Abstract
Background
The nonuniform benefit of tricuspid annuloplasty may be explained by the proportionality of tricuspid regurgitation (TR) severity to right ventricular (RV) area. The purpose of this study was to delineate distinct morphological phenotypes of functional TR and investigate their prognostic implications in patients undergoing tricuspid annuloplasty during left-sided valvular surgery.
Methods
The ratios of pre-procedural effective regurgitant orifice area (EROA) with right ventricular end-diastolic area (RVDA) were retrospectively assessed in 290 patients undergoing tricuspid annuloplasty. Based on optimal thresholds derived from penalized splines and maximally selected rank statistics, patients were stratified into proportionate (EROA/RVDA ratio ≤ 1.74) and disproportionate TR (EROA/RVDA ratio > 1.74).
Results
Overall, 59 (20%) and 231 (80%) patients had proportionate and disproportionate TR, respectively. Compared to those with proportionate TR, patients with disproportionate TR were older, had a higher prevalence of atrial fibrillation, lower pulmonary pressures, more impaired RV function, and larger tricuspid leaflet tenting area. Over a median follow-up of 4.1 years, 79 adverse events (47 heart failure hospitalizations and 32 deaths) occurred. Patients with disproportionate TR had higher rates of adverse events than those with proportionate TR (32% vs 10%; P = 0.001) and were independently associated with poor outcomes on multivariate analysis. TR proportionality outperformed guideline-based classification of TR severity in outcome prediction and provided incremental prognostic value to both the EuroSCORE II and STS score (incremental χ2 = 6.757 and 9.094 respectively; both P < 0.05).
Conclusions
Disproportionate TR is strongly associated with adverse prognosis and may aid patient selection and risk stratification for tricuspid annuloplasty with left-sided valvular surgery.
Graphical Abstract




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Spinner EM, Shannon P, Buice D, Jimenez JH, Veledar E, Del Nido PJ et al (2011) In vitro characterization of the mechanisms responsible for functional tricuspid regurgitation. Circulation 124(8):920–929
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F et al (2021) 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143(5):e35–e71
Moraca RJ, Moon MR, Lawton JS, Guthrie TJ, Aubuchon KA, Moazami N et al (2009) Outcomes of tricuspid valve repair and replacement: a propensity analysis. Ann Thorac Surg 87(1):83–88 (discussion 8-9)
Hahn RT, Zamorano JL (2017) The need for a new tricuspid regurgitation grading scheme. Eur Heart J Cardiovasc Imaging 18(12):1342–1343
Badano LP, Hahn R, Rodriguez-Zanella H, Araiza Garaygordobil D, Ochoa-Jimenez RC, Muraru D (2019) Morphological assessment of the tricuspid apparatus and grading regurgitation severity in patients with functional tricuspid regurgitation: thinking outside the box. JACC Cardiovasc Imaging 12(4):652–664
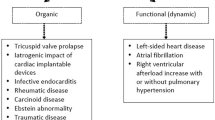
Prihadi EA, Delgado V, Leon MB, Enriquez-Sarano M, Topilsky Y, Bax JJ (2019) Morphologic types of tricuspid regurgitation: characteristics and prognostic implications. JACC Cardiovasc Imaging 12(3):491–499
Grayburn PA, Sannino A, Packer M (2021) Distinguishing proportionate and disproportionate subtypes in functional mitral regurgitation and left ventricular systolic dysfunction. JACC Cardiovasc Imaging 14(4):726–729
Obadia JF, Messika-Zeitoun D, Leurent G, Iung B, Bonnet G, Piriou N et al (2018) Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med 379(24):2297–2306
Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM et al (2018) Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 379(24):2307–2318
Fortuni F, Dietz MF, Prihadi EA, van der Bijl P, De Ferrari GM, Bax JJ et al (2021) Ratio between vena contracta width and tricuspid annular diameter: prognostic value in secondary tricuspid regurgitation. J Am Soc Echocardiogr 34(9):944–954
Yiu KH, Wong A, Pu L, Chiang MF, Sit KY, Chan D et al (2014) Prognostic value of preoperative right ventricular geometry and tricuspid valve tethering area in patients undergoing tricuspid annuloplasty. Circulation 129(1):87–92
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP et al (2009) Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr 10(1):1–25
Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C et al (2010) European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr 11(4):307–332
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2006) Recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1-39 e14
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713 (quiz 86-8)
Topilsky Y, Khanna A, Le Tourneau T, Park S, Michelena H, Suri R et al (2012) Clinical context and mechanism of functional tricuspid regurgitation in patients with and without pulmonary hypertension. Circ Cardiovasc Imaging 5(3):314–323
