Abstract
Purpose
Populations malnourished in early life are at increased risk for cardiometabolic diseases. We assessed if improved nutrition predicts cardiometabolic function, as assessed by postprandial biomarker responses.
Methods
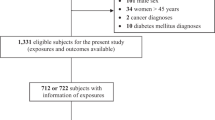
Participants had been randomized at the village level to receive one of two nutritional supplements as children. At mean age 44 y (range 37–53 years), we obtained plasma samples before and 2 h after a mixed-component meal challenge. We assayed biomarkers including lipids, glycemic measurements, and inflammatory cytokines. We compared postprandial biomarker responses among those who received the improved nutrition intervention from conception through to their second birthday (the first 1000 days) to those with other exposure status, including those who received the improved nutrition intervention at other ages, and those who received the less nutritious supplement.
Results
Among 1027 participants (59.4% female), 22.9% were exposed to improved nutrition in the first 1000 days. Insulin increased the most in response to the meal challenge (over twofold), and non-esterified fatty acids decreased the most (by half). Glucose increased postprandial by 11.4% in the exposed group, compared with 15.7% in the other exposure group (p < 0.05), which remained significant after adjusting for confounders (− 4.7%; 95% confidence interval: − 9.3%, − 0.01%). Responses to the prandial challenges for the other biomarkers did not differ by intervention group (all p > 0.05).
Conclusion
Early life exposure to improved nutrition was associated with a more favorable postprandial glucose response in this population. We did not observe a difference in overall cardiometabolic responses between the exposure groups.


Similar content being viewed by others
Data availability
Data described in the manuscript will be made available upon request, pending approval by the principal investigator.
Code availability
Statistical codes used to produce the results in the manuscript will be made available upon request, pending approval by the principal investigator.
References
Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, Sachdev HS, Maternal, Child Undernutrition Study G (2008) Maternal and child undernutrition: consequences for adult health and human capital. Lancet 371(9609):340–357. https://doi.org/10.1016/S0140-6736(07)61692-4
Martorell R (2017) Improved nutrition in the first 1000 days and adult human capital and health. Am J Hum Biol. https://doi.org/10.1002/ajhb.22952
Adair LS (2014) Long-term consequences of nutrition and growth in early childhood and possible preventive interventions. Nestle Nutr Inst Workshop Ser 78:111–120. https://doi.org/10.1159/000354949
Barker DJ, Osmond C (1986) Infant mortality, childhood nutrition, and ischaemic heart disease in England and Wales. Lancet 1(8489):1077–1081. https://doi.org/10.1016/s0140-6736(86)91340-1
Suzuki K (2018) The developing world of DOHaD. J Dev Orig Health Dis 9(3):266–269. https://doi.org/10.1017/s2040174417000691
Popkin BM, Adair LS, Ng SW (2012) Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 70(1):3–21. https://doi.org/10.1111/j.1753-4887.2011.00456.x
Popkin BM (2015) Nutrition transition and the global diabetes epidemic. Curr Diab Rep 15(9):64. https://doi.org/10.1007/s11892-015-0631-4
Popkin BM (1998) The nutrition transition and its health implications in lower-income countries. Public Health Nutr 1(1):5–21
Institute for Health Metrics and Evaluation (IHME) (2018) Findings from the global burden of disease study. IHME, Seattle
