H, Chien CB, Morcos PA, Rosenblatt J (2012) Crowding induces live cell extrusion to maintain homeostatic cell numbers in epithelia. Nature 484(7395):546–549. https://doi.org/10.1038/nature10999
Parker A, Vaux L, Patterson AM, Modasia A, Muraro D, Fletcher AG, Byrne HM, Maini PK, Watson AJM, Pin C (2019) Elevated apoptosis impairs epithelial cell turnover and shortens villi in TNF-driven intestinal inflammation. Cell Death Dis 10:108. https://doi.org/10.1038/s41419-018-1275-5
Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, Granucci F, Kraehenbuhl JP, Ricciardi-Castagnoli P (2001) Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol 2(4):361–367. https://doi.org/10.1038/86373
Li Z, Zhang C, Zhou Z, Zhang J, Zhang J, Tian Z (2012) Small intestinal intraepithelial lymphocytes expressing CD8 and T cell receptor gammadelta are involved in bacterial clearance during Salmonella enterica serovar Typhimurium infection. Infect Immun 80(2):565–574. https://doi.org/10.1128/IAI.05078-11
Pull SL, Doherty JM, Mills JC, Gordon JI, Stappenbeck TS (2005) Activated macrophages are an adaptive element of the colonic epithelial progenitor niche necessary for regenerative responses to injury. Proc Natl Acad Sci USA 102(1):99–104
Turner JR (2009) Intestinal mucosal barrier function in health and disease. Nat Rev Immunol 9(11):799–809. https://doi.org/10.1038/nri2653
Cirera I, Bauer TM, Navasa M, Vila J, Grande L, Taura P, Fuster J, Garcia-Valdecasas JC, Lacy A, Suarez MJ, Rimola A, Rodes J (2001) Bacterial translocation of enteric organisms in patients with cirrhosis. J Hepatol 34(1):32–37. https://doi.org/10.1016/s0168-8278(00)00013-1
Valadez JMA, Rivera-Espinosa L, Mendez-Guerrero O, Chavez-Pacheco JL, Juarez IG, Torre A (2016) Intestinal permeability in a patient with liver cirrhosis. Ther Clin Risk Manag 12:1729–1748
Miller TL, Wolin MJ (1996) Pathways of acetate, propionate, and butyrate formation by the human fecal microbial flora. Appl Environ Microbiol 62(5):1589–1592
Derrien M, Vaughan EE, Plugge CM, de Vos WM (2004) Akkermansia muciniphila gen. nov., sp nov., a human intestinal mucin-degrading bacterium. Int J Syst Evol Micr 54:1469–1476
Louis P, Young P, Holtrop G, Flint HJ (2010) Diversity of human colonic butyrate-producing bacteria revealed by analysis of the butyryl-CoA:acetate CoA-transferase gene. Environ Microbiol 12(2):304–314. https://doi.org/10.1111/j.1462-2920.2009.02066.x
Lu YY, Fan CN, Li P, Lu YF, Chang XL, Qi KM (2016) Short chain fatty acids prevent high-fat-diet-induced obesity in mice by regulating G protein-coupled receptors and gut microbiota. Sci Rep 6(2016):37589. https://doi.org/10.1038/srep37589
Yu CX, Liu SJ, Chen LQ, Shen J, Niu YM, Wang TY, Zhang WQ, Fu L (2019) Effect of exercise and butyrate supplementation on microbiota composition and lipid metabolism. J Endocrinol 243(2):125–135
Zhai SX, Qin S, Li LL, Zhu LM, Zou ZQ, Wang L (2019) Dietary butyrate suppresses inflammation through modulating gut microbiota in high-fat diet-fed mice. Fems Microbiol Lett 366(13):153. https://doi.org/10.1093/femsle/fnz153
Zhao L, Zhang Q, Ma WN, Tian F, Shen HY, Zhou MM (2017) A combination of quercetin and resveratrol reduces obesity in high-fat diet-fed rats by modulation of gut microbiota. Food Funct 8(12):4644–4656
