Abstract
Background
Adrenal infarction is a rare complication of antiphospholipid syndrome (APS).
Objectives
The purpose of the current study is to detect and study the magnetic resonance imaging (MRI) findings of adrenal glands in APS patients.
Materials and methods
In a cross-sectional study, the data of 20 patients with primary or secondary APS were compared to 20 SLE patients without antiphospholipid antibody (aPL) syndrome (controls). MRI of the abdomen showing the adrenal glands was performed.
Results
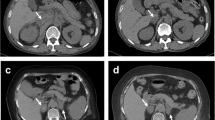
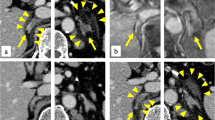
Of the patients, 80% were females with a mean age 32.45 ± 9.93 years, and mean disease duration of 46.65 ± 58.71 months. Adrenal gland abnormalities in the MRI study were detected in 35 % of APS patients vs. no abnormalities detected in the SLE controls. Adrenal gland enlargement was found in all patients (35 %). Capsular enhancement (infarction or hemorrhagic infarction) was found in 5 patients, increased stranding of the surrounding fat planes (inflammatory process) in 4 patients and increased signal on T1WI and T2WI (hemorrhage) in 3 patients. In patients with adrenal gland involvement, 71.4 % had triple aPL positivity compared to 23.1 % in patients with normal adrenal findings (p = 0.04).
Conclusions
Adrenal gland abnormalities on MRI were detected in 35 % of the APS patients (whether primary or secondary); thus, increased focus on management is needed. This percentage is not small and needs to be focused on in terms of management.
Zusammenfassung
Hintergrund
Ein Nebenniereninfarkt ist eine seltene Komplikation bei Antiphospholipidsyndrom (APS).
Zielsetzung
Ziel der vorliegenden Studie ist die Untersuchung von MRT(Magnetresonanztomographie)-Befunden der Nebennieren in einer Gruppe von APS-Patienten.
Material und Methoden
In dieser Querschnittsstudie wurden die von 20 Patienten mit primären oder sekundären APS mit denen von 20 SLE(systemischer Lupus erythematosus)-Patienten ohne Antiphospholipidantikörper (aPL) verglichen. Durchgeführt wurden abdominelle MRTs mit Darstellung der Nebennieren.
Ergebnisse
Von allen Patienten waren 80% Frauen mit einem Durchschnittsalter 32,45 ± 9,93 Jahre, die mittlere Krankheitsdauer lag bei 46,65 ± 58,71 Monaten. In den MRTs wurden bei 35 % der APS-Patienten Anomalien detektiert, im SLE-Kontrollkollektiv dagegen bei keinem. Eine Vergrößerung der Nebenniere bestand bei allen Patienten (35 %), ein kapsuläres Enhancement (Infarkt bzw. hämorrhagischer Infarkt) bei 5, vermehrtes Stranding im periadrenalen Fettgewebe (entzündlicher Prozess) bei 4 und erhöhte T1W- und T2W-Signalwerte (Blutung) bei 3 Patienten. Von den Patienten mit adrenaler Beteiligung wiesen 71,4 % eine Triple-aPL-Positivität auf, von den Patienten mit unauffälligen Nebennierenbefunden dagegen nur 23,1% (p = 0,04).
Schlussfolgerungen
Nebennierenanomalien wurden magnetresonanztomographisch bei 35 % der APS-Patienten nachgewiesen, was die Notwendigkeit einer stärkeren Fokussierung auf das entsprechende Management verdeutlicht. Hinsichtlich des Patientenmanagements ist dieser nicht unerhebliche Prozentsatz zu bedenken.