Ndisang JF, Rastogi S (2013) Cardiometabolic diseases and related complications: current status and future perspective. Biomed Res Int 2013:467682. https://doi.org/10.1155/2013/467682
Klop B, Proctor SD, Mamo JC, Botham KM, Castro Cabezas M (2012) Understanding postprandial inflammation and its relationship to lifestyle behaviour and metabolic diseases. Int J Vasc Med 2012:947417. https://doi.org/10.1155/2012/947417
Ceriello A, Genovese S (2016) Atherogenicity of postprandial hyperglycemia and lipotoxicity. Rev Endocr Metab Disord 17(1):111–116. https://doi.org/10.1007/s11154-016-9341-8
Ceriello A, Taboga C, Tonutti L, Quagliaro L, Piconi L, Bais B, Da Ros R, Motz E (2002) Evidence for an independent and cumulative effect of postprandial hypertriglyceridemia and hyperglycemia on endothelial dysfunction and oxidative stress generation: effects of short- and long-term simvastatin treatment. Circulation 106(10):1211–1218
de Vries MA, Klop B, Janssen HW, Njo TL, Westerman EM, Castro Cabezas M (2014) Postprandial inflammation: targeting glucose and lipids. Adv Exp Med Biol 824:161–170. https://doi.org/10.1007/978-3-319-07320-0_12
Miranda JJ, Barrientos-Gutierrez T, Corvalan C, Hyder AA, Lazo-Porras M, Oni T, Wells JCK (2019) Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med 25(11):1667–1679. https://doi.org/10.1038/s41591-019-0644-7
van Ommen B, van der Greef J, Ordovas JM, Daniel H (2014) Phenotypic flexibility as key factor in the human nutrition and health relationship. Genes Nutr 9(5):423. https://doi.org/10.1007/s12263-014-0423-5
Castro JP, El-Atat FA, McFarlane SI, Aneja A, Sowers JR (2003) Cardiometabolic syndrome: pathophysiology and treatment. Curr Hypertens Rep 5(5):393–401. https://doi.org/10.1007/s11906-003-0085-y
van Ommen B, Keijer J, Heil SG, Kaput J (2009) Challenging homeostasis to define biomarkers for nutrition related health. Mol Nutr Food Res 53(7):795–804. https://doi.org/10.1002/mnfr.200800390
Calder PC, Ahluwalia N, Albers R, Bosco N, Bourdet-Sicard R, Haller D, Holgate ST, Jonsson LS, Latulippe ME, Marcos A, Moreines J, M'Rini C, Muller M, Pawelec G, van Neerven RJ, Watzl B, Zhao J (2013) A consideration of biomarkers to be used for evaluation of inflammation in human nutritional studies. Br J Nutr 109(Suppl 1):S1–34. https://doi.org/10.1017/S0007114512005119
Popkin BM, Corvalan C, Grummer-Strawn LM (2020) Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395(10217):65–74. https://doi.org/10.1016/S0140-6736(19)32497-3
Conlisk AJ, Barnhart HX, Martorell R, Grajeda R, Stein AD (2004) Maternal and child nutritional supplementation are inversely associated with fasting plasma glucose concentration in young Guatemalan adults. J Nutr 134(4):890–897
Stein AD, Wang M, Ramirez-Zea M, Flores R, Grajeda R, Melgar P, Ramakrishnan U, Martorell R (2006) Exposure to a nutrition supplementation intervention in early childhood and risk factors for cardiovascular disease in adulthood: evidence from Guatemala. Am J Epidemiol 164(12):1160–1170. https://doi.org/10.1093/aje/kwj328
Ford ND, Behrman JR, Hoddinott JF, Maluccio JA, Martorell R, Ramirez-Zea M, Stein AD (2018) Exposure to improved nutrition from conception to age 2 years and adult cardiometabolic disease risk: a modelling study. Lancet Glob Health 6(8):e875–e884. https://doi.org/10.1016/S2214-109X(18)30231-6
He S, Le NA, Ramirez-Zea M, Martorell R, Narayan KMV, Stein AD (2020) Leptin partially mediates the association between early-life nutritional supplementation and long-term glycemic status among women in a Guatemalan longitudinal cohort. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqaa001
Martorell R, Habicht JP, Rivera JA (1041S) History and design of the INCAP longitudinal study (1969–77) and its follow-up (1988–89). J Nutr 125(4 Suppl):1027S–1041S
