Abstract
Purpose
Intake of specific nutrients has been linked to mental states and various indices of cognitive performance although the effects are often subtle and difficult to interpret. Measurement of so-called objective variables (e.g. reaction times) is often considered to be the gold standard for assessing outcomes in this field of research. It can, however, be argued that data on subjective experience (e.g. mood) are also important and may enrich existing objective data. The aim of this review is to evaluate methods for measuring mental performance and mood, considering the definition of subjective mood and the validity of measures of subjective experience.
Methods
A multi-stakeholder expert group was invited by ILSI Europe to come to a consensus around the utility of objective and subjective measurement in this field, which forms the basis of the paper. Therefore, the present review reflects a succinct overview of the science but is not intended to be a systematic review.
Results
The proposed approach extends the traditional methodology using standard ‘objective’ measurements to also include the consumers’ subjective experiences in relation to food. Specific recommendations include 1) using contemporary methods to capture transient mood states; 2) using sufficiently sensitive measures to capture effects of nutritional intervention; 3) considering the possibility that subjective and objective responses will occur over different time frames; and 4) recognition of the importance of expectancy and placebo effects for subjective measures.
Conclusions
The consensus reached was that the most informative approach should involve collection and consideration of both objective and subjective data.
Similar content being viewed by others
Introduction
Nutrition plays an important role in brain function throughout the entire lifespan. Appropriate nutrient intake allows normal brain growth and neurodevelopment in early life and reduces the risk of cognitive decline and Alzheimer’s disease in older age [1, 2]. Our knowledge about nutrition has greatly evolved over the last 50 years, and in developed countries, food is no longer seen uniquely as a survival necessity and a primary need, but is associated with promotion of mental fitness [3–5]. The effects of nutrients on cognitive performance—mental processes (e.g. attention, memory, reasoning, problem solving, decision-making) related to the processing of information and application of knowledge—have been widely examined usually by employing objective outcomes measures such as reaction time and accuracy. The effects of nutrition on subjective measures of psychological functions, such as self-reported mood, have received relatively less attention. The aim of this review is to provide a comprehensive overview of the theoretical frameworks that link subjective experience of mood to cognition and, from this understanding, identify the most promising methods to measure the individual experience of mood and its relationship to cognitive function. This will be illustrated with examples from studies that have examined the effects of nutritional interventions on cognitive performance and mood. However, the effects of nutritional manipulations are often subtle and inconsistently reported (e.g. Halyburton et al. [6]; Hellhammer et al. [7]; Rogers et al. [8]). Therefore, this review will also draw upon examples from the stress, cognition and mood literature, since stress induction [e.g. the use of sensory overload (excessive noise) or performing a task under social evaluation to provoke a psychophysiological stress response] is both robust and reliable in the provocation of mood change and moderation of cognitive function [9, 10]. Whilst stress response can be termed as any alteration to homoeostasis in an organism, for the purposes of this review, stress is defined as a mismatch between the demands of a task/context/stimuli and perceived ability to cope. If a context/stimuli is perceived as stressful, this will provoke a subjective response (e.g. negative affect/mood) and a physiological response (e.g. the release of the hormone cortisol to orchestrate the neuroendocrine response to stress). The main topics that will be addressed are: (1) how to best measure mental performance and mood, i.e. which measures are most reliable and validated under which conditions, (2) how placebo effects may affect subjective state and response to nutrient intervention, (3) the relationship between objective and subjective measures, (4) the ability to detect meaningful effects and elucidate their mechanism of action and (5) how nutrient effects on subjective experience, measured by standardised questionnaires, translate into everyday life and the clinical relevance of these. The proposed approach extends the traditional empirical approach of using solely standard “objective” measurements to also consider subjective state in a more integrated manner using advances in technology and appropriate analytical strategies. Such data on subjective experience may enrich our understanding and interpretation of objective measures and as such these recommendations are expected to help guide researchers from academia and industry when studying the effects that foods or specific product consumption can have on mood and mental performance.
Definition and measurement of subjective mood state
In behavioural sciences, measures of motor and cognitive behaviour (reaction time, number of words recalled) and physiological variables (salivary cortisol concentration, blood pressure, heart rate variability) are considered to be objective measures, in contrast to self-rating/self-reported measures of cognitive performance (e.g. participants’ self-rated perception of how accurately or quickly a task was performed) and mood, which are often referred to as subjective measures of an individual’s subjective experience. Mood can be described as a pervasive and predominant affective state and is commonly conceived to vary along orthogonal and bipolar dimensions of valence (positive vs negative) and arousal/activation (e.g. Russell [11]; Watson and Tellegen [12]). Mood can also be temporally separated into protracted (e.g. depressed mood) and transient, fluctuating affective states (e.g. a momentary state of increased vigour). As mood is inherently phenomenological, it is perceived as an inconsistent measure of the brain’s output, despite demonstrations that mood can be consistently measured. For example, specific drugs (e.g. Brown and Chandler [13]; Mula and Sander [14]) and stimuli (e.g. stress [15]) have been shown to have very consistent effects on mood, as measured by ratings on scales and questionnaires. In addition to well-being questionnaires, which often capture protracted, generalised affective mood states, there are several validated tools available to assess transient mood states which have been able to capture changes in mood as a result of a number of different nutritional interventions [16, 17]. For example, relative to placebo, a 30-day high-flavanol chocolate drink improved self-rated calmness and contentedness, measured by Bond–Lader mood scales [16] and the Profile of Mood States (POMS) captured changes in tension–anxiety scores following intervention with L-theanine under conditions of induced stress [17]. Table 1 provides examples of questionnaire/scale measures of subjective mood state and well-being and their potential suitability for nutritional interventions.
