Abstract
Purpose
This study was aimed to determine the impact of hydroxytyrosol (HT), a minor compound found in olive oil, on breast cancer stem cells (BCSCs) and the migration capacity of triple-negative breast cancer (TNBC) cell lines through the alteration of epithelial-to-mesenchymal transition (EMT) and embryonic signaling pathways.
Methods
BCSCs self-renewal was determined by the mammosphere-forming efficiency in SUM159PT, BT549, MDA-MB-231 and Hs578T TNBC cell lines. Flow cytometric analysis of CD44+/CD24−/low and aldehyde dehydrogenase positive (ALDH+) subpopulations, migration by the “wound healing assay”, invasion and Western blot of EMT markers and TGFβ signaling were investigated in SUM159PT, BT549 and MDA-MB-231 cell lines. Wnt/β-catenin signaling was assessed by Western blot in BT549 cells expressing WNT1 and MDA-MB-231 cells. Changes in TGFβ activity was determined by SMAD Binding Element (SBE) reporter assay.
Results
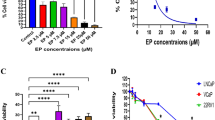
HT reduced BCSCs self-renewal, ALDH+ (aldehyde dehydrogenase) and CD44+/CD24−/low subpopulations, tumor cell migration and invasion. Consistently, HT suppressed Wnt/β-catenin signaling by decreasing p-LRP6, LRP6, β-catenin and cyclin D1 protein expression and the EMT markers SLUG, ZEB1, SNAIL and VIMENTIN. Finally, HT inhibited p-SMAD2/3 and SMAD2/3 in SUM159PT, BT549 and MDA-MB-231 cells, what was correlated with a less TGFβ activity.
Conclusion
In conclusion, we report for the first time the inhibitory role of HT on BCSCs and tumor cell migration by targeting EMT, Wnt/β-catenin and TGFβ signaling pathways. Our findings highlight the importance of the chemopreventive compound HT as a novel candidate to be investigated as an alternative targeted therapy for TNBC.






Similar content being viewed by others
References
Foulkes WD, Smith IE, Reis-Filho JS (2010) Triple-negative breast cancer. N Engl J Med 363:1938–1948. https://doi.org/10.1056/NEJMra1001389
González-González A, Muñoz-Muela E, Marchal JA et al (2018) Activating transcription factor 4 modulates TGFβ-induced aggressiveness in triple negative breast cancer via SMAD2/3/4 and mTORC2 signaling. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-17-3125
Lehmann BD, Bauer JA, Chen X et al (2011) Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121:2750–2767. https://doi.org/10.1172/JCI45014
Idowu MO, Kmieciak M, Dumur C et al (2012) CD44(+)/CD24(-/low) cancer stem/progenitor cells are more abundant in triple-negative invasive breast carcinoma phenotype and are associated with poor outcome. Hum Pathol 43:364–373. https://doi.org/10.1016/j.humpath.2011.05.005
Bianchini G, Balko JM, Mayer IA et al (2016) Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol 13:674–690. https://doi.org/10.1038/nrclinonc.2016.66
Al-Hajj M, Wicha MS, Benito-Hernandez A et al (2003) Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA 100:3983–3988. https://doi.org/10.1073/pnas.0530291100
Ginestier C, Hur MH, Charafe-Jauffret E et al (2007) ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell 1:555–567. https://doi.org/10.1016/j.stem.2007.08.014
Charafe-Jauffret E, Ginestier C, Iovino F et al (2009) Breast cancer cell lines contain functional cancer stem cells with metastatic capacity and a distinct molecular signature. Cancer Res 69:1302–1313. https://doi.org/10.1158/0008-5472.CAN-08-2741
Brooks MD, Burness ML, Wicha MS (2015) Therapeutic implications of cellular heterogeneity and plasticity in breast cancer. Cell Stem Cell 17:260–271. https://doi.org/10.1016/j.stem.2015.08.014
Mani SA, Guo W, Liao M et al (2008) The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133:704–715. https://doi.org/10.1016/j.cell.2008.03.027
Takebe N, Warren RQ, Ivy SP (2011) Breast cancer growth and metastasis: interplay between cancer stem cells, embryonic signaling pathways and epithelial-to-mesenchymal transition. Breast Cancer Res 13:211. https://doi.org/10.1186/bcr2876
