Abstract
Purpose
Anti-inflammatory and barrier-protective properties have been attributed to proanthocyanidins in the context of intestinal dysfunction, however little information is available about the impact of these phytochemicals on intestinal barrier integrity and immune response in the human. Here we assessed the putative protective properties of a grape-seed proanthocyanidin extract (GSPE) against dextran sodium sulfate (DSS)-induced acute dysfunction of the human colon in an Ussing chamber system.
Methods
Human proximal and distal colon tissues from colectomized patients were submitted ex vivo for a 30-min preventive GSPE treatment (50 or 200 µg mL−1) followed by 1-h incubation with DSS (12% w v−1). Transepithelial electrical resistance (TEER), permeation of a fluorescently-labeled dextran (FD4) and proinflammatory cytokine release [tumor necrosis factor (TNF)-α and interleukin (IL)-1β] of colonic tissues were determined.
Results
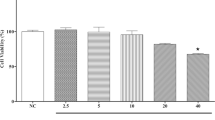
DSS reduced TEER (45–52%) in both the proximal and distal colon; however, significant increments in FD4 permeation (fourfold) and TNF-α release (61%) were observed only in the proximal colon. The preventive GSPE treatment decreased DSS-induced TEER loss (20–32%), FD4 permeation (66–73%) and TNF-α release (22–33%) of the proximal colon dose-dependently. The distal colon was not responsive to the preventive treatment but showed a reduction in IL-1β release below basal levels with the highest GSPE concentration.
Conclusions
Our results demonstrate potential preventive effects of GSPE on human colon dysfunction. Further studies are required to test whether administering GSPE could be a complementary therapeutic approach in colonic dysfunction associated with metabolic disorders and inflammatory bowel disease.





Similar content being viewed by others
References
Chelakkot C, Ghim J, Ryu SH (2018) Mechanisms regulating intestinal barrier integrity and its pathological implications. Exp Mol Med 50:103
Hamilton MK, Boudry G, Lemay DG, Raybould HE (2015) Changes in intestinal barrier function and gut microbiota in high-fat diet-fed rats are dynamic and region dependent. Am J Physiol Gastrointest Liver Physiol 308:G840–G851. https://doi.org/10.1152/ajpgi.00029.2015
Neurath MF (2014) Cytokines in inflammatory bowel disease. Nat Rev Immunol 14:329–342. https://doi.org/10.1038/nri3661
Duan Y, Zeng L, Zheng C et al (2018) Inflammatory links between high fat diets and diseases. Front Immunol 9:2649. https://doi.org/10.3389/fimmu.2018.02649
Boutagy NE, McMillan RP, Frisard MI, Hulver MW (2016) Metabolic endotoxemia with obesity: is it real and is it relevant? Biochimie 124:11–20. https://doi.org/10.1016/j.biochi.2015.06.020
Fukui H (2016) Increased intestinal permeability and decreased barrier function: does it really influence the risk of inflammation? Inflamm Intest Dis 1:135–145. https://doi.org/10.1159/000447252
Randhawa PK, Singh K, Singh N, Jaggi AS (2014) A review on chemical-induced inflammatory bowel disease models in rodents. Korean J Physiol Pharmacol 18:279–288. https://doi.org/10.4196/kjpp.2014.18.4.279
Eichele DD, Kharbanda KK (2017) Dextran sodium sulfate colitis murine model: an indispensable tool for advancing our understanding of inflammatory bowel diseases pathogenesis. World J Gastroenterol 23:6016–6029. https://doi.org/10.3748/wjg.v23.i33.6016
