Abstract
Purpose
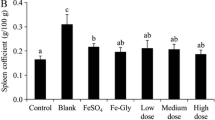
The effects of orally administered β-lactoglobulin hydrolysate-iron complex (β-LGH-Fe) on haematological and biochemical parameters in anaemic rats were evaluated. Female weaning Sprague–Dawley rats were fed with iron-deficient diet to induce iron deficiency anaemia. After 6 weeks, the obtained anaemic rats were divided into five groups: iron deficiency control group (iron-deficient diet without β-LGH-Fe complex supplementation, IDC); three groups supplemented with different dosages of β-LGH-Fe complex (0.5 mg Fe/kg BW, iron-deficient diet with low β-LGH-Fe, IDLFe; 2.0 mg Fe/kg BW, iron-deficient diet with medium β-LGH-Fe, IDMF; 4.0 mg Fe/kg BW, iron-deficient diet with high β-LGH-Fe, IDHFe); and ferrous sulphate-supplemented group at a dosage of 2.0 mg Fe/kg BW.
Results
β-LGH-Fe complex could significantly improve hematocrit and haemoglobin decrease, and normalise the serum iron level, total iron-binding capacity and transferrin saturation of anaemic rats in a dose-dependent manner. Serum ferritin content and hepatic nonheme iron level were also increased. In addition, the antioxidant enzyme activities of superoxidase dismutase, catalase and glutathione peroxidase in both plasma and liver homogenate were improved. The production of malondialdehyde and pro-inflammatory cytokines (TNF-α and IL-6) decreased.
Conclusions
It suggests that β-LGH-Fe complex can ameliorate iron deficiency anaemia, which might make it a potential ingredient with anti-anaemia activity.





Similar content being viewed by others
Abbreviations
- CTA:
-
Catalase
- Hb:
-
Haemoglobin
- HTC:
-
Haematocrit
- IDA:
-
Iron deficiency anaemia
- IL-6:
-
Interleukin-6
- GSH-Px:
-
Glutathione peroxidase
- MDA:
-
Malondialdehyde
- SOD:
-
Superoxidase dismutase
- TNF-α:
-
Tumour necrosis factor α
- TS:
-
Transferrin saturation
References
Andango PE, Osendarp SJ, Ayah R, West CE, Mwaniki DL, De Wolf CA, Kraaijenhagen R, Kok FJ, Verhoef H (2007) Efficacy of iron fortified whole maize flour on iron status of school children in Kenya: a randomized controlled trail. Lancet 369:1799–1806
Leung AKC, Chan KW (2001) Fe deficiency anemia. Adv Pediatr 48:385–408
Beard JL (2001) Iron biology in immune function, muscle metabolism and neuronal functioning. J Nutr 131:568S–580S
Schumann K, Ettle T, Szegner B, Elsenhans B, Solomons NW (2007) On risks and benefits of iron supplementation recommendations for iron intake revisited. J Trace Elem Med Biol 21:47–68
Dewey KG, Domellof M, Cohen RJ, Landa Rivera L, Hernell O, Lönnerdal B (2002) Iron supplementation affects growth and morbidity of breast-fed infants: results of a randomized trial in Sweden and Honduras. J Nutr 132:3249–3255
Hyder SM, Persson LA, Chowdhury AMR, Ekstrom EC (2002) Do side-effects reduce compliance to iron supplementation? A study of daily and weekly-dose regimens in pregnancy. J Health Popul Nutr 20:175–179
Martins EAL, Robalinho RL, Meneghini R (1995) Oxidative stress induces activation of a cytosolic protein responsible for control of iron uptake. Arch Biochem Biophys 316:128–134
Ballot DE, MacPhail AP, Bothwell TH, Gillooly M, Mayet FG (1989) Fortification of curry powder with NaFe(III)EDTA in an iron deficient population. Report of a controlled iron-fortification trial. Am J Clin Nutr 49:162–169
Hurrell R (2002) How to ensure adequate iron absorption from iron-fortified food. Nutr Rev 60:7–15
Chaud MV, Izumi C, Nahaal Z, Shuhama T, Bianchi Mde L, de Freitas O (2002) Iron derivatives from casein hydrolysates as a potential source in the treatment of iron deficiency. J Agric Food Chem 50:871–877
Miquel E, Farre R (2007) Effects and future trends of casein phosphopeptides on zinc bioavailability. Trends Food Sci Technol 18:139–143
Ani-Kibangou B, Bouhallab S, Molle D (2005) Improved absorption of caseinophosphopeptide-bound iron: role of alkaline phosphatase. J Nutr Biochem 16:398–401
Nakano T, Goto T, Nakaji T, Aoki T (2007) Bioavailability of iron-fortified whey protein concentrate in iron-deficient rats. Asian Aust J Anim Sci 20:1120–1126