Moods can be linked to specific events, such as those caused by artificial mood inductions, but more commonly they occur somewhat independently of second-by-second, or minute-by-minute circumstances. Ecological momentary assessment (EMA) or experience sampling methods (ESM) are alternative mood measurement tools which may more realistically capture sequential, transient states by requiring brief inputs of mood state during daily activities. EMA data can be captured, for example, via mobile devices such as smart phones, where participants are periodically asked to fill in short questionnaires. Psychological research has established that recollected effect may diverge from actual experience because it is influenced by errors in recollection, recall biases, focusing illusions and salient memory heuristics [18]. This “memory–experience gap” between life as it is remembered and life as it is experienced may be important to the processes through which the past impacts on future behaviour. Moreover, effects resulting from interventions with nutrients may not be noticeable after acute administrations commonly applied in laboratory settings, but may give rise to improved well-being over time, especially if the intervention has other benefits such as cardiovascular health. One recent study, which endeavoured to measure daily fluctuations in mood via cell phone questionnaires, reported an effect of a multivitamin supplement on alertness after 4-week supplementation [19]. Others have validated cardiovascular biomarkers against the mood reports acquired during daily life. For instance, Steptoe and colleagues found that systolic blood pressure correlated with positive effect in men during work hours [20].
Validity of measures of subjective states
There are numerous types of validity, but in this context, the most important is construct validity—are we actually measuring what we think we are measuring? Evaluation of construct validity involves demonstrating that the measure correlates with variables that are known to be related to the construct (purportedly measured by the instrument being evaluated or for which there are theoretical grounds for expecting it to be related). Thus, identifying the “gold standard” against which to validate is crucial. Employing the stress induction model to illustrate this point, the seminal work of Seyle [21] explained that many stressors placed upon us have neutral effects until, by our own thinking, we appraise the experience as subjectively negative or positive. Thus, when measuring stress in individuals, it is important to acknowledge that a self-report of stress will need to be evaluated against the baseline of an individual (i.e. personality, past experience, as well as physiological state). This explains why different people may have profoundly different reactions to the same basic source of stress. In other words, it is one’s own perception that is crucial. However, both physiological and subjective mood responses to stress are relatively stable individual traits and can thus be accurately and consistently measured after exposure to stressful stimuli. For example, good correlations between subjective and physiological stress increases are shown in participants after the Trier Social Stress Test (TSST) [15]. Yet measurement of stress elicited by the TSST can be modulated by genetics, lifestyle, etc., and thus, validity of any subjective measurement will need to be evaluated in the context of these types of variables.
Contextual information is often missed when comparing measures; thus, validation of self-report with performance or physiological data must take into account large individual differences and also must control for as many external variables as possible. For example, measuring physical activity with objective (accelerometry) compared with self-report measures, not surprisingly produces very poor correlations [22] and is interpreted as reflecting recall bias inherent in self-report measures. However, an alternative explanation is that the two methods measure different things. Self-reports take into account the specific context, whereas accelerometry is a raw measure of movement. In summary, validity of subjective measures can be obtained via consistency of results after highly controlled stimuli such as the TSST and to some extent with physiological measures, when carefully controlled for “individual” factors.
Detection and interpretation of meaningful effects
A common problem in this field is how to interpret null effects. Detecting no effect on a measure of subjective state following a nutritional intervention could mean that the intervention really does not influence the mood parameter measured. Alternatively, it could reflect a lack of sensitivity of that measure to small or subtle changes in state or that the intervention prevented a degradation that would otherwise have been observed. An effect may also fail to be detected because of inadequate power which is also related to the magnitude of the experimental effect, or individual differences in the use of a scale which increase variability and decrease sensitivity of the measure [5]. Large inter- and intra-subject variability in subjective measures such as mood mean that larger sample sizes to detect the effects of a nutrient against this relatively noisy background may be required. Null or inconsistent effects may also be attributable to the use of insensitive experimental designs (e.g. between subjects) or inappropriate selection of baseline measures and the failure to include these in the statistical analysis. Two psychological measures of mood may claim to measure the same subjective state, but it may be that only one is sufficiently sensitive to detect effects of a nutritional manipulation. It is feasible that commonly employed measures may be inadequate to assess subjective state in relation to nutrient intervention and mask real effects. A lack of effect on some measures could be due to a subtle effect of a nutrient on only one component of the subjective state which when computed into a “scale score” is no longer detected. Many studies have simply administered “off the shelf” measures and report the factor scores or summed items based on previous validation studies or factor analyses which are not based on the same populations in the same state, e.g. following a nutrition intervention.