He JW, Guo HD, Zheng WJ, Yao W (2019) Effects of stress on the mucus-microbial interactions in the gut. Curr Protein Pept Sc 20(2):155–163. https://doi.org/10.2174/1389203719666180514152406
Xing PY, Pettersson S, Kundu P (2020) Microbial metabolites and intestinal stem cells tune intestinal homeostasis. Proteomics. https://doi.org/10.1002/Pmic.201800419
Satokari R (2015) Contentious host-microbiota relationship in inflammatory bowel disease - can foes become friends again? Scand J Gastroentero 50(1):34–42
Geirnaert A, Calatayud M, Grootaert C, Laukens D, Devriese S, Smagghe G, De Vos M, Boon N, Van de Wiele T (2017) Butyrate-producing bacteria supplemented in vitro to Crohn’s disease patient microbiota increased butyrate production and enhanced intestinal epithelial barrier integrity. Sci Rep 7:11450. https://doi.org/10.1038/s41598-017-11734-8
Zhou D, Pan Q, Xin F-Z, Zhang R-N, He C-X, Chen G-y, Liu C, Chen Y-W, Fan J-G (2017) Sodium butyrate attenuates high-fat diet-induced steatohepatitis in mice by improving gut microbiota and gastrointestinal barrier. World J Gastroenterol 23:60. https://doi.org/10.3748/wjg.v23.i1.60
Lamas A, Regal P, Vazquez B, Cepeda A, Franco CM (2019) Short chain fatty acids commonly produced by gut microbiota influence salmonella enterica motility, biofilm formation, and gene expression. Antibiotics. https://doi.org/10.3390/antibiotics8040265
da Silva BC, Vieira FD, Mourino JLP, Bolivar N, Seiffert WQ (2016) Butyrate and propionate improve the growth performance of Litopenaeus vannamei. Aquac Res 47(2):612–623
Alva-Murillo N, Ochoa-Zarzosa A, Lopez-Meza JE (2012) Short chain fatty acids (propionic and hexanoic) decrease Staphylococcus aureus internalization into bovine mammary epithelial cells and modulate antimicrobial peptide expression. Vet Microbiol 155(2–4):324–331
Sunkara LT, Jiang W, Zhang G (2012) Modulation of antimicrobial host defense peptide gene expression by free fatty acids. PLoS ONE 7(11):e49558. https://doi.org/10.1371/journal.pone.0049558
Jung TH, Park JH, Jeon WM, Han KS (2015) Butyrate modulates bacterial adherence on LS174T human colorectal cells by stimulating mucin secretion and MAPK signaling pathway. Nutr Res Pract 9(4):343–349. https://doi.org/10.4162/nrp.2015.9.4.343
Dekker J, Rossen JWA, Buller HA, Einerhand AWC (2002) The MUC family: an obituary. Trends Biochem Sci 27(3):126–131
Williams SJ, Munster DJ, Quin RJ, Gotley DC, McGuckin MA (1999) The MUC3 gene encodes a transmembrane mucin and is alternatively spliced. Biochem Bioph Res Co 261(1):83–89
Gaudier E, Jarry A, Blottiere HM, de Coppet P, Buisine MP, Aubert JP, Laboisse C, Cherbut C, Hoebler C (2004) Butyrate specifically modulates MUC gene expression in intestinal epithelial goblet cells deprived of glucose. Am J Physiol Gastr L 287(6):G1168–G1174
Augenlicht L, Shi L, Mariadason J, Laboisse C, Velcich A (2003) Repression of MUC2 gene expression by butyrate, a physiological regulator of intestinal cell maturation. Oncogene 22(32):4983–4992
Wrzosek L, Miquel S, Noordine ML, Bouet S, Chevalier-Curt MJ, Robert V, Philippe C, Bridonneau C, Cherbuy C, Robbe-Masselot C, Langella P, Thomas M (2013) Bacteroides thetaiotaomicron and Faecalibacterium prausnitzii influence the production of mucus glycans and the development of goblet cells in the colonic epithelium of a gnotobiotic model rodent. BMC Biol 11:61. https://doi.org/10.1186/1741-7007-11-61