Laroui H, Ingersoll SA, Liu HC et al (2012) Dextran sodium sulfate (DSS) induces colitis in mice by forming nano-lipocomplexes with medium-chain-length fatty acids in the colon. PLoS One 7:e32084. https://doi.org/10.1371/journal.pone.0032084
Masumoto S, Terao A, Yamamoto Y et al (2016) Non-absorbable apple procyanidins prevent obesity associated with gut microbial and metabolomic changes. Sci Rep 6:31208. https://doi.org/10.1038/srep31208
Gil-Cardoso K, Ginés I, Pinent M et al (2018) The co-administration of proanthocyanidins and an obesogenic diet prevents the increase in intestinal permeability and metabolic endotoxemia derived to the diet. J Nutr Biochem 62:35–42. https://doi.org/10.1016/j.jnutbio.2018.07.012
Martin DA, Bolling BW (2015) A review of the efficacy of dietary polyphenols in experimental models of inflammatory bowel diseases. Food Funct 6:1773–1786. https://doi.org/10.1039/c5fo00202h
Smeriglio A, Barreca D, Bellocco E, Trombetta D (2017) Proanthocyanidins and hydrolysable tannins: occurrence, dietary intake and pharmacological effects. Br J Pharmacol 174:1244–1262. https://doi.org/10.1111/bph.13630
Li X-L, Cai Y-Q, Qin H, Wu Y-J (2008) Therapeutic effect and mechanism of proanthocyanidins from grape seeds in rats with TNBS-induced ulcerative colitis. Can J Physiol Pharmacol 86:841–849. https://doi.org/10.1139/Y08-089
Wang Y-H, Yang X-L, Wang L et al (2010) Effects of proanthocyanidins from grape seed on treatment of recurrent ulcerative colitis in rats. Can J Physiol Pharmacol 88:888–898. https://doi.org/10.1139/Y10-071
Cheah KY, Bastian SEP, Acott TMV et al (2013) Grape seed extract reduces the severity of selected disease markers in the proximal colon of dextran sulphate sodium-induced colitis in rats. Dig Dis Sci 58:970–977. https://doi.org/10.1007/s10620-012-2464-1
Terra X, Valls J, Vitrac X et al (2007) Grape-seed procyanidins act as antiinflammatory agents in endotoxin-stimulated RAW 264.7 macrophages by inhibiting NFkB signaling pathway. J Agric Food Chem 55:4357–4365. https://doi.org/10.1021/jf0633185
Wang Y-H, Ge B, Yang X-L et al (2011) Proanthocyanidins from grape seeds modulates the nuclear factor-kappa B signal transduction pathways in rats with TNBS-induced recurrent ulcerative colitis. Int Immunopharmacol 11:1620–1627. https://doi.org/10.1016/j.intimp.2011.05.024
Geraedts MCP, Troost FJ, Tinnemans R et al (2010) Release of satiety hormones in response to specific dietary proteins is different between human and murine small intestinal mucosa. Ann Nutr Metab 56:308–313. https://doi.org/10.1159/000312664
Sjöberg Å, Lutz M, Tannergren C et al (2013) Comprehensive study on regional human intestinal permeability and prediction of fraction absorbed of drugs using the Ussing chamber technique. Eur J Pharm Sci 48:166–180. https://doi.org/10.1016/J.EJPS.2012.10.007
Margalef M, Pons Z, Iglesias-Carres L et al (2016) Gender-related similarities and differences in the body distribution of grape seed flavanols in rats. Mol Nutr Food Res 60:760–772. https://doi.org/10.1002/mnfr.201500717
Pizarro TT, Stappenbeck TS, Rieder F et al (2019) Challenges in IBD research: preclinical human IBD mechanisms. Inflamm Bowel Dis 25:S5–S12. https://doi.org/10.1093/ibd/izz075
Wallon C, Braaf Y, Wolving M et al (2005) Endoscopic biopsies in Ussing chambers evaluated for studies of macromolecular permeability in the human colon. Scand J Gastroenterol 40:586–595. https://doi.org/10.1080/00365520510012235