Appropriate analyses of data from studies where subjective state is the outcome variable pose some unique problems. Even where participants can be randomised to nutrient or placebo interventions, it cannot be assumed that baseline measures will not differ and hence change from baseline or inclusion of baseline as a covariate is the recommended statistical approach. In these randomised studies, both analysis of variance (ANOVA) on change from baseline and analysis of covariance (ANCOVA) with baseline as a covariate will be unbiased [23]. In non-randomised studies where baseline differences may pre-exist and samples may be more heterogeneous, both methods may contradict each other since neither can be unbiased. True randomisation is therefore the preferred approach. Moreover, the overuse and over-interpretation of subgroup analyses poses further problems in this field [24], as does the splitting of samples using median splits [21] since these may exaggerate or even produce effects which are actually artefacts of the reduction of a continuous variable such as mood to a categorical group.
Expectancy and placebo effects
Placebo effects are a concern for all scientific research and well-designed clinical studies go to great lengths to avoid potential bias introduced by these effects by “blinding”. However, via expectations, placebos influence a variety of outcome measures including physiological responses. Despite continuing efforts to fully understand the psychological mechanisms of placebo effects, it is well recognised that expectation is a major contributor to study outcomes in response to treatment in intervention studies [25]. Expectancy effects can be described as changes in behaviour that occur in an experiment due to the anticipation of results that unconsciously affect the outcome. The observation that these effects may be one of the main mechanisms that underlie the placebo effect has been supported by neuroimaging studies which have shown that the placebo response is associated with widespread frontal and prefrontal activation which is consistent with the processing of expectation and executive function [26]. Most of our knowledge about placebo mechanisms comes from investigations of placebo effects in the domain of pain [27] where patients have repeatedly experienced significant pain relief from placebos when the placebo is described as an analgesic medication compared to when it is not [28]. This is an example of a verbal cue that can create a strong expectancy effect which results in behavioural, clinical or physiological changes [29]. Another example of this is where caffeine-associated stimuli such as the smell and taste of coffee have been shown to elicit both self-reported and physiological arousal [30] and where the expectation of having consumed caffeine can result in improvements in cognitive performance and mood [18]. In this particular study, participants were randomly allocated to both a drink (caffeinated coffee vs. decaffeinated coffee) and an expectancy (told caffeine vs. told decaffeinated) condition. Both caffeine and expectation of having consumed caffeine improved attention and psychomotor speed.
There are many other factors which influence expectation including previous experience of the intervention, knowledge of others’ accounts, influences such as the researcher and non-verbal and sensory cues such as the label of the product and the taste. For instance, Rogers et al. [31] showed that when energy drinks were labelled “energy drink” rather than “healthy and nutritious”, both the expected energy from the drink and the expectation of better performance on cognitive tasks were significantly greater. In this study, taste also resulted in expectation of better performance on the task; however, these expectancies did not carry through to influence actual performance, which is contradictory to Green et al.’s study [32]. They did find that expectancy effects were able to influence performance on a cognitive task. Green et al. [32] gave study participants either glucose or aspartame on two occasions in a counterbalanced manner. On one occasion, for each treatment, participants were misinformed about the treatment they were going to receive (glucose or aspartame). Improvements in the Bakan vigilance task were observed after glucose consumption, but only when participants were told they were going to receive glucose. No task improvements were observed when participants thought that they were consuming aspartame. Similar effects were observed by Stollery and Christian [33] who found a subtle improvement in a task of delayed free recall when participants believed they had consumed glucose. Whilst the authors concluded that the expectancy effects were small and unlikely to be confused with glucose enhancements, they did suggest that routine collection of product beliefs should be carried out in future studies. This is particularly important when testing commercial products, on potential consumers. Whilst typically substantial effort is invested to control for placebo effects (by having a placebo), expectancy effects are also important for subjective and objective state post-ingestion. Moreover, it is these effects reinforced by repeated exposure which will guide consumers into making a decision to purchase a product. Hence, expectancy effects also need to be measured in studies of nutrient interventions. These observations also emphasise the importance of an appropriate, well-matched placebo, particularly in experiments where the product could easily be recognised by the consumer, and post-study debriefing may be useful to assess the effectiveness of blinding of the treatment conditions (although this is rarely reported in published studies). It should also be noted that use of objective measures will not cancel or even ameliorate placebo effects. Thus, the expectancy of the study participants is an important factor in the design of nutritional intervention studies.
