Abstract
Purpose
Fatalities due to heart and cerebrovascular diseases caused by uncontrolled hyperlipidaemia increase every year; on the other hand, lipid-lowering drugs are known to cause side effects. The gut microbiota has been thoroughly investigated by researchers and consumers, because they have unique functional properties and littler side effects. However, the effects of the gut microbiota remain controversial. We conducted a meta-analysis to assess the effects of products designed to modulate the gut microbiota on various hyperlipidaemias.
Methods
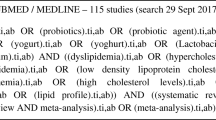
We systematically searched PubMed, Embase, Cochrane Library (Central), and Web of Science for randomized controlled trials (published before June 2017, and those only in English) to compare treatment (products designed to modulate the gut microbiota) versus placebo. Our main endpoints were total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) in serum. We assessed pooled data using a fixed effects model.
Results
Of 1337 identified studies, 21 were eligible and included in our analysis (n = 1436 participants). The combined estimate of effect size for the impact of products designed to modulate the gut microbiota on serum TC (WMD − 11.07 mg/dL, 95% CI − 13.72 to − 8.43, p < 0.001), LDL-C (WMD − 10.96 mg/dL, 95% CI − 13.37 to − 8.56, p < 0.001), and HDL-C (WMD 0.72 mg/dL, 95% CI 0.06–1.38, p = 0.032) were statistically significant, while no significant effect was found on TG concentrations (WMD − 0.56 mg/dL, 95% CI − 5.59 to 4.47, p = 0.828). Subgroup analysis showed parallel trials, probiotics, and long-term intervention had better effects on lowering blood lipid levels.
Conclusion
Products designed to modulate the gut microbiota results in changes of the plasma lipid concentrations and these changes may protect against cardiovascular disease.










Similar content being viewed by others
Abbreviations
- AHA:
-
American Heart Association
- ATP III:
-
Adult treatment panel III
- BMI:
-
Body mass index
- HDL-C:
-
High density lipoprotein cholesterol
- LDL-C:
-
Low density lipoprotein cholesterol
- NCEP:
-
National Cholesterol Education Program
- PRISMA:
-
Preferred reporting items for systematic meta-analysis
- RCTs:
-
Randomized controlled trials
- SD:
-
Standard deviation
- SEM:
-
Standard error of the mean
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- WHO:
-
World Health Organization
- WMD:
-
Weighted mean difference
References
Owens AP, Byrnes JR, Mackman N (2014) Hyperlipidemia, tissue factor, coagulation, and simvastatin. Trends Cardiovasc Med 24(3):95–98. https://doi.org/10.1016/j.tcm.2013.07.003
Mitchell S, Roso S, Samuel M, Pladevall-Vila M (2016) Unmet need in the hyperlipidaemia population with high risk of cardiovascular disease: a targeted literature review of observational studies. BMC Cardiovasc Disord 16(1):74–84. https://doi.org/10.1186/s12872-016-0241-3
Committee of Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults (2016) Chinese guidelines on prevention and treatment of dyslipidemia in adults. Chin Circ J 31(10):937–953. https://doi.org/10.3969/j.issn.1000-3614.2016.10.001
Obesity CRi (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation 106(25):3143–3421
Abel ED, Litwin SE, Sweeney G (2008) Cardiac remodeling in obesity. Physiol Rev 88(2):389–419. https://doi.org/10.1152/physrev.00017.2007
Wang Y, Liu D, Li Y, Guo L, Cui Y, Zhang X, Li E (2016) Metabolomic analysis of serum from obese adults with hyperlipemia by UHPLC-Q-TOF MS/MS. Biomed Chromatogr 30(1):48–54. https://doi.org/10.1002/bmc.3491
Chen Y-L, Xiao C-H, Hu Z-X, Liu X-S, Liu Z, Zhang W-N, Zhao X-J (2017) Dynamic lipid profile of hyperlipidemia mice. J Chromatogr B 1055–1056:165–171. https://doi.org/10.1016/j.jchromb.2017.04.017