Stein AD, Melgar P, Hoddinott J, Martorell R (2008) Cohort profile: the Institute of Nutrition of Central America and Panama (INCAP) Nutrition Trial Cohort Study. Int J Epidemiol 37(4):716–720. https://doi.org/10.1093/ije/dyn028
Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 7(4):284–294
National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A (2002) Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
American Diabetes Association (2018) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care 41(Suppl 1):S13–s27. https://doi.org/10.2337/dc18-S002
Venables WN, Ripley BD (2002) Modern applied statistics with S. Fourth edition. Springer, Berlin
Lopez-Lopez J, Lopez-Jaramillo P, Camacho PA, Gomez-Arbelaez D, Cohen DD (2015) The link between fetal programming, inflammation, muscular strength, and blood pressure. Mediat Inflamm. https://doi.org/10.1155/2015/710613
Yan X, Zhu MJ, Dodson MV, Du M (2013) Developmental programming of fetal skeletal muscle and adipose tissue development. J Genom 1:29–38. https://doi.org/10.7150/jgen.3930
Symonds ME, Pope M, Sharkey D, Budge H (2012) Adipose tissue and fetal programming. Diabetologia 55(6):1597–1606. https://doi.org/10.1007/s00125-012-2505-5
Waterland RA, Garza C (2002) Early postnatal nutrition determines adult pancreatic glucose-responsive insulin secretion and islet gene expression in rats. J Nutr 132(3):357–364. https://doi.org/10.1093/jn/132.3.357
Holness MJ, Langdown ML, Sugden MC (2000) Early-life programming of susceptibility to dysregulation of glucose metabolism and the development of Type 2 diabetes mellitus. Biochem J 349(Pt 3):657–665. https://doi.org/10.1042/bj3490657
Martorell R (1138S) Results and implications of the INCAP follow-up study. J Nutr 125(4 Suppl):1127S–1138S
Gruszfeld D, Weber M, Gradowska K, Socha P, Grote V, Xhonneux A, Dain E, Verduci E, Riva E, Closa-Monasterolo R, Escribano J, Koletzko B (2016) Association of early protein intake and pre-peritoneal fat at five years of age: follow-up of a randomized clinical trial. Nutr Metab Cardiovasc Dis 26(9):824–832. https://doi.org/10.1016/j.numecd.2016.04.005
Wilcox G (2005) Insulin and insulin resistance. Clin Biochem Rev 26(2):19–39
Meek TH, Morton GJ (2016) The role of leptin in diabetes: metabolic effects. Diabetologia 59(5):928–932. https://doi.org/10.1007/s00125-016-3898-3
Scarlett JM, Schwartz MW (2015) Gut-brain mechanisms controlling glucose homeostasis. F1000Prime Rep 7:12. https://doi.org/10.12703/p7-12
Roche HM, Gibney MJ (1995) Postprandial triacylglycerolaemia–nutritional implications. Prog Lipid Res 34(3):249–266
Langsted A, Freiberg JJ, Nordestgaard BG (2008) Fasting and nonfasting lipid levels: influence of normal food intake on lipids, lipoproteins, apolipoproteins, and cardiovascular risk prediction. Circulation 118(20):2047–2056. https://doi.org/10.1161/CIRCULATIONAHA.108.804146
O’Keefe JH, Bell DS (2007) Postprandial hyperglycemia/hyperlipidemia (postprandial dysmetabolism) is a cardiovascular risk factor. Am J Cardiol 100(5):899–904
Miles JM, Isley WL, Harris WS (2005) Postprandial free fatty acid metabolism in normal, dyslipidemic and type 2 diabetic subjects: a relationship to hepatic triglyceride metabolism? J Investig Med 53(1):S106–S106. https://doi.org/10.2310/6650.2005.00005.162
Kwon H, Pessin JE (2013) Adipokines mediate inflammation and insulin resistance. Front Endocrinol (Lausanne) 4:71. https://doi.org/10.3389/fendo.2013.00071
Lopez-Jaramillo P, Gomez-Arbelaez D, Lopez-Lopez J, Lopez-Lopez C, Martinez-Ortega J, Gomez-Rodriguez A, Triana-Cubillos S (2014) The role of leptin/adiponectin ratio in metabolic syndrome and diabetes. Horm Mol Biol Clin Investig 18(1):37–45. https://doi.org/10.1515/hmbci-2013-0053