Relationships between subjective and objective mental performance measures
Whilst mood states are subjective in the sense that they occur in a person’s experience, manifestations of mood can also be observed objectively in physical actions, cognition and behaviour. Mood-influenced cognition is most often studied in patients with depression or those who have recovered from depression. In such studies, depression has been shown to correlate with worse performance in attention and memory tasks. The definition of clinical depression is defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM V) as a “depressed mood or a loss of interest or pleasure in daily activities for more than 2 weeks, where mood represents a change from the person’s baseline”. This rather qualitative definition is made quantitative in clinical intervention studies by establishment of threshold scores in depression checklists or questionnaires (such as the Beck Depression Inventory) which measure particular levels of impaired function in social, occupational and educational settings. Due to the concrete criteria of clinical depression, comparison of depressed vs healthy participant behaviour is a useful approach for understanding mood–cognition interactions. For instance, depressed study participants demonstrate attentional negative bias towards stimuli such as words or facial expressions as compared to non-depressed participants [34] and show a slowing down of response times compared to non-depressed participants. Interestingly, researchers have shown that participants with familial history of depression, but with no prior diagnosis of depression, also exhibit attentional bias towards negative stimuli that is greater than that of participants with no familial history of depression. These “emotional bias” cognition tests have been proposed as an early detection method to identify participants with a predisposition to depression. Similarly, functional magnetic resonance imaging (fMRI) measurements of amygdala reactivity to negative stimuli appear to be greater in participants with family history of depression or carriers of putative “depression genes” such as the 5-HTTLPR short alleles or met MAO alleles [35].
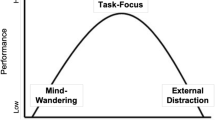
With respect to healthy participants, the negative effect of poor mood on cognition has been demonstrated with similar paradigms. For example, after a stress induction to provoke negative mood, participants exhibit stronger reactions to negative stimuli reflected by altered reaction times or decision-making [36]. Poor mood has also been shown to affect attentional biases towards punishment-associated stimuli, as manifested by faster reaction time towards such stimuli. Impaired cognitive processing due to mood has also been observed via poorer performance on effortful versus automatic visual tasks in depressed subjects [37]. The above examples describe several areas where mood has an immediate effect on cognition; however, we also need to consider the direct effects of nutrients on mood and cognition and how they may not be measurable at the same time. Consideration needs to be given to the fact that there may be a temporal lag between ingestion of a nutrient and its effect on mood and cognition. For example, improvements in mood may have a motivating effect on subsequent cognitive performance. It is highly likely that effects of nutrients or dietary supplements on mood and cognition occur within different time frames and even at different doses of the nutrient and as such effects may be missed if subjective and objective measures are not considered concomitantly and independently. For example in an acute study by Scholey et al. [19], cognitive performance and self-reported mental fatigue were measured after two doses of cocoa flavanols. Both doses improved performance on the Serial Threes task, whilst only the low dose improved mood. In addition, the high acute dose improved response times in a Rapid Visual Information Processing Task (RVIP) but showed no effects on mood. It is plausible that the effects of a nutrient on subjective state in the longer term may produce acute changes in cognition or that such changes are not related temporally. Hence, it is advisable to consider acute on chronic studies and more frequent assessments to ensure that these effects and the relationships between acute and chronic effects in both subjective and objective outcomes are captured.
Linking subjective states to mechanisms of action
Demonstration of biological plausibility is crucial when linking the effects of specific nutrients to subjective mood states; however, there is a paucity of studies which have attempted to link these two types of outcome within the same study. We will use the example of n − 3 PUFA to describe potential mechanisms. Animals fed a diet containing low levels of n − 3 PUFA display impaired emotional and cognitive behaviour [38–47]. Metabolism of monoamines [48], neuronal plasticity [49], neuroinflammation [50, 51] and stress response [52] are impaired in the brains of these animals. In humans, an impaired stress response has been repeatedly associated with low n − 3 PUFA [44, 53–57]. Promising data obtained in humans and animal models show that docosahexaenoic acid (DHA) dietary supplementation lowers self-reported cognitive (e.g. feeling unease and fear) and physiological (e.g. sweating) anxiety symptoms [58], cortisol response to mental stress [55, 59] and to inflammatory stimuli [60], and peripheral and brain inflammation, especially in healthy older adults [50, 61–65]. The activity of proinflammatory cytokines in the brain are involved in the development of somatic symptoms (fatigue, attention, etc.) known to alter mental performance and mood as described above [66–68]. To conclude, preclinical studies have highlighted plausible biological mechanisms relating to neurobiological systems involved in mood and cognitive disorders, possibly underlying the effects of various nutrients on subjective mood state.