Taylor BL, Woodfall GE, Sheedy KE, O’Riley ML, Rainbow KA, Bramwell EL, Kellow NJ (2017) Effect of probiotics on metabolic outcomes in pregnant women with gestational diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutrients 9(5):461–474. https://doi.org/10.3390/nu9050461
Flint HJ, Scott KP, Louis P, Duncan SH (2012) The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol 9(10):577–589
Sanders Mary E (2008) Probiotics: definition, sources, selection, and uses. Clin Infect Dis 46(s2):S58–S61. https://doi.org/10.1086/523341
Gourbeyre P, Denery S, Bodinier M (2011) Probiotics, prebiotics, and synbiotics: impact on the gut immune system and allergic reactions. J Leukoc Biol 89(5):685–695. https://doi.org/10.1189/jlb.1109753
Cani PD, Neyrinck AM, Fava F, Knauf C, Burcelin RG, Tuohy KM, Gibson GR, Delzenne NM (2007) Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia 50(11):2374–2383. https://doi.org/10.1007/s00125-007-0791-0
Nicolucci AC, Reimer RA (2017) Prebiotics as a modulator of gut microbiota in paediatric obesity. Pediatr Obes 12(4):265–273. https://doi.org/10.1111/ijpo.12140
Bagarolli RA, Tobar N, Oliveira AG, Araújo TG, Carvalho BM, Rocha GZ, Vecina JF, Calisto K, Guadagnini D, Prada PO, Santos A, Saad STO, Saad MJA (2017) Probiotics modulate gut microbiota and improve insulin sensitivity in DIO mice. J Nutr Biochem 50:16–25. https://doi.org/10.1016/j.jnutbio.2017.08.006
Wang Y, Sun J, Zhong H, Li N, Xu H, Zhu Q, Liu Y (2017) Effect of probiotics on the meat flavour and gut microbiota of chicken. Sci Rep. https://doi.org/10.1038/s41598-017-06677-z
De Roos NM, Scheuten G, Katan MB (1999) Yoghurt enriched with Lactobacillus acidophilus does not lower blood lipids in healthy men and women with normal to borderline high serum cholesterol levels. Eur J Clin Nutr 53(4):277–280
Lewis SJ, Burmeister S (2005) A double-blind placebo-controlled study of the effects of Lactobacillus acidophilus on plasma lipids. Eur J Clin Nutr 59(6):776–780. https://doi.org/10.1038/sj.ejcn.1602139
Simons LA, Amansec SG, Conway P (2006) Effect of Lactobacillus fermentum on serum lipids in subjects with elevated serum cholesterol. Nutr Metabol Cardiovasc Dis 16(8):531–535. https://doi.org/10.1016/j.numecd.2005.10.009
Andrade S, Borges N (2009) Effect of fermented milk containing Lactobacillus acidophilus and Bifidobacterium longum on plasma lipids of women with normal or moderately elevated cholesterol. J Dairy Res 76(4):469–474. https://doi.org/10.1017/S0022029909990173
Ejtahed HS, Mohtadi-Nia J, Homayouni-Rad A, Niafar M, Asghari-Jafarabadi M, Mofid V, Akbarian-Moghari A (2011) Effect of probiotic yogurt containing Lactobacillus acidophilus and Bifidobacterium lactis on lipid profile in individuals with type 2 diabetes mellitus. J Dairy Sci 94(7):3288–3294. https://doi.org/10.3168/jds.2010-4128
Asemi Z, Samimi M, Tabasi Z, Talebian P, Azarbad Z, Hydarzadeh Z, Esmaillzadeh A (2012) Effect of daily consumption of probiotic yoghurt on lipid profiles in pregnant women: a randomized controlled clinical trial. J Mater Fetal Neonatal Med 25 (9):1552–1556. https://doi.org/10.3109/14767058.2011.640372
Jones ML, Martoni CJ, Parent M, Prakash S (2012) Cholesterol-lowering efficacy of a microencapsulated bile salt hydrolase-active Lactobacillus reuteri NCIMB 30242 yoghurt formulation in hypercholesterolaemic adults. Br J Nutr 107(10):1505–1513. https://doi.org/10.1017/S0007114511004703
Agerholm-Larsen LBM, Grunwald GK, Astrup A (2000) The effect of a probiotic milk product on plasma cholesterol: a meta-analysis of short-term intervention studies. Eur J Clin Nutr 54:856–860
Guo Z, Liu XM, Zhang QX, Shen Z, Tian FW, Zhang H, Sun ZH, Zhang HP, Chen W (2011) Influence of consumption of probiotics on the plasma lipid profile: a meta-analysis of randomised controlled trials. Nutr Metabol Cardiovasc Dis 21(11):844–850. https://doi.org/10.1016/j.numecd.2011.04.008