Kaden-Volynets V, Gunther C, Zimmermann J, Beisner J, Becker C, Bischoff SC (2019) Deletion of the Casp8 gene in mice results in ileocolitis, gut barrier dysfunction, and malassimilation, which can be partially attenuated by inulin or sodium butyrate. Am J Physiol Gastr L 317(4):G493–G507
Okumura R, Takeda K (2018) Maintenance of intestinal homeostasis by mucosal barriers. Inflamm Regener 38:5. https://doi.org/10.1186/s41232-018-0063-z
Chen JL, Zhai ZY, Long HR, Yang GM, Deng BC, Deng JP (2020) Inducible expression of defensins and cathelicidins by nutrients and associated regulatory mechanisms. Peptides 123:170177. https://doi.org/10.1016/j.peptides.2019.170177
Cheng D, Xu JH, Li JY, Wang SY, Wu TF, Chen QK, Yu T (2018) Butyrate ameliorated-NLRC3 protects the intestinal barrier in a GPR43-dependent manner. Exp Cell Res 368(1):101–110. https://doi.org/10.1016/j.yexcr.2018.04.018
Yan H, Ajuwon KM (2017) Butyrate modifies intestinal barrier function in IPEC-J2 cells through a selective upregulation of tight junction proteins and activation of the Akt signaling pathway. PLoS ONE 12(6):e0179586. https://doi.org/10.1371/journal.pone.0179586
Nastasi C, Fredholm S, Willerslev-Olsen A, Hansen M, Bonefeld CM, Geisler C, Andersen MH, Ødum N, Woetmann A (2017) Butyrate and propionate inhibit antigen-specific CD8+ T cell activation by suppressing IL-12 production by antigen-presenting cells. Sci Rep 7(1):14516. https://doi.org/10.1038/s41598-017-15099-w
Nastasi C, Candela M, Bonefeld CM, Geisler C, Hansen M, Krejsgaard T, Biagi E, Andersen MH, Brigidi P, Odum N, Litman T, Woetmann A (2015) The effect of short-chain fatty acids on human monocyte-derived dendritic cells. Sci Rep 5:16148. https://doi.org/10.1038/srep16148
Park J, Kim M, Kang S, Jannasch A, Cooper B, Patterson J, Kim C (2014) Short-chain fatty acids induce both effector and regulatory T cells by suppression of histone deacetylases and regulation of the mTOR-S6K pathway. Mucosal Immunol. https://doi.org/10.1038/mi.2014.44
Martin-Gallausiaux C, Beguet-Crespel F, Marinelli L, Jamet A, Ledue F, Blottiere HM, Lapaque N (2018) Butyrate produced by gut commensal bacteria activates TGF-beta1 expression through the transcription factor SP1 in human intestinal epithelial cells. Sci Rep. https://doi.org/10.1038/S41598-018-28048-Y
Schulthess J, Pandey S, Capitani M, Rue-Albrecht KC, Arnold I, Franchini F, Chomka A, Ilott NE, Johnston DGW, Pires E, McCullagh J, Sansom SN, Arancibia-Carcamo CV, Uhlig HH, Powrie F (2019) The short chain fatty acid butyrate imprints an antimicrobial program in macrophages. Immunity 50(2):432-445e437. https://doi.org/10.1016/j.immuni.2018.12.018
Maslowski KM, Vieira AT, Ng A, Kranich J, Sierro F, Yu D, Schilter HC, Rolph MS, Mackay F, Artis D, Xavier RJ, Teixeira MM, Mackay CR (2009) Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461(7268):1282-U1119
Clayburgh DR, Shen L, Turner JR (2004) A porous defense: the leaky epithelial barrier in intestinal disease. Lab Invest 84(3):282–291
Fritsch J, Abreu M (2019) The Microbiota and the immune response: what is the chicken and what is the egg? Gastrointest Endosc Clin N Am. https://doi.org/10.1016/j.giec.2019.02.005
Hilsden RJ, Meddings JB, Hardin J, Gall DG, Sutherland LR (1999) Intestinal permeability and postheparin plasma diamine oxidase activity in the prediction of Crohn’s disease relapse. Inflamm Bowel Dis 5(2):85–91