Recommendations and conclusions
In this paper, we argue that the subjective effects of foods on self-reported mood and cognition can enrich our understanding and interpretation of gold-standard “objective outcome measures” (cognitive test outcomes, e.g. reaction times, the number of words recalled and physiological markers, e.g. salivary cortisol concentrations) and should be considered both concomitantly and independently. Thus, we make the case that measures of subjective states are a valid and appropriate methodology for assessing the effects of nutritional intake on mood and mental performance. The proposed approach extends the traditional cognitive approach of using standard “objective” performance measurements to also include consumers’ subjective experiences in relation to food. Our specific recommendations are as follows:
-
Consideration of both traditional mood questionnaires or the use of ecological momentary assessment (EMA) or experience sampling methods (ESM), which may more realistically capture transient mood states. Identifying which are best and most reliable under which condition.
-
Use measures sufficiently sensitive to detect effects of a nutritional manipulation and to evaluate the magnitude and meaningfulness of changes demonstrated, e.g. by comparison with effects induced by drugs or alcohol or variations in mood which occur over the course of a day.
-
Consider the possibility that subjective and objective measures will occur within different time frames and in response to different doses. Acute on chronic studies may help capture transient effects on mood or cognitive function which may result in longer-term measureable benefits.
-
Recognition of the importance of expectancy and placebo effects when measuring subjective mood states and behaviour generally and selection of well-matched placebos.
-
Demonstrating biological plausibility is crucial when linking the effects of specific nutrients to subjective mood states and behaviour.
Abbreviations
- ANCOVA:
-
Analysis of covariance
- ANOVA:
-
Analysis of variance
- DHA:
-
Docosahexaenoic acid
- EMA:
-
Ecological momentary assessment
- ESM:
-
Experience sampling methods
- fMRI:
-
Functional magnetic resonance imaging
- POMS:
-
Profile of mood states
- PUFA:
-
Polyunsaturated fatty acid
- RVIP:
-
Rapid visual information processing
- TSST:
-
Trier social stress test
References
Anderson JW, Johnstone BM, Remley DT (1999) Breast-feeding and cognitive development: a meta-analysis. Am J Clin Nutr 70:525–535
Singh B, Parsaik AK, Mielke MM, Erwin PJ, Knopman DS, Petersen RC, Roberts RO (2014) Association of Mediterranean diet with mild cognitive impairment and Alzheimer’s disease: a systematic review and meta-analysis. J Alzheimers Dis 39:271
Ordovas JM (2015) Genetics of brain and cognition and their interactions with dietary and environmental factors. In: Best T, Dye L (eds) Nutrition for brain health and cognitive performance, 1st edn. CRC Press, Boca Rotan, pp 41–74
Gómez-Pinilla F (2008) Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci 9:568–578
de Jager CA, Dye L, de Bruin EA, Butler L, Fletcher J, Lamport DJ, Latulippe ME, Spencer JP, Wesnes K (2014) Criteria for validation and selection of cognitive tests for investigating the effects of foods and nutrients. Nutr Rev 72:162–179
Halyburton AK, Brinkworth GD, Wilson CJ, Noakes M, Buckley JD, Keogh JB, Clifton PM (2007) Low-and high-carbohydrate weight-loss diets have similar effects on mood but not cognitive performance. Am J Clin Nutr 86:580–587
Hellhammer J, Waladkhani AR, Hero T, Buss C (2010) Effects of milk phospholipid on memory and psychological stress response. Br Food J 112:1124–1137
Rogers PJ, Appleton KM, Kessler D, Peters TJ, Gunnell D, Hayward RC, Heatherley SV, Christian LM, McNaughton SA, Ness AR (2008) No effect of n − 3 long-chain polyunsaturated fatty acid (EPA and DHA) supplementation on depressed mood and cognitive function: a randomised controlled trial. Br J Nutr 99:421–431
Lupien SJ, Maheu F, Tu M, Fiocco A, Schramek TE (2007) The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition. Brain Cogn 65:209–237
Lupien SJ, McEwen BS, Gunnar MR, Heim C (2009) Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 10:434–445
Russell JA (1980) A circumplex model of affect. J Pers Soc Psychol 39:1161
Watson D, Tellegen A (1985) Toward a consensual structure of mood. Psychol Bull 98:219
Brown ES, Chandler PA (2001) Mood and cognitive changes during systemic corticosteroid therapy. Prim Care Companion J Clin Psychiatry 3:17
Mula M, Sander JW (2007) Negative effects of antiepileptic drugs on mood in patients with epilepsy. Drug Saf 30:555–567