Cho YA, Kim J (2015) Effect of probiotics on blood lipid concentrations a meta-analysis of randomized controlled trials. Medicine 94(43):e1714–e1724. https://doi.org/10.1097/md.0000000000001714
Shimizu M, Hashiguchi M, Shiga T, Tamura HO, Mochizuki M (2015) Meta-Analysis: Effects of probiotic supplementation on lipid profiles in normal to mildly hypercholesterolemic individuals. PLoS One 10(10):e0139795. https://doi.org/10.1371/journal.pone.0139795
Puri S, Sharma S, Kurpad A (2016) Potential of probiotics in hypercholesterolemia: a meta-analysis. Indian J Pub Health 60(4):280–286. https://doi.org/10.4103/0019-557x.195859
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56(2):455–463
Wang Y, Ames NP, Tun HM, Tosh SM, Jones PJ, Khafipour E (2016) High molecular weight barley β-glucan alters gut microbiota toward reduced cardiovascular disease risk. Front Microbiol 7:129–144. https://doi.org/10.3389/fmicb.2016.00129
Larkin TA, Astheimer LB, Price WE (2009) Dietary combination of soy with a probiotic or prebiotic food significantly reduces total and LDL cholesterol in mildly hypercholesterolaemic subjects. Eur J Clin Nutr 63(2):238–245. https://doi.org/10.1038/sj.ejcn.1602910
Bertolami MC, Faludi AA, Batlouni M (1999) Evaluation of the effects of a new fermented milk product (Gaio) on primary hypercholesterolemia. Eur J Clin Nutr 53(2):97–101
Kiessling G, Schneider J, Jahreis G (2002) Long-term consumption of fermented dairy products over 6 months increases HDL cholesterol. Eur J Clin Nutr 56(9):843–849. https://doi.org/10.1038/sj.ejcn.1601399
St-Onge MP, Farnworth ER, Savard T, Chabot D, Mafu A, Jones PJ (2002) Kefir consumption does not alter plasma lipid levels or cholesterol fractional synthesis rates relative to milk in hyperlipidemic men: a randomized controlled trial. BMC Complement Altern Med 2:1–7
Xiao JZ, Kondo S, Takahashi N, Miyaji K, Oshida K, Hiramatsu A, Iwatsuki K, Kokubo S, Hosono A (2003) Effects of milk products fermented by Bifidobacterium longum on blood lipids in rats and healthy adult male volunteers. J Dairy Sci 86(7):2452–2461
Giacco R, Clemente G, Luongo D, Lasorella G, Fiume I, Brouns F, Bornet F, Patti L, Cipriano P, Rivellese AA, Riccardi G (2004) Effects of short-chain fructo-oligosaccharides on glucose and lipid metabolism in mild hypercholesterolaemic individuals. Clin Nutr 23(3):331–340. https://doi.org/10.1016/j.clnu.2003.07.010
Hlivak P, Odraska J, Ferencik M, Ebringer L, Jahnova E, Mikes Z (2005) One-year application of probiotic strain Enterococcus faecium M-74 decreases serum cholesterol levels. Bratislavské lekárske listy 106(2):67–72
Hatakka K, Mutanen M, Holma R, Saxelin M, Korpela R (2008) Lactobacillus rhamnosus LC705 together with Propionibacterium freudenreichii ssp shermanii JS administered in capsules is ineffective in lowering serum lipids. J Am Coll Nutr 27(4):441–447
Ataie-Jafari A, Larijani B, Alavi Majd H, Tahbaz F (2009) Cholesterol-lowering effect of probiotic yogurt in comparison with ordinary yogurt in mildly to moderately hypercholesterolemic subjects. Ann Nutr Metabol 54(1):22–27. https://doi.org/10.1159/000203284
Ooi LG, Ahmad R, Yuen KH, Liong MT (2010) Lactobacillus acidophilus CHO-220 and inulin reduced plasma total cholesterol and low-density lipoprotein cholesterol via alteration of lipid transporters. J Dairy Sci 93(11):5048–5058. https://doi.org/10.3168/jds.2010-3311
Berthold HK, Schulte DM, Lapointe JF, Lemieux P, Krone W, Gouni-Berthold I (2011) The whey fermentation product malleable protein matrix decreases triglyceride concentrations in subjects with hypercholesterolemia: a randomized placebo-controlled trial1. J Dairy Sci 94(2):589–601. https://doi.org/10.3168/jds.2010-3115
Jones ML, Martoni CJ, Prakash S (2012) Cholesterol lowering and inhibition of sterol absorption by Lactobacillus reuteri NCIMB 30242: a randomized controlled trial. Eur J Clin Nutr 66(11):1234–1241. https://doi.org/10.1038/ejcn.2012.126