Zeissig S, Burgel N, Gunzel D, Richter J, Mankertz J, Wahnschaffe U, Kroesen AJ, Zeitz M, Fromm M, Schulzke JD (2007) Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn’s disease. Gut 56(1):61–72. https://doi.org/10.1136/gut.2006.094375
Di Sabatino A, Ciccocioppo R, Luinetti O, Ricevuti L, Morera R, Cifone AG, Solcia E, Corazza GR (2003) Increased enterocyte apoptosis in inflamed areas of Crohn’s disease. Dis Colon Rectum 46(11):1498–1507
Coufal S, Galanova N, Bajer L, Gajdarova Z, Schierova D, Zakostelska ZJ, Kostovcikova K, Jackova Z, Stehlikova Z, Drastich P, Tlaskalova-Hogenova H, Kverka M (2019) Inflammatory bowel disease types differ in markers of inflammation, gut barrier and in specific anti-bacterial response. Cells. https://doi.org/10.3390/cells8070719
Kapsoritakis A, Kapsoritaki A, Davidi I, Lotis V, Manolakis A, Mylonis P, Theodoridou A, Germenis A, Potamianos S (2008) Imbalance of tissue inhibitors of metalloproteinases (TIMP) – 1 and – 4 serum levels, in patients with inflammatory bowel disease. BMC Gastroenterol 8:55. https://doi.org/10.1186/1471-230X-8-55
Luo XP, Yue B, Yu ZL, Ren YJ, Zhang J, Ren JY, Wang ZT, Dou W (2020) Obacunone Protects Against Ulcerative Colitis in Mice by Modulating Gut Microbiota, Attenuating TLR4/NF-kappa B Signaling Cascades, and Improving Disrupted Epithelial Barriers. Front Microbiol 11:497. https://doi.org/10.3389/fmicb.2020.00497
Sayoc-Becerra A, Krishnan M, Fan SJ, Jimenez J, Hernandez R, Gibson K, Preciado R, Butt G, McCole DF (2020) The JAK-inhibitor tofacitinib rescues human intestinal epithelial cells and colonoids from cytokine-induced barrier dysfunction. Inflamm Bowel Dis 26(3):407–422
Mankertz J, Tavalali S, Schmitz H, Mankertz A, Riecken EO, Fromm M, Schulzke JD (2000) Expression from the human occludin promoter is affected by tumor necrosis factor alpha and interferon gamma. J Cell Sci 113(11):2085–2090
Wang Y, Xie Q, Zhang Y, Ma W, Ning K, Xiang JY, Cui J, Xiang H (2020) Combination of probiotics with different functions alleviate DSS-induced colitis by regulating intestinal microbiota, IL-10, and barrier function. Appl Microbiol Biotechnol 104(1):335–349. https://doi.org/10.1007/s00253-019-10259-6
Zhang MM, Zhou Q, Dorfman RG, Huang XL, Fan TT, Zhang H, Zhang J, Yu CG (2016) Butyrate inhibits interleukin-17 and generates Tregs to ameliorate colorectal colitis in rats. BMC Gastroenterol 16:84. https://doi.org/10.1186/s12876-016-0500-x
Kelly CJ, Zheng L, Campbell EL, Saeedi B, Scholz CC, Bayless AJ, Wilson KE, Glover LE, Kominsky DJ, Magnuson A, Weir TL, Ehrentraut SF, Pickel C, Kuhn KA, Lanis JM, Nguyen V, Taylor CT, Colgan SP (2015) Crosstalk between microbiota-derived short-chain fatty acids and intestinal epithelial hif augments tissue barrier function. Cell Host Microbe 17(5):662–671
Valenzano MC, DiGuilio K, Mercado J, Teter M, To J, Ferraro B, Mixson B, Manley I, Baker V, Moore BA, Wertheimer J, Mullin JM (2015) Remodeling of tight junctions and enhancement of barrier integrity of the CACO-2 intestinal epithelial cell layer by micronutrients. Plos One 10(7):e0133926. https://doi.org/10.1371/journal.pone.0133926
Bordonaro M, Lazarova DL, Sartorelli AC (2008) Butyrate and Wnt signaling: a possible solution to the puzzle of dietary fiber and colon cancer risk? Cell Cycle 7(9):1178–1183. https://doi.org/10.4161/cc.7.9.5818