Campbell J, Ehlert U (2012) Acute psychosocial stress: does the emotional stress response correspond with physiological responses? Psychoneuroendocrinology 37:1111–1134
Pase MP, Scholey AB, Pipingas A, Kras M, Nolidin K, Gibbs A, Wesnes K, Stough C (2013) Cocoa polyphenols enhance positive mood states but not cognitive performance: a randomized, placebo-controlled trial. J Psychopharmacol 27:451–458
Yoto A, Motoki M, Murao S, Yokogoshi H (2012) Effects of L-theanine or caffeine intake on changes in blood pressure under physical and psychological stresses. J Physiol Anthropol 31:28
Dawkins L, Shahzad FZ, Ahmed SS, Edmonds CJ (2011) Expectation of having consumed caffeine can improve performance and mood. Appetite 57:597–600
Scholey AB, French SJ, Morris PJ, Kennedy DO, Milne AL, Haskell CF (2010) Consumption of cocoa flavanols results in acute improvements in mood and cognitive performance during sustained mental effort. J Psychopharmacol 24:1505–1514
Steptoe A, Wardle J, Marmot M (2005) Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc Natl Acad Sci USA 102:6508–6512
Selye H (1936) Thymus and adrenals in the response of the organism to injuries and intoxications. Br J Exp Pathol 17:234
Hamer M, Kivimaki M, Steptoe A (2012) Longitudinal patterns in physical activity and sedentary behaviour from mid-life to early old age: a substudy of the Whitehall II cohort. J Epidemiol Community Health 66:1110–1115
Van Breukelen GJ (2006) ANCOVA versus change from baseline had more power in randomized studies and more bias in nonrandomized studies. J Clin Epidemiol 59:920–925
Pocock SJ, Assmann SE, Enos LE, Kasten LE (2002) Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Stat Med 21:2917–2930
Finniss DG, Kaptchuk TJ, Miller F, Benedetti F (2010) Biological, clinical, and ethical advances of placebo effects. Lancet 375:686–695
Benedetti F, Mayberg HS, Wager TD, Stohler CS, Zubieta JK (2005) Neurobiological mechanisms of the placebo effect. J Neurosci 25:10390–10402
Colloca L, Benedetti F (2005) Placebos and painkillers: is mind as real as matter? Nat Rev Neurol 6:545–552
Wager TD, Atlas LY, Leotti LA, Rilling JK (2011) Predicting individual differences in placebo analgesia: contributions of brain activity during anticipation and pain experience. J Neurosci 31:439–452
Co Colloca L, Miller FG (2011) How placebo responses are formed: a learning perspective. Philos Trans Roy Soc B 366:1859–1869
Flaten MA, Blumenthal TD (1999) Caffeine-associated stimuli elicit conditioned responses: an experimental model of the placebo effect. Psychopharmacology 145:105–112
Rogers PJ, Law J, Sanderson C (2012) Modelling the psychostimulant effects of an energy drink. Label and taste influence expectations, but only caffeine delivers. Appetite 59:634
Green Green MW, Taylor MA, Elliman NA, Rhodes O (2001) Placebo expectancy effects in the relationship between glucose and cognition. Br J Nutr 86:173–179
Stollery B, Christian L (2013) Glucose and memory: the influence of drink, expectancy, and beliefs. Psychopharmacology 228:685–697
Murrough JW, Iacoviello B, Neumeister A, Charney DS, Iosifescu DV (2011) Cognitive dysfunction in depression: neurocircuitry and new therapeutic strategies. Neurobiol Learn Mem 96:553–563
Roiser JP, Sahakian BJ (2013) Hot and cold cognition in depression. CNS Spectr 18:139–149
Hockey GR, John Maule A, Clough PJ, Bdzola L (2000) Effects of negative mood states on risk in everyday decision making. Cognition Emotion 14:823–855
Hammar A, Lund A, Hugdahl K (2003) Long-lasting cognitive impairment in unipolar major depression: a 6-month follow-up study. Psychiat Res 118:189–196
DeMar JC, Ma K, Bell JM, Igarashi M, Greenstein D, Rapoport SI (2006) One generation of n − 3 polyunsaturated fatty acid deprivation increases depression and aggression test scores in rats. J Lipid Res 47:172–180
Fedorova I, Hussein N, Baumann MH, Di Martino C, Salem N Jr (2009) An n − 3 fatty acid deficiency impairs rat spatial learning in the Barnes maze. Behav Neurosci 123:196
Francès H, Coudereau JP, Sandouk P, Clément M, Monier C, Bourre JM (1996) Influence of a dietary α-linolenic acid deficiency on learning in the Morris water maze and on the effects of morphine. Eur J Pharmacol 298:217–225
Lafourcade M, Larrieu T, Mato S, Duffaud A, Sepers M, Matias I, De Smedt-Peyrusse V, Labrousse VF, Bretillon L, Matute C (2011) Nutritional omega-3 deficiency abolishes endocannabinoid-mediated neuronal functions. Nat Neurosci 14:345–350
Larrieu T, Madore C, Joffre C, Layé S (2012) Nutritional n − 3 polyunsaturated fatty acids deficiency alters cannabinoid receptor signaling pathway in the brain and associated anxiety-like behavior in mice. J Physiol Biochem 68:671–681