Fuentes MC, Lajo T, Carrion JM, Cune J (2013) Cholesterol-lowering efficacy of Lactobacillus plantarum CECT 7527, 7528 and 7529 in hypercholesterolaemic adults. Br J Nutr 109(10):1866–1872. https://doi.org/10.1017/s000711451200373x
Ogawa A, Kadooka Y, Kato K, Shirouchi B, Sato M (2014) Lactobacillus gasseri SBT2055 reduces postprandial and fasting serum non-esterified fatty acid levels in Japanese hypertriacylglycerolemic subjects. Lipids Health Dis 13:36–44. https://doi.org/10.1186/1476-511x-13-36
Ahn HY, Kim M, Ahn YT, Sim JH, Choi ID, Lee SH, Lee JH (2015) The triglyceride-lowering effect of supplementation with dual probiotic strains, Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032: reduction of fasting plasma lysophosphatidylcholines in nondiabetic and hypertriglyceridemic subjects. Nutr Metabol Cardiovasc Dis 25(8):724–733. https://doi.org/10.1016/j.numecd.2015.05.002
Rerksuppaphol S, Rerksuppaphol L (2015) A randomized double-blind controlled trial of Lactobacillus acidophilus plus bifidobacterium bifidum versus placebo in patients with hypercholesterolemia. J Clin Diagn Res 9(3):KC01–K04. https://doi.org/10.7860/JCDR/2015/11867.5728
Cavallini DC, Manzoni MS, Bedani R, Roselino MN, Celiberto LS, Vendramini RC, de Valdez G, Abdalla DS, Pinto RA, Rosetto D, Valentini SR, Rossi EA (2016) Probiotic soy product supplemented with isoflavones improves the lipid profile of moderately hypercholesterolemic men: a randomized controlled trial. Nutrients 8(1):52–70. https://doi.org/10.3390/nu8010052
Fuentes MC, Lajo T, Carrion JM, Cune J (2016) A randomized clinical trial evaluating a proprietary mixture of Lactobacillus plantarum strains for lowering cholesterol. Mediterr J Nutr Metabol 9(2):125–135. https://doi.org/10.3233/MNM-160065
Tan S, Zhao A, Zheng Y, Wang P, Zhang Y (2017) Effects of Lactobacillus paracasei N1115 on intestinal microbiota and serum lipid of dyslipidemias. FASEB J 31 (1 Supplement):45–46
Gilliland SE, Nelson CR, Maxwell C (1985) Assimilation of cholesterol by Lactobacillus acidophilus. Appl Environ Microbiol 49(2):377–381
Pereira DI, Gibson GR (2002) Cholesterol assimilation by lactic acid bacteria and bifidobacteria isolated from the human gut. Appl Environ Microbiol 68(9):4689–4693
Liong MT, Shah NP (2005) Bile salt deconjugation and BSH activity of five bifidobacterial strains and their cholesterol co-precipitating properties. Food Res Int 38(2):135–142. https://doi.org/10.1016/j.foodres.2004.08.003
Tahri K, Grill JP, Schneider F (1997) Involvement of trihydroxyconjugated bile salts in cholesterol assimilation by bifidobacteria. Curr Microbiol 34(2):79–84
Zhao JR, Yang H (2005) Progress in the effect of probiotics on cholesterol and its mechanism. Wei sheng wu xue bao = Acta microbiologica Sinica 45(2):315–319
Huang Y, Zheng Y (2010) The probiotic Lactobacillus acidophilus reduces cholesterol absorption through the down-regulation of Niemann-Pick C1-like 1 in Caco-2 cells. Br J Nutr 103(4):473–478. https://doi.org/10.1017/s0007114509991991
Lye H-S, Rahmat-Ali GR, Liong M-T (2010) Mechanisms of cholesterol removal by lactobacilli under conditions that mimic the human gastrointestinal tract. Int Dairy J 20(3):169–175. https://doi.org/10.1016/j.idairyj.2009.10.003
Sterne JA, Egger M, Smith GD (2001) Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 323(7304):101–105
Acknowledgements
This research was supported by the National Natural Science Foundation of China (81703677). The assistance of the staff is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deng, X., Ma, J., Song, M. et al. Effects of products designed to modulate the gut microbiota on hyperlipidaemia. Eur J Nutr 58, 2713–2729 (2019). https://doi.org/10.1007/s00394-018-1821-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1821-z



