Abstract
Purpose
There is strong scientific evidence for reducing sodium and increasing potassium intake to the recommended levels to lower blood pressure and cardiovascular risk, but consumption levels in Kazakhstan are unknown. This study sought to estimate mean sodium and potassium intake using 24-h urine samples and describe dietary knowledge and behavior among adults in Kazakhstan.
Methods
In two cross-sectional surveys, the same multi-stage cluster sampling method was used to randomly select participants aged 25–64 years from Almaty City in 2015 and Kyzylorda in 2016. Complete 24-h urine samples were available for 478 participants; 294 in Almaty City and 184 in Kyzylorda (response rates 86% and 54%, respectively) and were weighted for the age and sex distribution of the two regions.
Results
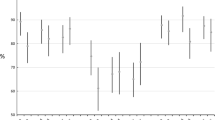
Weighted mean 24-h urinary sodium excretion was 6782 mg/day (17.2 g salt) (95% CI 6507–7058) in both regions combined, and not significantly different between the regions (P = 0.660). 99% of adults in the two regions combined consumed above the World Health Organization’s (WHO) recommended sodium maximum of 2000 mg/day; however, only 15% of adults perceived that they consumed excess sodium. Weighted mean 24-h urinary potassium excretion was 2271 mg/day (95% CI 2151–2391) for the regions combined.
Conclusion
Mean sodium consumption in Kazakhstan was more than triple the WHO’s recommended maximum, and mean potassium consumption was below the recommended minimum. National efforts to lower sodium intake and increase potassium intake are needed and would likely prevent ample premature deaths and disease burden.



Similar content being viewed by others
References
Institute for Health Metrics and Evaluation (2017) GBD compare. IHME, University of Washington. http://vizhub.healthdata.org/gbd-compare. Accessed 3 Nov 2017
World Health Organization (2018) Noncommunicable disease country profiles 2018- Kazakhstan. World Health Organization. http://www.who.int/nmh/countries/2018/kaz_en.pdf. Accessed 21 Nov 2018
He FJ, Li J, Macgregor GA (2013) Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. BMJ 346:f1325
Newberry SJ, Chung M, Anderson CAM, Chen C, Fu Z, Tang A, Zhao N, Booth M, Marks J, Hollands S, Motala A, Larkin JK, Shanman R, Hempel S (2018) Sodium and potassium intake: effects on chronic disease outcomes and risks. Comparative Effectiveness Review No. 206. Agency for Healthcare Research and Quality. https://effectivehealthcare.ahrq.gov/topics/sodium-potassium/final-report-2018. Accessed 1 Sept 2018
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ (2013) Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 346:f1326. https://doi.org/10.1136/bmj.f1326
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP (2013) Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 346:f1378. https://doi.org/10.1136/bmj.f1378
Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, Li Q, Lackland DT, Leung AA, Anderson CAM, MacGregor GA, He FJ (2020) Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ 368:m315. https://doi.org/10.1136/bmj.m315%JBMJ
World Health Organization (2012) Guideline: sodium intake for adults and children. World Health Organization. http://apps.who.int/iris/bitstream/10665/77985/1/9789241504836_eng.pdf?ua=1&ua=1. Accessed 8 Aug 2016
World Health Organization (2012) Potassium intake for adults and children—guideline. World Health Organization. http://apps.who.int/iris/bitstream/10665/77986/1/9789241504829_eng.pdf?ua=1. Accessed 16 Feb 2018
Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J (2006) Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 114(1):82–96. https://doi.org/10.1161/CIRCULATIONAHA.106.176158
World Health Organization (2013) NCD global monitoring framework. World Health Organization,. http://www.who.int/nmh/global_monitoring_framework/en/. Accessed 16 Nov 2015
Intersalt Cooperative Research Group (1988) Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24-hour urinary sodium and potassium excretion. BMJ 297(6644):319–328
Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, Zhao L, Chan Q, Elliott P (2003) Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens 17(9):623–630. https://doi.org/10.1038/sj.jhh.1001605
