Abstract
Objective
This study aimed to assess the all-cause and cause-specific standardized mortality ratios (SMRs) in patients with giant cell arteritis (GCA).
Methods
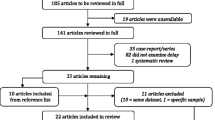
We surveyed studies examining all-cause and/or cause-specific SMRs in patients with GCA compared to the general population, using MEDLINE, EMBASE, Cochrane databases, and manual searches. We then performed a meta-analysis of all-cause, sex-specific, region-specific, and cause-specific SMRs in patients with GCA.
Results
In total, 8 reports including 1972 patients with GCA (including 877 patients who died) met the inclusion criteria. Compared with the general population, all-cause SMR was not increased in patients with GCA (SMR 1.081, 95% confidence interval [CI] 0.963–1.214, p = 0.184). Stratification by region showed no significant increase in all-cause SMR in Europe and USA. Sex-specific meta-analysis revealed that the pooled SMR was 1.046 (95%CI 0.834–1.314, p = 0.696) for women and 1.051 (95%CI 0.974–1.133, p = 0.204) for men. There were no sex-specific significant differences in SMR. The risk of mortality due to cardiovascular disease (CVD) was significantly increased (SMR 1.312, 95%CI 1.136–1.516, p < 0.001). However, there was no significant increase in the SMR for mortality due to cancer (SMR 0.833, 95%CI 0.613–1.132, p = 0.243).
Conclusions
Patients with GCA do not show increased rates of death from all causes, regardless of sex, region, or malignancy. However, these patients are at an increased risk of death due to CVD.
Zusammenfassung
Ziel
Ziel der Studie war es, standardisierte Mortalitätsverhältnisse („standardized mortality ratios“ [SMR]) in Bezug auf die Gesamt- und ursachenspezifische Mortalität bei Patienten mit Riesenzellarteriitis (RZA) zu bestimmen.
Methoden
In MEDLINE, EMBASE und Cochrane-Datenbanken sowie manuell wurde nach Studien zu Gesamt- und/oder ursachenspezifischen SMR bei RZA-Patienten im Vergleich zur Allgemeinbevölkerung gesucht. Daraufhin wurde eine Metaanalyse der Gesamt-, geschlechtsspezifischen, regionsspezifischen und ursachenspezifischen SMR bei Patienten mit RZA durchgeführt.
Ergebnisse
Insgesamt 8 Publikationen mit 1972 RZA-Patienten (einschließlich 877 Patienten, die verstarben) erfüllten die Einschlusskriterien. Im Vergleich zur Allgemeinbevölkerung war das Gesamt-SMR bei Patienten mit RZA nicht erhöht (SMR 1,081, 95%-Konfidenzintervall [KI] 0,963–1,214, p = 0,184). Die regionale Stratifikation ergab keine signifikante Erhöhung des Gesamt-SMR in Europa und den USA. Eine geschlechtsbezogene Metaanalyse ergab ein gepooltes SMR von 1,046 (95%-KI 0,834–1,314, p = 0,696) für Frauen und 1,051 (95%-KI 0,974–1,133, p = 0,204) für Männer. Es fanden sich keine signifikanten geschlechtsspezifischen Unterschiede im SMR. Das Mortalitätsrisiko bedingt durch kardiovaskuläre Erkrankungen war signifikant erhöht (SMR 1,312, 95%-KI 1,136–1,516, p < 0,001). Hinsichtlich des SMR für tumorbedingte Mortalität war dagegen keine signifikante Erhöhung festzustellen (SMR 0,833, 95%-KI 0,613–1,132, p = 0,243).
Schlussfolgerungen
Patienten mit RZA weisen keine erhöhten Gesamtsterberaten auf, unabhängig von Geschlecht, geografischer Region oder Malignität. Die Patienten haben aber ein erhöhtes Sterberisiko bedingt durch kardiovaskuläre Erkrankungen.



Similar content being viewed by others
References
Davey Smith G, Egger M (1997) Meta-analyses of randomised controlled trials. Lancet 350(9085):1182
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Egger M, Smith GD, Phillips AN (1997) Meta-analysis: principles and procedures. BMJ 315(7121):1533–1537
Gonzalez-Gay MA, Blanco R, Abraira V et al (1997) Giant cell arteritis in Lugo, Spain, is associated with low longterm mortality. J Rheumatol 24(11):2171–2176
González-Gay MA, García-Porrúa C (2001) Epidemiology of the vasculitides. Rheum Dis Clin North Am 27(4):729–749
Gonzalez-Gay MA, Lopez-Diaz MJ, Martinez-Lado L et al (2007) Cancer in biopsy-proven giant cell arteritis. A population-based study. Semin Arthritis Rheum 37(3):156–163
Gonzalez-Gay MA, Rubiera G, Pineiro A et al (2005) Ischemic heart disease in patients from Northwest Spain with biopsy proven giant cell arteritis. A population based study. J Rheumatol 32(3):502–506
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Hunder GG, Bloch DA, Michel BA et al (1990) The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheumatol 33(8):1122–1128
Jennette JC, Falk R, Bacon P et al (2013) 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheumatol 65(1):1–11
Julious SA, Nicholl J, George S (2001) Why do we continue to use standardized mortality ratios for small area comparisons? J Public Health Med 23(1):40–46
Kermani TA, Warrington KJ, Crowson CS et al (2013) Large-vessel involvement in giant cell arteritis: a population-based cohort study of the incidence-trends and prognosis. Ann Rheum Dis 72(12):1989–1994
Matteson EL, Gold KN, Bloch DA et al (1996) Long-term survival of patients with giant cell arteritis in the American College of Rheumatology giant cell arteritis classification criteria cohort. Am J Med 100(2):193–196
Mohammad AJ, Nilsson JA, Jacobsson LT et al (2015) Incidence and mortality rates of biopsy-proven giant cell arteritis in southern Sweden. Ann Rheum Dis 74(6):993–997
Nesher G, Sonnenblick M, Friedlander Y (1994) Analysis of steroid related complications and mortality in temporal arteritis: a 15-year survey of 43 patients. J Rheumatol 21(7):1283–1286
Proven A, Gabriel SE, Orces C et al (2003) Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Care Res 49(5):703–708
Uddhammar A, Eriksson AL, Nystrom L et al (2002) Increased mortality due to cardiovascular disease in patients with giant cell arteritis in northern Sweden. J Rheumatol 29(4):737–742
Acknowledgements
This research received no specific grant from any public, commercial, or not-for-profit sectors funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. H. Lee and G. G. Song declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Lee, Y.H., Song, G.G. Overall and cause-specific mortality in giant cell arteritis. Z Rheumatol 77, 946–951 (2018). https://doi.org/10.1007/s00393-018-0440-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-018-0440-7