Abstract
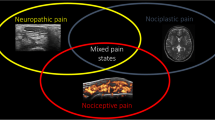
Rheumatic diseases are characterized by chronic inflammation of synovial joints and are often associated with persistent pain and increased pain sensitivity. The inflammatory process is a complex cascade of events involving several mediators, which can lead to a chronic condition of pain. Inflammation can stimulate angiogenesis, and angiogenesis can facilitate inflammation. Inflammatory pain arises from tissue damage via the sensitization of pain receptors (nociceptors). The main peripheral mechanism underlying nociceptive pain is a change in the activity of the nociceptors located in the affected anatomical structures (joints, tendons, and ligaments), which renders them more sensitive to normally painful stimuli (hyperalgesia) or normally non-painful stimuli (allodynia). Neuroimmune interaction has been considered to play an essential role in rheumatic disease. Neurogenic inflammation, which influences normal central nervous system signaling, leads to insufficient signaling/bioavailability of various cytokines. These central mechanisms play an important role in the increased pain sensitivity following inflammation and are responsible for the development of secondary hyperalgesia in regions beyond the injured tissue. Reduction of pain in rheumatic disease requires familiarity with various pain mechanisms.
Zusammenfassung
Rheumatische Erkrankungen, die durch chronische Entzündungen der Synovialgelenke gekennzeichnet sind, gehen häufig mit anhaltenden Schmerzen und erhöhter Schmerzempfindlichkeit einher. Der Entzündungsprozess ist eine komplexe Kaskade von Ereignissen, an denen mehrere Mediatoren beteiligt sind, und kann zu einem chronischen Schmerzzustand führen. Eine Entzündung kann die Angiogenese stimulieren, dadurch können wiederum Entzündungsprozesse stimuliert werden. Entzündliche Schmerzen im Rahmen von Gewebeschäden werden durch Sensibilisierung von Schmerzrezeptoren (Nozizeptoren) vermittelt. Der hauptsächliche periphere Mechanismus, der nozizeptiven Schmerzen zugrunde liegt, ist eine Veränderung der Aktivität der Nozizeptoren in den betroffenen anatomischen Strukturen (Gelenke, Sehnen und Bänder), wodurch sie empfindlicher auf normalerweise schmerzhafte Reize (Hyperalgesie) oder normalerweise nicht schmerzhafte Reize (Allodynie) reagieren. Es wird angenommen, dass die Interaktion von Nervensystem und Immunsystem eine wesentliche Rolle bei rheumatischen Erkrankungen spielt. Neurogene Entzündungen, die die normale Signalübertragung des zentralen Nervensystems beeinflussen, führen zu einer veränderten Signalübertragung/Bioverfügbarkeit verschiedener Zytokine. Diese zentralen Mechanismen spielen eine wichtige Rolle bei der Erhöhung der Schmerzempfindlichkeit nach Entzündungen und sind für die Entwicklung einer sekundären Hyperalgesie in Regionen außerhalb des entzündlichen Gewebes verantwortlich. Therapeutisch resultiert daraus für die Schmerzreduzierung bei rheumatischen Erkrankungen, dass die Behandelnden mit verschiedenen Schmerzmechanismen vertraut sein sollten.