Similar content being viewed by others
References
Charles E (2009) Antiphospholipid syndrome review. Clin Lab Med 29(2):305–319
Levine JS, Branch DW, Rauch J (2002) The antiphospholipid syndrome. N Engl J Med 346(10):752–763
Piette JC, Wechsler B, Frances C, Papo T, Godeau P (1993) Exclusion criteria for primary antiphospholipid syndrome. J Rheumatol 20:1802–1804
Merkel PA, Chang Y, Pierangeli SS, Convery K, Harris EN, Polisson RP (1996) The prevalence and clinical associations of anticardiolipin antibodies in a large inception cohort of patients with connective tissue diseases. Am J Med 101(6):576–583
Miyakis S, Lockshin MD, Atsumi T et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306
Zoghlami-Rintelen C, Vormittag R, Sailer T et al (2005) The presence of IgG antibodies against beta2-glycoprotein I predicts the risk of thrombosis in patients with the lupus anticoagulant. J Thromb Haemost 3:1160–1165
Papadopoulos KI, Jönsson A, Berntorp E, Törnquist C, Hulthén UL (1995) Primary antiphospholipid syndrome associated with postoperative primary adrenal failure. J Intern Med 238:175–178
Elsayes KM, Mukundan G, Narra VR et al (2004) Adrenal masses: MR imaging features with pathologic correlation. Radiographics 24(Suppl 1):73–86
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725 doi:10.1002/art.1780400928
Petri M, Genovese M, Engle E, Hochberg M (1991) Definition, incidence and clinical description of flare in systemic lupus erythematosus. Arthritis Rheum 8:937–944
Abrahamowicz M, Fortin PR, Berger R du, Nayak R, Neville C, Liang MH (1998) The relationship between disease activity and expert physician’s decision to start major treatment in active systemic lupus erythematosus: a decision aid for development of entry criteria for clinical trials. J Rheumatol 25:277–284
Brandt JT, Triplett DA, Alving B et al (1995) Criteria for the diagnosis of lupus anticoagulants: an update. On behalf of the Subcommittee on Lupus anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the ISTH. Thromb Haemost 74:1185–1190
Takebayashi K, Aso Y, Tayama K, Takemura Y, Inukai T (2003) Primary antiphospholipid syndrome associated with acute adrenal failure. Am J Med Sci 325:41–44
Espinosa G, Santos E, Cervera R et al (2003) Adrenal involvement in the antiphospholipid syndrome clinical and immunologic characteristics of 86 Patients. Medicine (Baltimore) 82(2):106–118
Arnason JA, Graziano FM (1995) Adrenal insufficiency in the antiphospholipid antibody syndrome. Semin Arthritis Rheum 25:109–116
Carvalho JF de, Caleiro MT, Vendramini M, Bonfá E (2010) Clinical and laboratory evaluation of patients with primary antiphopholipid syndrome according to the frequency of antinuclear antibody (ANA Hep-2). Rev Bras Reumatol 5(3):262–272
Dahiya S, Bhagavan A, Ooi WB (2012) Spontaneous bilateral adrenal hemorrhage. Endocrine 42(1):226–227. doi:10.1007/s12020-012-9678-z
Dhawan N, Bodukam VK, Thakur K, Singh A, Jenkins D, Bahl J (2015) Idiopathic bilateral adrenal hemorrhage in a 63-year-old male: a case report and review of the literature. Case Rep Urol: doi:10.1155/2015/503638
Oelkers W (1996) Adrenal insufficiency. N Engl J Med 335:1206–1212
Ruffatti AA, Salvan E, Del Ross T et al (2014) Treatment strategies and pregnancy outcomes in antiphospholipid syndrome patients with thrombosis and triple antiphospholipid positivity. A european multicentre retrospective study. Thromb Haemost 112(4):727–735. doi:10.1160/TH14-03-0191
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. A. Shahin, S. M. El Desouky, M. Y. Awadallah, and D. E. Megahed state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or animals.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Shahin, A.A., El Desouky, S.M., Awadallah, M.Y. et al. Adrenal gland abnormalities detected by magnetic resonance imaging in patients with antiphospholipid syndrome. Z Rheumatol 76, 170–175 (2017). https://doi.org/10.1007/s00393-016-0107-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-016-0107-1