Zhao Y, Chen FD, Wu W, Sun MM, Bilotta AJ, Yao SX, Xiao Y, Huang XS, Eaves-Pyles TD, Golovko G, Fofanov Y, D’Souza W, Zhao QH, Liu ZJ, Cong YZ (2018) GPR43 mediates microbiota metabolite SCFA regulation of antimicrobial peptide expression in intestinal epithelial cells via activation of mTOR and STAT3. Mucosal Immunol 11(3):752–762
Chang PV, Hao L, Offermanns S, Medzhitov R (2014) The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc Natl Acad Sci USA 111(6):2247–2252. https://doi.org/10.1073/pnas.1322269111
Frank DN, Robertson CE, Hamm CM, Kpadeh Z, Zhang TY, Chen HY, Zhu W, Sartor RB, Boedeker EC, Harpaz N, Pace NR, Li E (2011) Disease Phenotype and Genotype Are Associated with Shifts in Intestinal-associated Microbiota in Inflammatory Bowel Diseases. Inflamm Bowel Dis 17(1):179–184
Ott SJ, Musfeldt M, Wenderoth DF, Hampe J, Brant O, Folsch UR, Timmins KN, Schreiber S (2004) Reduction in diversity of the colonic mucosa associated bacterial microflora in patients with active inflammatory bowel disease. Gut 53(5):685–693
Goncalves P, Araujo JR, Di Santo JP (2018) A cross-talk between microbiota-derived short-chain fatty acids and the host mucosal immune system regulates intestinal homeostasis and inflammatory bowel disease. Inflamm Bowel Dis 24(3):558–572
Eeckhaut V, Machiels K, Perrier C, Romero C, Maes S, Flahou B, Steppe M, Haesebrouck F, Sas B, Ducatelle R, Vermeire S, Van Immerseel F (2013) Butyricicoccus pullicaecorum in inflammatory bowel disease. Gut 62(12):1745–1752
Turroni F, Milani C, Duranti S, Mancabelli L, Mangifesta M, Viappiani A, Lugli GA, Ferrario C, Gioiosa L, Ferrarini A, Li J, Palanza P, Delledonne M, van Sinderen D, Ventura M (2016) Deciphering bifidobacterial-mediated metabolic interactions and their impact on gut microbiota by a multi-omics approach. Isme J 10(7):1656–1668
Simeoli R, Raso GM, Pirozzi C, Lama A, Santoro A, Russo R, Montero-Melendez T, Canani RB, Calignano A, Perretti M, Meli R (2017) An orally administered butyrate-releasing derivative reduces neutrophil recruitment and inflammation in dextran sulphate sodium-induced murine colitis. Brit J Pharmacol 174(11):1484–1496
Atkinson MA, Eisenbarth GS, Michels AW (2014) Type 1 diabetes. Lancet 383(9911):69–82
Gulden E, Ihira M, Ohashi A, Reinbeck AL, Freudenberg MA, Kolb H, Burkart V (2013) Toll-Like Receptor 4 Deficiency Accelerates the Development of Insulin-Deficient Diabetes in Non-Obese Diabetic Mice. Plos One 8(9):e75385. https://doi.org/10.1371/journal.pone.0075385
Simon MC, Reinbeck AL, Wessel C, Heindirk J, Jelenik T, Kaul K, Arreguin-Cano J, Strom A, Blaut M, Backhed F, Burkart V, Roden M (2020) Distinct alterations of gut morphology and microbiota characterize accelerated diabetes onset in nonobese diabetic mice. J Biol Chem 295(4):969–980
Kuitunen M, Saukkonen T, Ilonen J, Akerblom HK, Savilahti E (2002) Intestinal permeability to mannitol and lactulose in children with type 1 diabetes with the HLA-DQB1*02 allele. Autoimmunity 35(5):365–368
Sapone A, de Magistris L, Pietzak M, Clemente MG, Tripathi A, Cucca F, Lampis R, Kryszak D, Carteni M, Generoso M, Iafusco D, Prisco F, Laghi F, Riegler G, Carratu R, Counts D, Fasano A (2006) Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes 55(5):1443–1449