Schmitz H, Barmeyer C, Gitter AH et al (2006) Epithelial barrier and transport function of the colon in ulcerative colitis. Ann N Y Acad Sci 915:312–326. https://doi.org/10.1111/j.1749-6632.2000.tb05259.x
Geraedts MCP, Troost FJ, De Ridder RJ et al (2012) Validation of Ussing chamber technology to study satiety hormone release from human duodenal specimens. Obesity 20:678–682. https://doi.org/10.1038/oby.2011.104
Viktoria VB, Evgeny LF, Larisa SO et al (2018) Increased paracellular permeability of tumor-adjacent areas in 1,2-dimethylhydrazine-induced colon carcinogenesis in rats. Cancer Biol Med 15:251. https://doi.org/10.20892/j.issn.2095-3941.2018.0016
Thomson A, Smart K, Somerville MS et al (2019) The Ussing chamber system for measuring intestinal permeability in health and disease. BMC Gastroenterol 19:98. https://doi.org/10.1186/s12876-019-1002-4
Araki Y, Sugihara H, Hattori T (2006) In vitro effects of dextran sulfate sodium on a Caco-2 cell line and plausible mechanisms for dextran sulfate sodium-induced colitis. Oncol Rep 16:1357–1362
Zhao H, Zhang H, Wu H et al (2012) Protective role of 1,25(OH)2 vitamin D3 in the mucosal injury and epithelial barrier disruption in DSS-induced acute colitis in mice. BMC Gastroenterol 12:57. https://doi.org/10.1186/1471-230X-12-57
Zhao H, Yan R, Zhou X et al (2016) Hydrogen sulfide improves colonic barrier integrity in DSS-induced inflammation in Caco-2 cells and mice. Int Immunopharmacol 39:121–127. https://doi.org/10.1016/j.intimp.2016.07.020
Van Dijk APM, Keuskamp ZJ, Wilson JHP, Zijlstra FJ (1995) Sequential release of cytokines, lipid mediators and nitric oxide in experimental colitis. Mediat Inflamm 4:186–190. https://doi.org/10.1155/S0962935195000305
Nagib MM, Tadros MG, Elsayed MI, Khalifa AE (2013) Anti-inflammatory and anti-oxidant activities of olmesartan medoxomil ameliorate experimental colitis in rats. Toxicol Appl Pharmacol 271:106–113. https://doi.org/10.1016/j.taap.2013.04.026
Ruder B, Atreya R, Becker C (2019) Tumour necrosis factor alpha in intestinal homeostasis and gut related diseases. Int J Mol Sci. https://doi.org/10.3390/ijms20081887
Kitajima S, Takuma S, Morimoto M (1999) Tissue distribution of dextran sulfate sodium (DSS) in the acute phase of murine DSS-induced colitis. J Vet Med Sci 61:67–70. https://doi.org/10.1292/jvms.61.67
Smythies LE, Sellers M, Clements RH et al (2005) Human intestinal macrophages display profound inflammatory anergy despite avid phagocytic and bactericidal activity. J Clin Invest 115:66. https://doi.org/10.1172/JCI19229
Kamada N, Hisamatsu T, Okamoto S et al (2008) Unique CD14 intestinal macrophages contribute to the pathogenesis of Crohn disease via IL-23/IFN-gamma axis. J Clin Invest 118:2269–2280. https://doi.org/10.1172/JCI34610
Roulis M, Armaka M, Manoloukos M et al (2011) Intestinal epithelial cells as producers but not targets of chronic TNF suffice to cause murine Crohn-like pathology. Proc Natl Acad Sci U S A 108:5396–5401. https://doi.org/10.1073/pnas.1007811108
Gil-Cardoso K, Comitato R, Ginés I et al (2019) Protective effect of proanthocyanidins in a rat model of mild intestinal inflammation and impaired intestinal permeability induced by LPS. Mol Nutr Food Res 63:1800720. https://doi.org/10.1002/mnfr.201800720
Gil-Cardoso K, Ginés I, Pinent M et al (2017) Chronic supplementation with dietary proanthocyanidins protects from diet-induced intestinal alterations in obese rats. Mol Nutr Food Res 61:1601039. https://doi.org/10.1002/mnfr.201601039
