Abstract
Introduction
The purpose of this study is to use the CD15 focus score (FS) to determine the sensitivity and specificity of bacterial infection persistence in spacer-based two-stage revision arthroplasty.
Methods
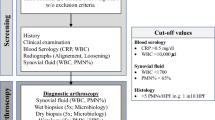
The analysis comprises 112 cases that were subjected to revision due to the presence of infection upon replacement of a joint endoprosthesis. The histopathological data were collected in accordance with the synovial-like interface membrane (SLIM) classification and the CD15-FS and correlated with the microbiological data (MD). The quantifying evaluation of the CD15-FS was performed without knowledge regarding the microbiological data (MD). Correlation with the MD was performed after a 14-day cultivation period.
Results
With a single evaluation (1 focus, field area: 1.2 mm2) with a score value of 42, the CD15-FS showed a sensitivity for the eradication of infections of 0.64 and a specificity of 0.79 (PPV = 0.5; NPV = 0.87). With tenfold evaluation (10 foci, field area: 12 mm2) with a score value of 220, the sensitivity for the eradication was 0.68, the specificity 0.91 (PPV = 0.7; NPV = 0.89). No statistically significant correlation between the score values and the different infectious species could be detected. Based on the MD in 112 cases the rate of infection eradication was 75%. Polymethylmethacrylate-particles (PMMA) were detected in the perispacertissue in 64 cases (58%). No significant correlation could be established between microbiological pathogen detection and the presence of PMMA.
Conclusion
In all cases (n = 112), periimplant synovial tissue (SLIM) with variable fibroblastic cellularity, capillary proliferation, leukocytic infiltration, fibrin deposition, new formation of woven bone and detection of PMMA particles was observed. These cases were classified as type IX perispacer synovialis/SLIM: type IX‑A with histopathological infection eradication and type IX‑B with histopathological infection persistence.
Zusammenfassung
Hintergrund
Ziel der Arbeit war es, mittels des CD15-Fokus-Scores (FS) eine Aussage zu Sensitivität und Spezifität der bakteriellen Infektpersistenz bei Spacer-basiertem zweizeitigem Gelenkendoprothesenwechsel zu ermitteln.
Methoden
Die Stichprobe umfasste 112 Fälle in denen aufgrund einer Infektion bei einem Gelenkendoprothesenwechsel eine Revision erfolgte. Die histopathologischen Daten wurden gemäß der SLIM-Klassifikation („synovial-like interface membrane“) und des CD15-FS erhoben und mit den mikrobiologischen Daten korreliert. Die quantifizierende Bewertung durch den CD15-FS erfolgte ohne Kenntnis der mikrobiologischen Daten(MD). Die Korrelation erfolgte erst nach Einhaltung einer 14-tägigen Kultivierung.
Ergebnisse
Der CD15-FS zeigte bei einfacher Auswertung eine Sensitivität für die Infekteradikation von 0,64 und eine Spezifität von 0,79 (PPV = 0,5; NPV = 0,87). Bei 10-facher Auswertung ergab sich eine Sensitivität von 0,68 und eine Spezifität von 0,91 (PPV = 0,7; NPV = 0,89). Es ließ sich kein signifikanter Zusammenhang mit den infektiösen Spezies nachweisen. Den MD zufolge betrug die Rate der Infekteradikation 75 %. In 64 Fällen bestand ein Partikelnachweis (Polymethylmethacrylat [PMMA]). Es konnte kein signifikanter Zusammenhang zwischen Erregernachweis und Präsenz von PMMA gezeigt werden.
Schlussfolgerung
In sämtlichen Fällen zeigte sich periimplantäres Gewebe mit variabler fibroblastischer Zellularität, Kapillarproliferation, Leukozyteninfiltration, Fibrinablagerung, Neubildung von Geflechtknochen und Nachweis von PMMA. Die Klassifikation erfolgte als Synovialis vom Perispacertyp – Typ 9, entsprechend Typ 9A mit histopathologischer Infekteradikation oder Typ 9B mit histopathologischer Infektpersistenz.