Lew J, Sanghavi M, Ayers CR, McGuire DK, Omland T, Atzler D, Gore MO, Neeland I, Berry JD, Khera A, Rohatgi A, de Lemos JA (2017) Sex-based differences in cardiometabolic biomarkers. Circulation 135(6):544–555. https://doi.org/10.1161/circulationaha.116.023005
Chen GC, Qin LQ, Ye JK (2014) Leptin levels and risk of type 2 diabetes: gender-specific meta-analysis. Obes Rev 15(2):134–142. https://doi.org/10.1111/obr.12088
Kautzky-Willer A, Handisurya A (2009) Metabolic diseases and associated complications: sex and gender matter! Eur J Clin Invest 39(8):631–648
Lee BM, Wolver TM (1998) Effect of glucose, sucrose and fructose on plasma glucose and insulin responses in normal humans: comparison with white bread. Enr J Clin Nutr 52(12):924–928
Besser REJ, Shields BM, Casas R, Hattersley AT, Ludvigsson J (2013) Lessons from the Mixed-Meal Tolerance Test. Diabetes Care 36:195–201
Van Dijk S, Mensink M, Esser D, Feskens EJM, Müller M, Afman LA (2012) Response to high-fat challenges varying in fat type in subjects with different metabolic risk phenotypes: a randomized trial. PLoS ONE 7(7):e41388
Westphal S, Leodolter A, Kahl S, Dierkes J, Malfertheiner P, Luley C (2002) Addition of glucose to a fatty meal delays chylomicrons and suppresses VLDL in healthy subjects. Eur J Clin Invest 32(5):322–327. https://doi.org/10.1046/j.1365-2362.2002.00978.x
Martorell R, Melgar P, Maluccio JA, Stein AD, Rivera JA (2010) The nutrition intervention improved adult human capital and economic productivity. J Nutr 140(2):411–414. https://doi.org/10.3945/jn.109.114504
Kemper H, Post G, Twisk J, Van Mechelen W (1999) Lifestyle and obesity in adolescence and young adulthood: results from the Amsterdam Growth And Health Longitudinal Study (AGAHLS). Int J Obes Relat Metab Disord 23(3):S34–S40
McLaren L (2007) Socioeconomic status and obesity. Epidemiol Rev 29(1):29–48. https://doi.org/10.1093/epirev/mxm001
Acknowledgements
The authors would like to thank the INCAP colleagues, field team, and our study participants in Guatemala.
Funding
This work was supported by the National Institutes of Health (Grant No. HD075784).
Author information
Authors and Affiliations
Contributions
SH collected laboratory data, conducted statistical analysis, interpreted the data, wrote the paper, and have primary responsibility of final content. NAL designed biomarker data collection procedures and provided essential materials for laboratory data collection. NAL, MRZ, RM, and KMVK contributed to the interpretation of data, writing, and reviewing of the manuscript. ADS designed the research and guided the overall data analysis, interpretation, and writing of the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
SH, NAL, MRZ, RM, KMVN, and ADS declare that there are no conflicts of interest.
Ethical approval
The study was approved by the Institutional Review Board at Emory University and the Ethics Review Committee of INCAP.
Informed consent
All study participants provided written informed consent in Spanish.
Consent for publication
The publication of this manuscript has been approved by all co-authors, as well as by the responsible authorities at the institute where the work has been carried out.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, S., Le, NA., Ramìrez-Zea, M. et al. Postprandial glycemic response differed by early life nutritional exposure in a longitudinal cohort: a single- and multi-biomarker approach. Eur J Nutr 60, 1973–1984 (2021). https://doi.org/10.1007/s00394-020-02389-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02389-9