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D (2013) Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 3(12):e003733. https://doi.org/10.1136/bmjopen-2013-003733
Jiang J, Zhang B, Zhang M, Xue F, Tang Y, Liang S, Hou L, Wang W, Han W, Asaiti K, Nasca PC, Wang Y, Pang H, Wang Z, Wang Y, Qiu C (2015) Prevalence of conventional cardiovascular disease risk factors among Chinese Kazakh individuals of diverse occupational backgrounds in Xinjiang China. Int J Cardiol 179:558–560. https://doi.org/10.1016/j.ijcard.2014.10.077
Han W, Hu Y, Tang Y, Xue F, Hou L, Liang S, Zhang B, Wang W, Asaiti K, Pang H, Wang Z, Wang Y, Zhang M, Jiang J (2017) Relationship between urinary sodium with blood pressure and hypertension among a Kazakh community population in Xinjiang, China. J Hum Hypertens 31(5):333–340. https://doi.org/10.1038/jhh.2016.83
Liu L, Liu L, Ding Y, Huang Z, He B, Sun S, Zhao G, Zhang H, Miki T, Mizushima S, Ikeda K, Nara Y, Yamori Y (2001) Ethnic and environmental differences in various markers of dietary intake and blood pressure among Chinese Han and three other minority peoples of China: results from the WHO Cardiovascular Diseases and Alimentary Comparison (CARDIAC) Study. Hypertens Res 24(3):315–322
The World Health Organization (2014) STEPwise approach to surveillance (STEPS). The World Health Organization. http://www.who.int/chp/steps/en/. Accessed 23 Sept 2014
World Health Organization (2011) Strategies to monitor and evaluate population sodium consumption and sources of sodium in the diet- report of a joint technical meeting. World Health Organization. http://whqlibdoc.who.int/publications/2011/9789241501699_eng.pdf. Accessed 30 Oct 2014
McLean RM (2014) Measuring population sodium intake: a review of methods. Nutrients 6(11):4651–4662
WHO/PAHO Regional Expert Group for Cardiovascular Disease Prevention through Population-wide Dietary Salt Reduction (2013) Protocol for population level sodium determination in 24-hour urine samples. The World Health Organization and Pan American Health Organization. https://www.paho.org/hq/dmdocuments/2013/24h-urine-Protocol-eng.pdf. Accessed 14 Aug 2017
John KA, Cogswell ME, Campbell NR, Nowson CA, Legetic B, Hennis AJ, Patel SM (2016) Accuracy and usefulness of select methods for assessing complete collection of 24-Hour Urine: A Systematic Review. J Clin Hypertens (Greenwich) 18(5):456–467. https://doi.org/10.1111/jch.12763
Elliott P, Brown I (2007) Sodium intakes around the world—background document prepared for the Forum and Technical meeting on Reducing Salt Intake in Populations. World Health Organization, Geneva
Joossens JV GJ (1984) Monitoring salt intake of the population: methodological considerations. In: de Backer HvGG PH, Ducimetière P (eds) Surveillance of the dietary habits of the population with regard to cardiovascular diseases. EURO Nut Report 2. pp 61–73. https://doi.org/10.1002/food.19840281012
Hu Y, Wang Z, Wang Y, Wang L, Han W, Tang Y, Xue F, Hou L, Liang S, Zhang B, Wang W, Asaiti K, Pang H, Zhang M, Jiang J (2017) Prevalence, awareness, treatment, and control of hypertension among Kazakhs with high salt intake in Xinjiang, China: a community-based cross-sectional study. Sci Rep 7:45547. https://doi.org/10.1038/srep45547
WHO Regional office for Europe (2019) FEEDcities project—the food environment in cities in eastern Europe and Central Asia—Kazakhstan. World Health Organization. http://www.euro.who.int/__data/assets/pdf_file/0006/396591/WHO-FEED-Kazakhstan-report_v6.pdf?ua=1. Accessed 22 Mar 2019
Ministry of National Economy of the Republic of Kazakhstan Committee on Statistics (2019) Standard of living of population. Ministry of National Economy of the Republic of Kazakhstan. http://stat.gov.kz/faces/wcnav_externalId/homeNumbersLivingStandart;jsessionid = xSvXJ_3Q9i56UgBx8n_P3XX7v-wtA9jqQxeGQjrWRqfy2GP_oeD9!1297609147!313338418?_adf.ctrl-state=7aj9u7q3j_4&_afrLoop=5319340933202703#%40%3F_afrLoop%3D5319340933202703%26_adf.ctrl-state%3Dbkw4bm0r5_4. Accessed 1 Apr 2018
Brown IJ, Tzoulaki I, Candeias V, Elliott P (2009) Salt intakes around the world: implications for public health. Int J Epidemiol 38(3):791–813. https://doi.org/10.1093/ije/dyp139