Kalluri R, Weinberg RA (2009) The basics of epithelial–mesenchymal transition. J Clin Invest 119:1420–1428. https://doi.org/10.1172/JCI39104
Fischer KR, Durrans A, Lee S et al (2015) Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature 527:472–476. https://doi.org/10.1038/nature15748
Granados-Principal S, Quiles JL, Ramirez-Tortosa CL et al (2010) Hydroxytyrosol: from laboratory investigations to future clinical trials. Nutr Rev 68:191–206. https://doi.org/10.1111/j.1753-4887.2010.00278.x
Granados-Principal S, Quiles JL, Ramirez-Tortosa CL et al (2012) Squalene ameliorates atherosclerotic lesions through the reduction of CD36 scavenger receptor expression in macrophages. Mol Nutr Food Res 56:733–740. https://doi.org/10.1002/mnfr.201100703
Granados-Principal S, Quiles JL, Ramirez-Tortosa CL et al (2010) New advances in molecular mechanisms and the prevention of adriamycin toxicity by antioxidant nutrients. Food Chem Toxicol 48:1425–1438. https://doi.org/10.1016/j.fct.2010.04.007
Granados-Principal S, El-Azem N, Pamplona R et al (2014) Hydroxytyrosol ameliorates oxidative stress and mitochondrial dysfunction in doxorubicin-induced cardiotoxicity in rats with breast cancer. Biochem Pharmacol 90:25–33. https://doi.org/10.1016/j.bcp.2014.04.001
Granados-Principal S, Quiles JL, Ramirez-Tortosa C et al (2011) Hydroxytyrosol inhibits growth and cell proliferation and promotes high expression of sfrp4 in rat mammary tumours. Mol Nutr Food Res 55(Suppl 1):S117–S126. https://doi.org/10.1002/mnfr.201000220
Dass RA, Sarshad AA, Carson BB et al (2016) Wnt5a signals through DVL1 to repress ribosomal DNA transcription by RNA polymerase I. PLoS Genet 12:e1006217. https://doi.org/10.1371/journal.pgen.1006217
Choi DS, Blanco E, Kim Y-S et al (2014) Chloroquine eliminates cancer stem cells through deregulation of Jak2 and DNMT1. Stem Cells 32:2309–2323. https://doi.org/10.1002/stem.1746
Dave B, Granados-Principal S, Zhu R et al (2014) Targeting RPL39 and MLF2 reduces tumor initiation and metastasis in breast cancer by inhibiting nitric oxide synthase signaling. Proc Natl Acad Sci USA 111:8838–8843. https://doi.org/10.1073/pnas.1320769111
Granados-Principal S, Liu Y, Guevara ML et al (2015) Inhibition of iNOS as a novel effective targeted therapy against triple-negative breast cancer. Breast Cancer Res 17:25. https://doi.org/10.1186/s13058-015-0527-x
Chiang K, Zielinska AE, Shaaban AM et al (2017) PRMT5 is a critical regulator of breast cancer stem cell function via histone methylation and FOXP1 expression. Cell Rep 21:3498–3513. https://doi.org/10.1016/j.celrep.2017.11.096
Liu S, Cong Y, Wang D et al (2014) Breast cancer stem cells transition between epithelial and mesenchymal states reflective of their normal counterparts. Stem Cell Rep 2:78–91. https://doi.org/10.1016/j.stemcr.2013.11.009
Liu C-C, Prior J, Piwnica-Worms D, Bu G (2010) LRP6 overexpression defines a class of breast cancer subtype and is a target for therapy. Proc Natl Acad Sci USA 107:5136–5141. https://doi.org/10.1073/pnas.0911220107
King TD, Suto MJ, Li Y (2012) The Wnt/β-catenin signaling pathway: a potential therapeutic target in the treatment of triple negative breast cancer. J Cell Biochem 113:13–18. https://doi.org/10.1002/jcb.23350
Guo W, Keckesova Z, Donaher JL et al (2012) Slug and Sox9 cooperatively determine the mammary stem cell state. Cell 148:1015–1028. https://doi.org/10.1016/j.cell.2012.02.008
Jitariu A, Cîmpean AM, Ribatti D, Raica M (2017) Triple negative breast cancer: the kiss of death. Oncotarget 8:46652–46662. https://doi.org/10.18632/oncotarget.16938
Bhola NE, Balko JM, Dugger TC et al (2013) TGF-β inhibition enhances chemotherapy action against triple-negative breast cancer. J Clin Invest 123:1348–1358. https://doi.org/10.1172/JCI65416
Jhan J-R, Andrechek ER (2017) Effective personalized therapy for breast cancer based on predictions of cell signaling pathway activation from gene expression analysis. Oncogene 36:3553–3561. https://doi.org/10.1038/onc.2016.503