Levant B, Radel JD, Carlson SE (2006) Reduced brain DHA content after a single reproductive cycle in female rats fed a diet deficient in N − 3 polyunsaturated fatty acids. Biol Psychiat 60:987–990
McNamara RK, Jandacek R, Rider T, Tso P, Cole-Strauss A, Lipton JW (2010) Omega-3 fatty acid deficiency increases constitutive pro-inflammatory cytokine production in rats: relationship with central serotonin turnover. Prostag Leukotr Ess 83:185–191
Moranis A, Delpech JC, De Smedt-Peyrusse V, Aubert A, Guesnet P, Lavialle M, Joffre C, Layé S (2012) Long term adequate n − 3 polyunsaturated fatty acid diet protects from depressive-like behavior but not from working memory disruption and brain cytokine expression in aged mice. Brain Behav Immun 26:721–731
Rao JS, Ertley RN, Lee HJ, DeMar JC, Arnold JT, Rapoport SI, Bazinet RP (2007) n − 3 polyunsaturated fatty acid deprivation in rats decreases frontal cortex BDNF via a p38 MAPK-dependent mechanism. Mol Psychiatry 12:36–46
Vancassel S, Aïd S, Pifferi F, Morice E, Nosten-Bertrand M, Chalon S, Lavialle M (2005) Cerebral asymmetry and behavioral lateralization in rats chronically lacking n − 3 polyunsaturated fatty acids. Biol Psychiatry 58:805–811
Chalon S (2006) Omega-3 fatty acids and monoamine neurotransmission. Prostag Leukotr Ess 75:259–269
Zainuddin MSA, Thuret S (2012) Nutrition, adult hippocampal neurogenesis and mental health. Br Med Bull 103:89–114
Layé S (2010) Polyunsaturated fatty acids, neuroinflammation and well being. Prostag Leukotr Ess 82:295–303
Mingam R, Moranis A, Bluthé R-M, De Smedt-Peyrusse V, Kelley KW, Guesnet P, Lavialle M, Dantzer R, Layé S (2008) Uncoupling of interleukin-6 from its signalling pathway by dietary n − 3-polyunsaturated fatty acid deprivation alters sickness behaviour in mice. Eur J Neurosci 28:1877–1886
Denis I, Potier B, Vancassel S, Heberden C, Lavialle M (2013) Omega-3 fatty acids and brain resistance to ageing and stress: body of evidence and possible mechanisms. Ageing Res Rev 12:579–594
Lin PY, Huang SY, Su KP (2010) A meta-analytic review of polyunsaturated fatty acid compositions in patients with depression. Biol Psychiat 68:140–147
Mocking RJ, Assies J, Bot M, Jansen EH, Schene AH, Pouwer F (2012) Biological effects of add-on eicosapentaenoic acid supplementation in diabetes mellitus and co-morbid depression: a randomized controlled trial. PLoS one 7:e49431
Assies J, Pouwer F, Lok A, Mocking RJ, Bockting CL, Visser I, Abeling NG, Duran M, Schene AH (2010) Plasma and erythrocyte fatty acid patterns in patients with recurrent depression: a matched case-control study. PLoS one 5:e10635
Laugero KD, Smilowitz JT, German JB, Jarcho MR, Mendoza SP, Bales KL (2011) Plasma omega 3 polyunsaturated fatty acid status and monounsaturated fatty acids are altered by chronic social stress and predict endocrine responses to acute stress in titi monkeys. Prostag Leukotr Ess 84:71–78
Mocking RJ, Ruhé HG, Assies J, Lok A, Koeter MW, Visser I, Bockting CL, Schene AH (2013) Relationship between the hypothalamic-pituitary-adrenal-axis and fatty acid metabolism in recurrent depression. Psychoneuroendocrinology 38:1607–1617
Kiecolt-Glaser JK, Belury MA, Andridge R, Malarkey WB, Glaser R (2011) Omega-3 supplementation lowers inflammation and anxiety in medical students: a randomized controlled trial. Brain Behav Immun 25:1725–1734
Delarue JOCP, Matzinger O, Binnert C, Schneiter P, Chiolero R, Tappy L (2003) Fish oil prevents the adrenal activation elicited by mental stress in healthy men. Diabetes Metab 29:289–295
Orr SK, Palumbo S, Bosetti F, Mount HT, Kang JX, Greenwood CE, Ma DW, Serhan CN, Bazinet RP (2013) Unesterified docosahexaenoic acid is protective in neuroinflammation. J Neurochem 127:378–393
Farzaneh-Far R, Harris WS, Garg S, Na B, Whooley MA (2009) Inverse association of erythrocyte n − 3 fatty acid levels with inflammatory biomarkers in patients with stable coronary artery disease: the Heart and Soul Study. Atherosclerosis 205:538–543
Ferrucci L, Cherubini A, Bandinelli S, Bartali B, Corsi A, Lauretani F, Martin A, Andres-Lacueva C, Senin U, Guralnik JM (2006) Relationship of plasma polyunsaturated fatty acids to circulating inflammatory markers. J Clin Endocrinol Metab 91:439–446
Kalogeropoulos N, Panagiotakos DB, Pitsavos C, Chrysohoou C, Rousinou G, Toutouza M, Stefanadis C (2010) Unsaturated fatty acids are inversely associated and n − 6/n − 3 ratios are positively related to inflammation and coagulation markers in plasma of apparently healthy adults. Clin Chim Acta 411:584–591