Secondulfo M, Iafusco D, Carratu R, deMagistris L, Sapone A, Generoso M, Mezzogiorno A, Sasso FC, Carteni M, De Rosa R, Prisco F, Esposito V (2004) Ultrastructural mucosal alterations and increased intestinal permeability in non-celiac, type I diabetic patients. Digest Liver Dis 36(1):35–45
Sorini C, Cosorich I, Lo Conte M, De Giorgi L, Facciotti F, Luciano R, Rocchi M, Ferrarese R, Sanvito F, Canducci F, Falcone M (2019) Loss of gut barrier integrity triggers activation of islet-reactive T cells and autoimmune diabetes. Proc Natl Acad Sci USA 116(30):15140–15149. https://doi.org/10.1073/pnas.1814558116
Coombes JL, Powrie F (2008) Dendritic cells in intestinal immune regulation. Nat Rev Immunol 8(6):435–446
Chen K, Chen H, Faas MM, de Haan BJ, Li JH, Xiao P, Zhang H, Diana J, de Vos P, Sun J (2017) Specific inulin-type fructan fibers protect against autoimmune diabetes by modulating gut immunity, barrier function, and microbiota homeostasis. Mol Nutr Food Res 61(8):1601006. https://doi.org/10.1002/mnfr.201601006
Hansen CHF, Larsen CS, Petersson HO, Zachariassen LF, Vegge A, Lauridsen C, Kot W, Krych L, Nielsen DS, Hansen AK (2019) Targeting gut microbiota and barrier function with prebiotics to alleviate autoimmune manifestations in NOD mice. Diabetologia 62(9):1689–1700. https://doi.org/10.1007/s00125-019-4910-5
Wen L, Ley RE, Volchkov PY, Stranges PB, Avanesyan L, Stonebraker AC, Hu CY, Wong FS, Szot GL, Bluestone JA, Gordon JI, Chervonsky AV (2008) Innate immunity and intestinal microbiota in the development of Type 1 diabetes. Nature 455(7216):1109-U1110
Harbison JE, Roth-Schulze AJ, Giles LC, Tran CD, Ngui KM, Penno MA, Thomson RL, Wentworth JM, Colman PG, Craig ME, Morahan G, Papenfuss AT, Barry SC, Harrison LC, Couper JJ (2019) Gut microbiome dysbiosis and increased intestinal permeability in children with islet autoimmunity and type 1 diabetes: A prospective cohort study. Pediatric Diabetes 20(5):574–583. https://doi.org/10.1111/pedi.12865
Vatanen T, Franzosa EA, Schwager R, Tripathi S, Arthur TD, Vehik K, Lernmark A, Hagopian WA, Rewers MJ, She JX, Toppari J, Ziegler AG, Akolkar B, Krischer JP, Stewart CJ, Ajami NJ, Petrosino JF, Gevers D, Lahdesmaki H, Vlamakis H, Huttenhower C, Xavier RJ (2018) The human gut microbiome in early-onset type 1 diabetes from the TEDDY study. Nature 562(7728):589–594. https://doi.org/10.1038/s41586-018-0620-2
Wood NJ (2012) Microbiota: Dysbiosis driven by inflammasome deficiency exacerbates hepatic steatosis and governs rate of NAFLD progression. Nature Rev Gastroenterol Hepatol 9(3):123. https://doi.org/10.1038/nrgastro.2012.21
Miura K, Ohnishi H (2014) Role of gut microbiota and Toll-like receptors in nonalcoholic fatty liver disease. World J Gastroenterol 20(23):7381–7391. https://doi.org/10.3748/wjg.v20.i23.7381
Mouries J, Brescia P, Silvestri A, Spadoni I, Sorribas M, Wiest R, Mileti E, Galbiati M, Invernizzi P, Adorini L, Penna G, Rescigno M (2019) Microbiota-driven gut vascular barrier disruption is a prerequisite for non-alcoholic steatohepatitis development. J Hepatol 71(6):1216–1228. https://doi.org/10.1016/j.jhep.2019.08.005
Wang B, Jiang X, Cao M, Ge J, Bao Q, Tang L, Chen Y, Li L (2016) Altered fecal microbiota correlates with liver biochemistry in nonobese patients with non-alcoholic fatty liver disease. Sci Rep 6:32002. https://doi.org/10.1038/srep32002