Similar content being viewed by others
Change history
06 July 2021
An Erratum to this paper has been published: https://doi.org/10.1007/s00393-021-01033-z
References
Aalirezaie A (2019) Hip and knee section, diagnosis, reimplantation: proceedings of international consensus on orthopedic infections. J Arthroplasty 34(2S):S369–S379. https://doi.org/10.1016/j.arth.2018.09.021
Akgün D (2019) High cure rate of periprosthetic hip joint infection with multidisciplinary team approach using standardized two-stage exchange. J Orthop Surg Res 14(1):78. https://doi.org/10.1186/s13018-019-1122-0
Athanasou NA (1995) Diagnosis of infection by frozen section during revision Arthroplasty. J Bone Joint Surg Br 77:28–33
Bauer TW (2006) Diagnosis of periprosthetic infection. J Bone Joint Surg Am 88:869–882. https://doi.org/10.2106/JBJS.E.01149
Bauer TW (2019) Hip and knee section, diagnosis, laboratory tests: proceedings of international consensus on orthopedic infections. J Arthroplasty 34(2S):S351–S359. https://doi.org/10.1016/j.arth.2018.09.019
Bori G (2007) Usefulness of histological analysis for predicting the presence of microorganisms at the time of reimplantation after hip resection Arthroplasty for the treatment of infection. J Bone Joint Surg Am 89:1232–1237. https://doi.org/10.2106/JBJS.F.00741
Della Valle CJ (1999) Analysis of frozen sections of Intraoperative specimens obtained at the time of reoperation after hip or knee resection Arthroplasty for the treatment of infection. J Bone Joint Surg Am 81(5):684–689. https://doi.org/10.2106/00004623-199905000-00009
Dieckmann R (2014) Two-stage hip revision arthroplasty with a hexagonal modular cementless stem in cases of periprosthetic infection. BMC Musculoskelet Disord 15:398. https://doi.org/10.1186/1471-2474-15-398
Dinneen LC, Blakesley BC (1973) Algorithm AS 62: a generator for the sampling distribution of the Mann–whitney U statistic. Appl Stat 22(2):269–273
Ethgen O (2004) Health-related quality of life in total hip and total knee Arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 86-A:963–974
Fletcher C (2013) WHO classification of tumours of soft tissue and bone, 4th edn.
George J (2016) Are frozen sections and MSIS criteria reliable at the time of reimplantation of two-stage revision Arthroplasty? Clin Orthop Relat Res 474(7):1619–1626. https://doi.org/10.1007/s11999-015-4673-3
George J (2018) Diagnostic utility of histological analysis for detecting ongoing infection during two-stage revision Arthroplasty in patients with inflammatory arthritis. J Arthroplasty 33(7S):S219–S223. https://doi.org/10.1016/j.arth.2017.12.021
Gontarewicz A (2012) Morphological study of synovial changes in two-stage reconstructions of the infected hip and knee arthroplasties. BMJ Open 2:e1467. https://doi.org/10.1136/bmjopen-2012-001467
Hansen T (2002) New aspects in the histological examination of polyethylene wear particles in failed total joint replacements. Acta Histochem 104:263–269
Hoell S (2016) Eradication rates, risk factors, and implant selection in two-stage revision knee arthroplasty: a mid-term follow-up study. J Orthop Surg Res 11(1):93. https://doi.org/10.1186/s13018-016-0428-4
Izakovicova P (2019) Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev 4(7):482–494. https://doi.org/10.1302/2058-5241.4.180092
Krenn V (2014) Revised histopathological consensus classification of joint implant related pathology. Pathol Res Pract 210(12):779–786. https://doi.org/10.1016/j.prp.2014.09.017
Krenn VT (2017) CD15 FS: Infection diagnosis and stratification into low-virulence and high-virulence microbial pathogens in periprosthetic joint infection. Pathol Res Pract 213(5):541–547. https://doi.org/10.1016/j.prp.2017.01.002