Kiecolt-Glaser JK, Belury MA, Porter K, Beversdorf D, Lemeshow S, Glaser R (2007) Depressive symptoms, n − 6: n − 3 fatty acids, and inflammation in older adults. Psychosom Med 69:217–224
Labrousse VF, Nadjar A, Joffre C, Costes L, Aubert A, Gregoire S, Bretillon L, Laye S (2012) Short-term long chain omega3 diet protects from neuroinflammatory processes and memory impairment in aged mice. PLoS one 7:e36861
Capuron L, Miller AH (2011) Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther 130:226–238
Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW (2008) From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurol 9:46–56
Dantzer R, Heijnen CJ, Kavelaars A, Laye S, Capuron L (2014) The neuroimmune basis of fatigue. Trends Neurosci 37:39–46
Bond A, Lader M (1974) The use of analogue scales in rating subjective feelings. Br J Med Psychol 47:211–218
Armitage CJ, Conner M, Norman P (1999) Differential effects of mood on information processing: evidence from the theories of reasoned action and planned behaviour. Eur J Soc Psychol 29:419–433
Watson D, Clark LA (1999) The PANAS-X: manual for the positive and negative affect schedule-expanded form. University of Iowa Press, Iowa City
McNair DM, Lorr M, Droppleman LF (1971) EITS manual for the profile of mood states. Educational and Industrial Testing Service, San Diego
Norcross JC, Guadagnoli E, Prochaska JO (1984) Factor structure of the profile of mood states (POMS): two partial replications. J Clin Psychol 40:1270–1277
Nyenhuis DL, Yamamoto C, Luchetta T, Terrien A, Parmentier A (1999) Adult and geriatric normative data and validation of the profile of mood states. J Clin Psychol 55:79–86
WHOQOL group (1995) The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 41:1403–1409
Skevington SM, Lotfy M, O’Connell KA (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 13:299–310
Diener ED, Emmons RA, Larsen RJ, Griffin S (1985) The satisfaction with life scale. J Pers Assess 49:71–75
Lyubomirsky S, Lepper HS (1999) A measure of subjective happiness: preliminary reliability and construct validation. Soc Indic Res 46:137–155
Goldberg DP (1972) The detection of psychiatric illness by questionnaire: a technique for the identification and assessment of non-psychotic psychiatric illness. Oxford University Press, London
Carvalho HWd, Patrick CJ, Jorge MR, SrB Andreoli (2011) Validation of the structural coherency of the General Health Questionnaire. Rev Bras Psiquiatria 33:59–63
Dale B, Sævareid HI, Söderhamn O (2009) Testing and using Goldberg’s General Health Questionnaire: mental health in relation to home nursing, home help, and family care among older, care-dependent individuals. Int J Ment Health Nurs 18:133–143
Montazeri A, Harirchi AM, Shariati M, Garmaroudi G, Ebadi M, Fateh A (2003) The 12-item General Health Questionnaire (GHQ-12): translation and validation study of the Iranian version. Health Qual Life Outcomes 1:66
Acknowledgments
This work was conducted by an expert group of the International Life Sciences Institute, Europe (ILSI Europe). The expert group received funding from the ILSI Europe Nutrition and Mental Performance Task Force. Industry members of this task force are listed on the ILSI Europe Web site at www.ilsi.eu. For further information about ILSI Europe, please email info@ilsieurope.be or call +32 2 771 00 14. The opinions expressed herein and the conclusions of this publication are those of the authors and do not necessarily represent the views of ILSI Europe nor those of its member companies.
Author’s contribution
M. Hamer, L. Dye, E. Siobhan Mitchell, S. Layé, C. Saunders, N. Boyle and J. Sijben contributed to the conceptualisation and writing of the manuscript. J. Schuermans coordinated the work of the group and assisted with writing, condensing and formatting the draft.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Saunders is a full-time employee of PepsiCo Inc. J. Sijben is a full-time employee of Nutricia Research. E. Siobhan Mitchell is a full-time employee of Nestlé Institute of Health Sciences. S. Layé, E. Siobhan Mitchell and J. Schuermans have no competing interests. M. Hamer has received funding from industry for research on physical activity and well-being. L. Dye and N. Boyle have received funding from various food companies for contract research on the effects of food on cognitive function and mood.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hamer, M., Dye, L., Siobhan Mitchell, E. et al. Examining techniques for measuring the effects of nutrients on mental performance and mood state. Eur J Nutr 55, 1991–2000 (2016). https://doi.org/10.1007/s00394-015-1143-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-1143-3