Ning LG, Liu RQ, Lou XH, Du HJ, Chen WG, Zhang FM, Li S, Chen XY, Xu GQ (2019) Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: a systemic review and meta-analysis. Eur J Gastroen Hepat 31(7):735–742
Natividad JM, Lamas B, Pham HP, Michel ML, Rainteau D, Bridonneau C, da Costa G, Vlieg JV, Sovran B, Chamignon C, Planchais J, Richard ML, Langella P, Veiga P, Sokol H (2018) Bilophila wadsworthia aggravates high fat diet induced metabolic dysfunctions in mice. Nature Commun 9:2802. https://doi.org/10.1038/s41467-018-05249-7
Rahman K, Desai C, Iyer SS, Thorn NE, Kumar P, Liu Y, Smith T, Neish AS, Li H, Tan S, Wu P, Liu X, Yu Y, Farris AB, Nusrat A, Parkos CA, Anania FA (2016) Loss of Junctional Adhesion Molecule A Promotes Severe Steatohepatitis in Mice on a Diet High in Saturated Fat, Fructose, and Cholesterol. Gastroenterology 151(4):733-746 e712. https://doi.org/10.1053/j.gastro.2016.06.022
Hundertmark J, Krenkel O, Tacke F (2018) Adapted immune responses of myeloid-derived cells in fatty liver disease. Front Immunol 9:2418. https://doi.org/10.3389/fimmu.2018.02418
Pleguezuelo M, Benitez JM, Jurado J, Montero JL, De la Mata M (2013) Diagnosis and management of bacterial infections in decompensated cirrhosis. World J Hepatol 5(1):16–25. https://doi.org/10.4254/wjh.v5.i1.16
Li Y, Liu T, Yan C, Xie R, Guo Z, Wang S, Zhang Y, Li Z, Wang B, Cao H (2018) Diammonium glycyrrhizinate protects against nonalcoholic fatty liver disease in mice through modulation of gut microbiota and restoration of intestinal barrier. Mol Pharm 15(9):3860–3870. https://doi.org/10.1021/acs.molpharmaceut.8b00347
Jin M, Zhu Y, Shao D, Zhao K, Xu C, Li Q, Yang H, Huang Q, Shi J (2017) Effects of polysaccharide from mycelia of Ganoderma lucidum on intestinal barrier functions of rats. Int J Biol Macromol 94(Pt A):1–9. https://doi.org/10.1016/j.ijbiomac.2016.09.099
Ye JZ, Lv LX, Wu WR, Li YT, Shi D, Fang DQ, Guo FF, Jiang HY, Yan R, Ye WC, Li LJ (2018) Butyrate protects mice against methionine-choline-deficient diet-induced non-alcoholic steatohepatitis by improving gut barrier function, attenuating inflammation and reducing endotoxin levels. Front Microbiol 9:1967. https://doi.org/10.3389/fmicb.2018.01967
Song JJ, Tian WJ, Kwok LY, Wang YL, Shang YN, Menghe B, Wang JG (2017) Effects of microencapsulated Lactobacillus plantarum LIP-1 on the gut microbiota of hyperlipidaemic rats. Br J Nutr 118(7):481–492. https://doi.org/10.1017/S0007114517002380
Patterson AM, Mulder IE, Travis AJ, Lan A, Cerf-Bensussan N, Gaboriau-Routhiau V, Garden K, Logan E, Delday MI, Coutts AGP, Monnais E, Ferraria VC, Inoue R, Grant G, Aminov RI (2017) Human gut symbiont roseburia hominis promotes and regulates innate immunity. Front Immunol 8:1166. https://doi.org/10.3389/fimmu.2017.01166
Wang JH, Bose S, Lim SK, Ansari A, Chin YW, Choi HS, Kim H (2017) Houttuynia cordata facilitates metformin on ameliorating insulin resistance associated with gut microbiota alteration in OLETF rats. Genes-Basel 8(10):239. https://doi.org/10.3390/genes8100239
Jin CJ, Sellmann C, Engstler J, Ziegenhardt D, Bergheim I (2015) Supplementation of sodium butyrate protects mice from the development of non-alcoholic steatohepatitis (NASH). British J Nutr 114:1–11. https://doi.org/10.1017/S0007114515003621