Li X, Lewis MT, Huang J et al (2008) Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. J Natl Cancer Inst 100:672–679. https://doi.org/10.1093/jnci/djn123
Diehn M, Cho RW, Lobo NA et al (2009) Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature 458:780–783. https://doi.org/10.1038/nature07733
Creighton CJ, Li X, Landis M et al (2009) Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci USA 106:13820–13825. https://doi.org/10.1073/pnas.0905718106
Liedtke C, Mazouni C, Hess KR et al (2008) Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol 26:1275–1281. https://doi.org/10.1200/JCO.2007.14.4147
Li Y, Wicha MS, Schwartz SJ, Sun D (2011) Implications of cancer stem cell theory for cancer chemoprevention by natural dietary compounds. J Nutr Biochem 22:799–806. https://doi.org/10.1016/j.jnutbio.2010.11.001
Kakarala M, Brenner DE, Korkaya H et al (2010) Targeting breast stem cells with the cancer preventive compounds curcumin and piperine. Breast Cancer Res Treat 122:777–785. https://doi.org/10.1007/s10549-009-0612-x
Li Y, Zhang T, Korkaya H et al (2010) Sulforaphane, a dietary component of broccoli/broccoli sprouts, inhibits breast cancer stem cells. Clin Cancer Res 16:2580–2590. https://doi.org/10.1158/1078-0432.CCR-09-2937
Avtanski DB, Nagalingam A, Bonner MY et al (2014) Honokiol inhibits epithelial-mesenchymal transition in breast cancer cells by targeting signal transducer and activator of transcription 3/Zeb1/E-cadherin axis. Mol Oncol 8:565–580. https://doi.org/10.1016/j.molonc.2014.01.004
Charpentier MS, Whipple RA, Vitolo MI et al (2014) Curcumin targets breast cancer stem-like cells with microtentacles that persist in mammospheres and promote reattachment. Cancer Res 74:1250–1260. https://doi.org/10.1158/0008-5472.CAN-13-1778
Fu Y, Chang H, Peng X et al (2014) Resveratrol inhibits breast cancer stem-like cells and induces autophagy via suppressing Wnt/β-catenin signaling pathway. PLoS One 9:e102535. https://doi.org/10.1371/journal.pone.0102535
Wang N, Wang Z, Wang Y et al (2015) Dietary compound isoliquiritigenin prevents mammary carcinogenesis by inhibiting breast cancer stem cells through WIF1 demethylation. Oncotarget 6:9854–9876. https://doi.org/10.18632/oncotarget.3396
Fu J, Ke X, Tan S et al (2016) The natural compound codonolactone attenuates TGF-β1-mediated epithelial-to-mesenchymal transition and motility of breast cancer cells. Oncol Rep 35:117–126. https://doi.org/10.3892/or.2015.4394
Sun M, Zhang N, Wang X et al (2016) Hedgehog pathway is involved in nitidine chloride induced inhibition of epithelial–mesenchymal transition and cancer stem cells-like properties in breast cancer cells. Cell Biosci 6:44. https://doi.org/10.1186/s13578-016-0104-8
Wang N, Wang Q, Tang H et al (2017) Direct inhibition of ACTN4 by ellagic acid limits breast cancer metastasis via regulation of β-catenin stabilization in cancer stem cells. J Exp Clin Cancer Res 36:172. https://doi.org/10.1186/s13046-017-0635-9
Li X, Meng Y, Xie C et al (2018) Diallyl Trisulfide inhibits breast cancer stem cells via suppression of Wnt/β-catenin pathway. J Cell Biochem 119:4134–4141. https://doi.org/10.1002/jcb.26613
Christian MS, Sharper VA, Hoberman AM et al (2004) The toxicity profile of hydrolyzed aqueous olive pulp extract. Drug Chem Toxicol 27:309–330. https://doi.org/10.1081/DCT-200039714
González-Santiago M, Fonollá J, Lopez-Huertas E (2010) Human absorption of a supplement containing purified hydroxytyrosol, a natural antioxidant from olive oil, and evidence for its transient association with low-density lipoproteins. Pharmacol Res 61:364–370. https://doi.org/10.1016/j.phrs.2009.12.016
Khymenets O, Fitó M, Touriño S et al (2010) Antioxidant activities of hydroxytyrosol main metabolites do not contribute to beneficial health effects after olive oil ingestion. Drug Metab Dispos 38:1417–1421. https://doi.org/10.1124/dmd.110.032821
Corominas-Faja B, Cuyàs E, Lozano-Sánchez J et al (2018) Extra-virgin olive oil contains a metabolo-epigenetic inhibitor of cancer stem cells. Carcinogenesis 39:601–613. https://doi.org/10.1093/carcin/bgy023