Similar content being viewed by others
References
Ashraf S, Mapp PI, Walsh DA (2011) Contributions of angiogenesis to inflammation, joint damage, and pain in a rat model of osteoarthritis. Arthritis Rheum 63(9):2700–2710
Bannwarth B, Kostine M (2017) Nerve growth factor antagonists: is the future of monoclonal antibodies becoming clearer? Drugs 77(13):1377–1387
Bonnet CS, Walsh DA (2005) Osteoarthritis, angiogenesis and inflammation. Rheumatology (Oxford) 44(1):7–16
Cazzola M, Atzeni F, Boccassini L et al (2014) Physiopathology of pain in rheumatology. Reumatismo 66(1):4–13
Crofford LJ (2002) The hypothalamic-pituitary-adrenal axis in the pathogenesis of rheumatic diseases. Endocrinol Metab Clin North Am 31(1):1–13
Čulo MI, Morović-Vergles J (2016) Etiology and pathogenesis of pain in rheumatic diseases. Reumatizam 63(1):18–22
Gatenholm B, Brittberg M (2019) Neuropeptides: important regulators of joint homeostasis. Knee Surg Sports Traumatol Arthrosc 27(3):942–949
Grubb BD (2004) Activation of sensory neurons in the arthritic joint. Novartis Found Symp 260:28–36
Handwerker HO (2007) Advancing our understanding of the mechanisms and mediators underlying pain and inflammation. Clin Drug Investig 27(1):1–6
Kojima M, Kojima T, Suzuki S et al (2009) Depression, inflammation, and pain in patients with rheumatoid arthritis. Arthritis Rheum 61(8):1018–1024
Kojima M, Kojima T, Suzuki S, Takahashi N et al (2014) Alexithymia, depression, inflammation, and pain in patients with rheumatoid arthritis. Arthritis Care Res (Hoboken) 66(5):679–686
Lampa J (2019) Pain without inflammation in rheumatic diseases. Best Pract Res Clin Rheumatol. https://doi.org/10.1016/j.berh.2019.101439
Lee YC, Frits ML (2014) Subgrouping of patients with rheumatoid arthritis based on pain, fatigue, inflammation, and psychosocial factors. Arthritis Rheumatol 66(8):2006–2014
Lin Y, Liu L, Jiang H (2017) Inhibition of interleukin‑6 function attenuates the central sensitization and pain behavior induced by osteoarthritis. Eur J Pharmacol 15(811):260–267
MacDonald IJ, Liu SC, Su CM (2018) Implications of angiogenesis involvement in arthritis. Int J Mol Sci 19(7):2012
McWilliams DF, Walsh DA (2017) Pain mechanisms in rheumatoid arthritis. Clin Exp Rheumatol 107(5):94–101
Moilanen LJ, Hämäläinen M, Nummenmaa E et al (2015) Monosodium iodoacetate-induced inflammation and joint pain are reduced in TRPA1 deficient mice—potential role of TRPA1 in osteoarthritis. Osteoarthritis Cartilage 23(11):2017–2026
Moynes DM, Vanner SJ, Lomax AE (2014) Participation of interleukin 17A in neuroimmune interactions. Brain Behav Immun 41:1–9
Nieto FR, Clark AK, Grist J (2016) Neuron-immune mechanisms contribute to pain in early stages of arthritis. J Neuroinflammation 13(1):96
Old EA, Clark AK, Malcangio M (2015) The role of glia in the spinal cord in neuropathic and inflammatory pain. Handb Exp Pharmacol 227:145–170
Riedel W, Neeck G (2001) Nociception, pain, and antinociception: current concepts. Z Rheumatol 60(6):404–415
Rifbjerg-Madsen S, Christensen AW, Christensen R et al (2017) Pain and pain mechanisms in patients with inflammatory arthritis: a Danish nationwide cross-sectional DANBIO registry survey. PLoS ONE 12(7):e180014
Sarzi-Puttini P, Atzeni F, Salaffi F (2014) Pain in rheumatic diseases: how relevant is it? Reumatismo 66(1):1–3
Seidel MF, Herguijuela M, Forkert R et al (2010) Nerve growth factor in rheumatic diseases. Semin Arthritis Rheum 40(2):109–126
Straub RH, Bijlsma JW, Masi A et al (2013) Role of neuroendocrine and neuroimmune mechanisms in chronic inflammatory rheumatic diseases—the 10-year update. Semin Arthritis Rheum 43(3):392–404
Syx D, Tran PB, Miller RE et al (2018) Peripheral mechanisms contributing to osteoarthritis pain. Curr Rheumatol Rep 20(2):9
Walsh DA, McWilliams DF (2014) Mechanisms, impact and management of pain in rheumatoid arthritis. Nat Rev Rheumatol 10(10):581–592
Yousefi B, Jadidi-Niaragh F, Azizi G (2014) The role of leukotrienes in immunopathogenesis of rheumatoid arthritis. Mod Rheumatol 24(2):225–2235
Zhang A, Lee YC (2018) Mechanisms for joint pain in rheumatoid arthritis (RA): from cytokines to central sensitization. Curr Osteoporos Rep 16(5):603–610
Zheng LX, Li KX, Hong FF (2019) Pain and bone damage in rheumatoid arthritis: role of leukotriene B4. Clin Exp Rheumatol 37(5):872–878
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
O. Seifert and C. Baerwald declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Additional information
Redaktion
C. Baerwald, Leipzig
H.-I. Huppertz, Bremen
G. Pongratz, Düsseldorf
Rights and permissions
About this article
Cite this article
Seifert, O., Baerwald, C. Interaction of pain and chronic inflammation. Z Rheumatol 80, 205–213 (2021). https://doi.org/10.1007/s00393-020-00951-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-020-00951-8