Johnson C, Mohan S, Rogers K, Shivashankar R, Thout SR, Gupta P, He FJ, MacGregor GA, Webster J, Krishnan A, Maulik PK, Reddy KS, Prabhakaran D, Neal B (2017) Mean dietary salt intake in urban and rural areas in India: a population survey of 1395 persons. J Am Heart Assoc 6(1):e004547. https://doi.org/10.1161/JAHA.116.004547
McLean R, Edmonds J, Williams S, Mann J, Skeaff S (2015) Balancing sodium and potassium: estimates of intake in a New Zealand adult population sample. Nutrients 7(11):8930–8938. https://doi.org/10.3390/nu7115439
Cogswell ME, Loria CM, Terry AL, Zhao L, Wang CY, Chen TC, Wright JD, Pfeiffer CM, Merritt R, Moy CS, Appel LJ (2018) Estimated 24-hour urinary sodium and potassium excretion in US adults. JAMA 319(12):1209–1220. https://doi.org/10.1001/jama.2018.1156
Na Tasevska, Runswick SA, Bingham SA (2006) Urinary potassium is as reliable as urinary nitrogen for use as a recovery biomarker in dietary studies of free living individuals. J Nutr 136(5):1334–1340. https://doi.org/10.1093/jn/136.5.1334%
Stamler J, Elliott P, Chan Q (2003) INTERMAP appendix tables, tables of contents (tables A). J Hum Hypertens 17(9):665
Hall JN, Moore S, Harper SB, Lynch JW (2009) Global variability in fruit and vegetable consumption. Am J Prev Med 36(5):402.e405–409.e405. https://doi.org/10.1016/j.amepre.2009.01.029
Perez V, Chang ET (2014) Sodium-to-potassium ratio and blood pressure, hypertension, and related factors. Adv Nutr 5(6):712–741. https://doi.org/10.3945/an.114.006783
van Mierlo LA, Greyling A, Zock PL, Kok FJ, Geleijnse JM (2010) Suboptimal potassium intake and potential impact on population blood pressure. Arch Intern Med 170(16):1501–1502. https://doi.org/10.1001/archinternmed.2010.284
Webb M, Fahimi S, Singh GM, Khatibzadeh S, Micha R, Powles J, Mozaffarian D (2017) Cost effectiveness of a government supported policy strategy to decrease sodium intake: global analysis across 183 nations. BMJ. https://doi.org/10.1136/bmj.i6699
Acknowledgements
The authors wish to thank Oksana Dolmatova, Arailym Beisbekova and Marzhan Adlet for participation in for data collection and field work, and the participants for their support and interest in partaking in the survey.
Funding
KT is supported by an Early Career Fellowship (APP1161597) from the National Health and Medical Research Council of Australia (NHMRC) and a Postdoctoral Fellowship (Award ID 102140) from the National Heart Foundation of Australia. FO and ST were supported by Kazakh Academy of Nutrition from the grant of the Ministry of Education and Science, Republic of Kazakhstan. JAS is supported by the NHMRC Postgraduate Scholarship (#1168948). JW is supported by a National Heart Foundation Future Leaders Fellowship (#102039). KT, JAS and JW are part of the NHMRC Center for Research Excellence on food policy interventions to reduce salt (#1117300).
Author information
Authors and Affiliations
Contributions
FO and ST designed and conducted the research; JJ and JB provided essential materials; KT and JAS analysed the data, KT and JW wrote the paper; KT had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
JW is Director of the WHO Collaborating Centre on Population Salt Reduction. The co-authors Jo Jewell and Joao Breda were staff members of the WHO Regional Office for Europe at the time of the study. The authors are responsible for the views expressed in this publication and they do not necessarily represent the decisions or stated policy of WHO. All other authors declare that they have no other competing interests related to this review.
Ethics approval
The project received ethical approval by the Kazakh Academy of Nutrition Ethics Committee (Project #2524/ГФ4).
Informed consent
Each participant was briefed on the project and provided written informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trieu, K., Ospanova, F., Tazhibayev, S. et al. Sodium and potassium intakes in the Kazakhstan population estimated using 24-h urinary excretion: evidence for national action. Eur J Nutr 60, 1537–1546 (2021). https://doi.org/10.1007/s00394-020-02354-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02354-6