Song M, Xia B, Li J (2006) Effects of topical treatment of sodium butyrate and 5-aminosalicylic acid on expression of trefoil factor 3, interleukin 1beta, and nuclear factor kappaB in trinitrobenzene sulphonic acid induced colitis in rats. Postgrad Med J 82(964):130–135. https://doi.org/10.1136/pgmj.2005.037945
Diao H, Jiao AR, Yu B, Mao XB, Chen DW (2019) Gastric infusion of short-chain fatty acids can improve intestinal barrier function in weaned piglets. Genes Nutr 14:4. https://doi.org/10.1186/s12263-019-0626-x
Xu YH, Gao CL, Guo HL, Zhang WQ, Huang W, Tang SS, Gan WJ, Xu Y, Zhou H, Zhu Q (2018) Sodium butyrate supplementation ameliorates diabetic inflammation in db/db mice. J Endocrinol 238(3):231–244. https://doi.org/10.1530/JOE-18-0137
Lin J, Peng L, Itzkowitz S, Holzman IR, Babyatsky MW (2005) Short-chain fatty acid induces intestinal mucosal injury in newborn rats and down-regulates intestinal trefoil factor gene expression in vivo and in vitro. J Pediatr Gastroenterol Nutr 41(5):607–611. https://doi.org/10.1097/01.mpg.0000179659.09210.ff
Bentley-Hewitt KL, Blatchford PA, Parkar SG, Ansell J, Pernthaner A (2012) Digested and fermented green kiwifruit increases human beta-defensin 1 and 2 production in vitro. Plant Food Hum Nutr 67(3):208–214
Zheng L, Kelly CJ, Battista KD, Schaefer R, Lanis JM, Alexeev EE, Wang RX, Onyiah JC, Kominsky DJ, Colgan SP (2017) Microbial-derived butyrate promotes epithelial barrier function through IL-10 receptor-dependent repression of claudin-2. J Immunol 199(8):2976–2984. https://doi.org/10.4049/jimmunol.1700105
Qin SM, Zhang KY, Ding XM, Bai SP, Wang JP, Zeng QF (2019) Effect of dietary graded resistant potato starch levels on growth performance, plasma cytokines concentration, and intestinal health in meat ducks. Poult Sci 98(9):3523–3532. https://doi.org/10.3382/ps/pez186
Maurer LH, Cazarin CBB, Quatrin A, Minuzzi NM, Costa EL, Morari J, Velloso LA, Leal RF, Rodrigues E, Bochi VC, Marstica MR, Emanuelli T (2019) Grape peel powder promotes intestinal barrier homeostasis in acute TNBS-colitis: A major role for dietary fiber and fiber-bound polyphenols. Food Res Int 123:425–439
Fei Y, Wang Y, Pang Y, Wang W, Zhu D, Xie M, Lan S, Wang Z (2019) Xylooligosaccharide modulates gut microbiota and alleviates colonic inflammation caused by high fat diet induced obesity. Front Physiol 10:1601. https://doi.org/10.3389/fphys.2019.01601
Perdijk O, van Baarlen P, Fernandez-Gutierrez MM, van den Brink E, Schuren FHJ, Brugman S, Savelkoul HFJ, Kleerebezem M, van Neerven RJJ (2019) Sialyllactose and galactooligosaccharides promote epithelial barrier functioning and distinctly modulate microbiota composition and short chain fatty acid production in vitro. Front Immunol 10:94. https://doi.org/10.3389/fimmu.2019.00094
Acknowledgements
I would like to thank my collaborators for their support and help.
Funding
This research was supported by Key Project of Natural Science Foundation of Zhejiang Province (Grant No. D19C200001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, W., Luo, X., Tang, J. et al. A bridge for short-chain fatty acids to affect inflammatory bowel disease, type 1 diabetes, and non-alcoholic fatty liver disease positively: by changing gut barrier. Eur J Nutr 60, 2317–2330 (2021). https://doi.org/10.1007/s00394-020-02431-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02431-w