González-Quilen C, Gil-Cardoso K, Ginés I et al (2019) Grape-seed proanthocyanidins are able to reverse intestinal dysfunction and metabolic endotoxemia induced by a cafeteria diet in wistar rats. Nutrients. https://doi.org/10.3390/nu11050979
Wu H, Luo T, Li YM et al (2018) Granny Smith apple procyanidin extract upregulates tight junction protein expression and modulates oxidative stress and inflammation in lipopolysaccharide-induced Caco-2 cells. Food Funct 9:3321–3329. https://doi.org/10.1039/c8fo00525g
Li X, Yang X, Cai Y et al (2011) Proanthocyanidins from grape seeds modulate the NF-κB signal transduction pathways in rats with TNBS-induced ulcerative colitis. Molecules 16:6721–6731. https://doi.org/10.3390/molecules16086721
Ginés I, Gil-Cardoso K, Serrano J et al (2018) Effects of an intermittent grape-seed proanthocyanidin (GSPE) treatment on a cafeteria diet obesogenic challenge in rats. Nutrients 10:315. https://doi.org/10.3390/nu10030315
Siegmund B, Lehr H-A, Fantuzzi G, Dinarello CA (2001) IL-1 -converting enzyme (caspase-1) in intestinal inflammation. Proc Natl Acad Sci 98:13249–13254. https://doi.org/10.1073/pnas.231473998
Sanz-Pamplona R, Berenguer A, Cordero D et al (2014) Aberrant gene expression in mucosa adjacent to tumor reveals a molecular crosstalk in colon cancer. Mol Cancer 13:46. https://doi.org/10.1186/1476-4598-13-46
Monagas M, Urpi-Sarda M, Sánchez-Patán F et al (2010) Insights into the metabolism and microbial biotransformation of dietary flavan-3-ols and the bioactivity of their metabolites. Food Funct 1:233–253
Margalef M, Pons Z, Bravo FI et al (2015) Plasma kinetics and microbial biotransformation of grape seed flavanols in rats. J Funct Foods 12:478–488. https://doi.org/10.1016/j.jff.2014.12.007
Mena P, Bresciani L, Brindani N et al (2019) Phenyl-γ-valerolactones and phenylvaleric acids, the main colonic metabolites of flavan-3-ols: synthesis, analysis, bioavailability, and bioactivity. Nat Prod Rep 36:714–752
Wiese S, Esatbeyoglu T, Winterhalter P et al (2015) Comparative biokinetics and metabolism of pure monomeric, dimeric, and polymeric flavan-3-ols: a randomized cross-over study in humans. Mol Nutr Food Res 59:610–621. https://doi.org/10.1002/mnfr.201400422
Castello F, Costabile G, Bresciani L et al (2018) Bioavailability and pharmacokinetic profile of grape pomace phenolic compounds in humans. Arch Biochem Biophys 646:1–9. https://doi.org/10.1016/j.abb.2018.03.021
Sano A (2017) Safety assessment of 4-week oral intake of proanthocyanidin-rich grape seed extract in healthy subjects. Food Chem Toxicol 108:519–523. https://doi.org/10.1016/j.fct.2016.11.021
Acknowledgements
This research was funded by the Spanish Ministerio de Economía y Competitividad, Grants AGL2014-55347-R, AGL2017-83477-R, and 2014LINE-06 grant from the URV-Banco Santander. C. González-Quilen received financial support through a FI-AGAUR grant from the Generalitat de Catalunya, C. Grau-Bové is student fellow in the Martí i Franquès program of the Universitat Rovira i Virgili, Tarragona, Spain. M. Pinent and X. Terra are Serra-Húnter fellows at the Universitat Rovira i Virgili, Tarragona, Spain.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
González-Quilen, C., Grau-Bové, C., Jorba-Martín, R. et al. Protective properties of grape-seed proanthocyanidins in human ex vivo acute colonic dysfunction induced by dextran sodium sulfate. Eur J Nutr 60, 79–88 (2021). https://doi.org/10.1007/s00394-020-02222-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02222-3