Li C (2020) Twenty common errors in the diagnosis and treatment of periprosthetic joint infection. Int Orthop 44(1):3–14. https://doi.org/10.1007/s00264-019-04426-7 (Review. Erratum in: Int Orthop. 2019 Dec 10; PMID: 31641803)
Morawietz L (2009) Twenty-three neutrophil granulocytes in 10 high-power fields is the best histopathological threshold to differentiate between aseptic and septic endoprosthesis loosening. Histopathology 54(7):847–853. https://doi.org/10.1111/j.1365-2559.2009.03313.x
Morawietz L (2006) Proposal for a histopathological consensus classification of the periprosthetic interface membrane. J Clin Pathol 59(6):591–597
Perino G (2018) Diagnostic guidelines for the histological particle algorithm in the periprosthetic neo-synovial tissue. BMC Clin Pathol 18:7. https://doi.org/10.1186/s12907-018-0074-3
Parvizi J (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty 33(5):1309–1314.e2. https://doi.org/10.1016/j.arth.2018.02.078
Parvizi J (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469:2992–2994. https://doi.org/10.1007/s11999-011-2102-9
Trampuz A (2006) Infections associated with orthopedic implants. Curr Opin Infect Dis 19(4):349–356 (Review)
Triantafyllopoulos GK (2017) Periprosthetic infection recurrence after 2‑stage exchange Arthroplasty: failure or fate? J Arthroplasty 32(2):526–531. https://doi.org/10.1016/j.arth.2016.08.002
Tsaras G (2012) Utility of intraoperative frozen section histopathology in the diagnosis of periprosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am 94:1700–1711. https://doi.org/10.2106/JBJS.J.00756
Zmistowski B (2014) Diagnosis of periprosthetic joint infection. J Orthop Res 32(Suppl 1):98–107. https://doi.org/10.1002/jor.22553
Acknowledgements
Special thanks are due to the employees of MVZ-HZMD-Trier GmbH, Ms. S. Giak, Ms. C. Soika and Ms. S. Klee, for the data collection and input of clinical as well as microbiological findings, especially in the context of preparation of the histopathological findings.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Liewen, V.T. Krenn, R. Dieckmann, L. Bause, M. Liebisch, A. Niemeier, A. Trampuz, and V. Krenn declare that there is no conflict of interest with regard to the contents of this publication. Regardless of a possible conflict of interest, this scientific contribution is independent and product neutral.
This article does not include any studies performed on humans or animals. The Ethics Committee of the State Medical Association of Rhineland-Palatinate, Mainz, Germany, has issued a positive vote under the reference number 837.400.15 (10168), “CD 15 Quantifizierung (CD 15 Focus Score) als Basis der periprothetischen Infektionsdiagnostik: Subspezifizierung der bakteriellen Infektion in niedrigpathogene und hochpathogenen Bakterien” (English: “CD 15 quantification (CD 15 focus score) as the basis of periprosthetic infection diagnosis: sub-specification of bacterial infection in low-pathogenic and highly pathogenic bacteria”), in which it is stated that there are no ethical or legal concerns.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Doctoral thesis by Caroline Liewen
These data represent a part of Caroline Liewen’s doctoral thesis at the Charité University Medicine, Berlin (supervisor of the thesis: Prof. Dr. med. Veit Krenn).
The original online version of this article was revised: In the original online version of the article, Figure 2 was incorrect.
Rights and permissions
About this article
Cite this article
Liewen, C., Krenn, V.T., Dieckmann, R. et al. Diagnostic value of the CD 15 focus score in two-stage revision arthroplasty of periprosthetic joint infections. Z Rheumatol 81, 342–351 (2022). https://doi.org/10.1007/s00393-020-00941-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-020-00941-w
Keywords
- Periprosthetic joint infection
- CD15 focus score
- Eradication of infection
- Two-stage revision arthroplasty
- SLIM-Classification