Wang Q-L, Tao Y-Y, Yuan J-L et al (2010) Salvianolic acid B prevents epithelial-to-mesenchymal transition through the TGF-beta1 signal transduction pathway in vivo and in vitro. BMC Cell Biol 11:31. https://doi.org/10.1186/1471-2121-11-31
Davies AH, Reipas K, Hu K et al (2015) Inhibition of RSK with the novel small-molecule inhibitor LJI308 overcomes chemoresistance by eliminating cancer stem cells. Oncotarget 6:20570–20577. https://doi.org/10.18632/oncotarget.4135
Li Y, Jiang F, Chen L et al (2015) Blockage of TGFβ-SMAD2 by demethylation-activated miR-148a is involved in caffeic acid-induced inhibition of cancer stem cell-like properties in vitro and in vivo. FEBS Open Bio 5:466–475. https://doi.org/10.1016/j.fob.2015.05.009
Dandawate PR, Subramaniam D, Jensen RA, Anant S (2016) Targeting cancer stem cells and signaling pathways by phytochemicals: novel approach for breast cancer therapy. Semin Cancer Biol 40–41:192–208. https://doi.org/10.1016/j.semcancer.2016.09.001
Farahmand L, Darvishi B, Majidzadeh -AK, Madjid Ansari A (2017) Naturally occurring compounds acting as potent anti-metastatic agents and their suppressing effects on Hedgehog and WNT/β-catenin signalling pathways. Cell Prolif. https://doi.org/10.1111/cpr.12299
Lin D, Kuang G, Wan J et al (2017) Luteolin suppresses the metastasis of triple-negative breast cancer by reversing epithelial-to-mesenchymal transition via downregulation of β-catenin expression. Oncol Rep 37:895–902. https://doi.org/10.3892/or.2016.5311
Bhuvanalakshmi G, Rangappa KS et al (2017) Breast cancer stem-like cells are inhibited by diosgenin, a steroidal saponin, by the attenuation of the Wnt β-Catenin signaling via the Wnt antagonist secreted frizzled related protein-4. Front Pharmacol 8:124. https://doi.org/10.3389/fphar.2017.00124
Li Y, Lu W, King TD et al (2010) Dkk1 stabilizes Wnt co-receptor LRP6: implication for Wnt ligand-induced LRP6 down-regulation. PLoS One 5:e11014. https://doi.org/10.1371/journal.pone.0011014
Guo X, Wang X-F (2009) Signaling cross-talk between TGF-beta/BMP and other pathways. Cell Res 19:71–88. https://doi.org/10.1038/cr.2008.302
Zhou B, Liu Y, Kahn M et al (2012) Interactions between β-catenin and transforming growth factor-β signaling pathways mediate epithelial-mesenchymal transition and are dependent on the transcriptional co-activator cAMP-response element-binding protein (CREB)-binding protein (CBP). J Biol Chem 287:7026–7038. https://doi.org/10.1074/jbc.M111.276311
Murillo-Garzón V, Gorroño-Etxebarria I, Åkerfelt M et al (2018) Frizzled-8 integrates Wnt-11 and transforming growth factor-β signaling in prostate cancer. Nat Commun 9:1747. https://doi.org/10.1038/s41467-018-04042-w
Sundqvist A, Morikawa M, Ren J et al (2018) JUNB governs a feed-forward network of TGFβ signaling that aggravates breast cancer invasion. Nucleic Acids Res 46:1180–1195. https://doi.org/10.1093/nar/gkx1190
El-Azem N, Pulido-Moran M, Ramirez-Tortosa CL et al (2018) Modulation by hydroxytyrosol of oxidative stress and antitumor activities of paclitaxel in breast cancer. Eur J Nutr 0:1–9. https://doi.org/10.1007/s00394-018-1638-9
Acknowledgements
Funding was provided by Instituto de Salud Carlos III (CP14/00197, PI15/00336, PIE16/00045), European Regional Development Fund (European Union), and the Chair “Doctors Galera-Requena in Cancer Stem Cell Research”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interests.
Rights and permissions
About this article
Cite this article
Cruz-Lozano, M., González-González, A., Marchal, J.A. et al. Hydroxytyrosol inhibits cancer stem cells and the metastatic capacity of triple-negative breast cancer cell lines by the simultaneous targeting of epithelial-to-mesenchymal transition, Wnt/β-catenin and TGFβ signaling pathways. Eur J Nutr 58, 3207–3219 (2019). https://doi.org/10.1007/s00394-018-1864-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1864-1