Argyri K, Miller DD, Glahn RP, Zhu L, Kapsokefalou M (2007) Peptides isolated from in vitro digests of milk enhance iron uptake by Caco-2 cells. J Agric Food Chem 55:10221–10225
Aït-Oukhatar N, Bouhallab S, Arhan P, Maubois JL, Drosdowsky M, Bouglé D (1999) Iron tissue storage and hemoglobin levels of deficient rats repleted with iron bound to the caseinophophopeptides 1–25 of β-casein. J Agric Food Chem 47:2786–2790
Aït-Oukhatar N, Bouhallab S, Bureau F, Arhan P, Maubois JL, Bouglé DL (2000) In vitro digestion of caseinophosphopeptide-iron complex. J Dairy Res 67:125–129
Aït-Oukhatar N, Bouhallab S, Bureau F, Arhan P, Maubois JL, Drosdowsky MA, Bouglé DL (1997) Bioavailability of caseinophosphopeptide bound iron in the young rat. J Nutr Biochem 8:190–194
Vegarud GE, Langsrud T, Svenning C (2000) Mineral-binding milk proteins and peptides; occurrence, biochemical and technological characteristics. Brit J Nutr 84:S91–S98
Kim SB, Seo IS, Khan MA, Ki KS, Nam MS, Kim HS (2007) Separation of iron-binding protein from whey through enzymatic hydrolysis. Int Dairy J 17:625–631
Maes W, Van Camp J, Vermeirssen V, Hemeryck M, Ketelslegers JM, Schrezenmeir J, Van Oosteveldt P, Huyghebaert A (2004) Influence of the lactokinin Ala-Leu-Pro-Met-His-Ile-Arg (ALPMHIR) on the release of endothelin-1 by endothelial cells. Regul Peptides 118:105–109
Yamauchi R, Usui H, Yunden J, Takenaka Y, Tani F, Yoshikawa M (2003) Characterization of beta-lactoglobulin, a bioactive peptide derived from bovine beta-lactoglobulin, as a neurotensin agonist. Biosci Biotechnol Biochem 67:940–943
Zhou J, Wang X, Ai T, Cheng X, Guo HY, Teng GX, Mao XY (2012) Preparation and characterization of β-lactoglobulin hydrolysate-iron complexes. J Dairy Sci 95:4230–4236
National Research Council (1985) Guide for the care and use of laboratory animals. NIH publication no. 85. Bethesda: National Institutes of Health, pp 23
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Zhu L, Glahn RP, Nelson D, Miller DD (2009) Comparing soluble ferric pyrophosphate to common iron salts and chelates as sources of bioavailable iron in a Caco-2 cell culture model. J Agric Food Chem 57:5014–5019
da Conceicao EC, Shuhama T, Izumi C, de Freitas O (2001) Iron supplementation prevents the development of iron deficiency in rats with omeprazole-induced hypochlorhydria. Nutr Res 21:1201–1208
Haro-Vicente JF, Pérez-Conesa D, Rincón F, Ros G, Martínez-Graciá C, Vidal ML (2008) Does ascorbic acid supplementation affect iron bioavailability in rats fed micronized dispersible ferric pyrophosphate fortified fruit juice? Eur J Nutr 47:470–478
Thomas CE, Gaffney-Stomberg E, Sun BH, O’Brien KO, Kerstetter JE, Insogna KL (2013) Increasing dietary protein acutely augments intestinal iron transporter expression and significantly increases iron absorption in rats. FASEB J 2:2476–2483
Yasuda K, Dawson HD, Wasmuth EV, Roneker CA, Chen C, Urban JF, Welch RM, Miller DD, Lei XG (2009) Supplemental dietary inulin influences expression of iron and inflammation related genes in young pigs. J Nutr 139:2018–2023
Acknowledgments
We are grateful for the financial support of this work by the National Natural Science Foundation of China (Beijing, China; Grant No. 30972291) and Beijing Natural Science Foundation (Beijing, China; Grant No. 5102021). J. Z. and X. Y. M. worked on preparing the project design, data analysis, final revision and submission of manuscript. J. Z., T. A. and J. J. M. conducted the experiment with the animals and performed the laboratorial analysis. J. Z. and X. W. performed the statistical analysis. None of the authors had any conflict of interest related to their participation in this study. All authors have read and approved the final manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, J., Mao, XY., Wang, X. et al. Anti-anaemia efficacy of β-lactoglobulin hydrolysate-iron complex on iron-deficient anaemic rats. Eur J Nutr 53, 877–884 (2014). https://doi.org/10.1007/s00394-013-0591-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-013-0591-x