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA et al (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. https://doi.org/10.1161/CIR.0000000000000031
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ et al (2017) 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 38(36):2739–2791
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA et al (2017) Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 30(4):303–371
Lancellotti P, Pibarot P, Chambers J, La Canna G, Pepi M, Dulgheru R et al (2022) Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper. Eur Heart J Cardiovasc Imaging 23(5):e171–e232
Chemla D, Castelain V, Humbert M, Hebert JL, Simonneau G, Lecarpentier Y et al (2004) New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure. Chest 126(4):1313–1317
Brener MI, Lurz P, Hausleiter J, Rodes-Cabau J, Fam N, Kodali SK et al (2022) Right ventricular-pulmonary arterial coupling and afterload reserve in patients undergoing transcatheter tricuspid valve repair. J Am Coll Cardiol 79(5):448–461
Fortmeier V, Lachmann M, Unterhuber M, Stolz L, Kassar M, Ochs L et al (2023) Epiphenomenon or prognostically relevant interventional target? A novel proportionality framework for severe tricuspid regurgitation. J Am Heart Assoc 12(6):e028737
Fukuda S, Saracino G, Matsumura Y, Daimon M, Tran H, Greenberg NL et al (2006) Three-dimensional geometry of the tricuspid annulus in healthy subjects and in patients with functional tricuspid regurgitation: a real-time, 3-dimensional echocardiographic study. Circulation 114(1 Suppl):I492–I498
Fukuda S, Gillinov AM, Song JM, Daimon M, Kongsaerepong V, Thomas JD et al (2006) Echocardiographic insights into atrial and ventricular mechanisms of functional tricuspid regurgitation. Am Heart J 152(6):1208–1214
Lopes PM, Albuquerque F, Freitas P, Gama F, Horta E, Reis C et al (2021) Assessing proportionate and disproportionate functional mitral regurgitation with individualized thresholds. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jeaa356.081
Orban M, Karam N, Lubos E, Kalbacher D, Braun D, Deseive S et al (2021) Impact of proportionality of secondary mitral regurgitation on outcome after transcatheter mitral valve repair. JACC Cardiovasc Imaging 14(4):715–725
Weber KT, Janicki JS, Shroff S, Fishman AP (1981) Contractile mechanics and interaction of the right and left ventricles. Am J Cardiol 47(3):686–695
Damiano RJ Jr, La Follette P Jr, Cox JL, Lowe JE, Santamore WP (1991) Significant left ventricular contribution to right ventricular systolic function. Am J Physiol 261(5 Pt 2):H1514–H1524
Spinner EM, Lerakis S, Higginson J, Pernetz M, Howell S, Veledar E et al (2012) Correlates of tricuspid regurgitation as determined by 3D echocardiography: pulmonary arterial pressure, ventricle geometry, annular dilatation, and papillary muscle displacement. Circ Cardiovasc Imaging 5(1):43–50
Namazi F, van der Bijl P, Fortuni F, Mertens BJA, Kamperidis V, van Wijngaarden SE et al (2021) Regurgitant volume/left ventricular end-diastolic volume ratio: prognostic value in patients with secondary mitral regurgitation. JACC Cardiovasc Imaging 14(4):730–739
Chen Y, Liu JH, Chan D, Sit KY, Wong CK, Ho KL et al (2016) Prevalence, predictors and clinical outcome of residual pulmonary hypertension following tricuspid annuloplasty. J Am Heart Assoc. https://doi.org/10.1161/JAHA.116.003353
Tse YK, Li HL, Yu SY, Wu MZ, Ren QW, Huang J et al (2022) Prognostic value of right ventricular remodelling in patients undergoing concomitant aortic and mitral valve surgery. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jeac162
Zhong Y, Bai W, Wang H, Qian H, Rao L (2021) Impact of concomitant tricuspid annuloplasty on right ventricular remodeling in patients with rheumatic mitral valve disease. Cardiovasc Ultrasound 19(1):16
Navia JL, Nowicki ER, Blackstone EH, Brozzi NA, Nento DE, Atik FA et al (2010) Surgical management of secondary tricuspid valve regurgitation: annulus, commissure, or leaflet procedure? J Thorac Cardiovasc Surg 139(6):1473–82 e5
Yamauchi H, Vasilyev NV, Marx GR, Loyola H, Padala M, Yoganathan AP et al (2012) Right ventricular papillary muscle approximation as a novel technique of valve repair for functional tricuspid regurgitation in an ex vivo porcine model. J Thorac Cardiovasc Surg 144(1):235–242
Couetil JP, Nappi F, Spadaccio C, Fiore A (2021) Papillary muscle septalization for functional tricuspid regurgitation: proof of concept and preliminary clinical experience. JTCVS Tech 10:282–288
Lurz P, Stephan von Bardeleben R, Weber M, Sitges M, Sorajja P, Hausleiter J et al (2021) Transcatheter edge-to-edge repair for treatment of tricuspid regurgitation. J Am Coll Cardiol 77(3):229–239
Funding
This work was supported by the Sanming Project of Medicine in Shenzhen, China (No. SZSM201911020) and HKU-SZH Fund for Shenzhen Key Medical Discipline (No. SZXK2020081).
Author information
Authors and Affiliations
Contributions
Conceptualization: Y-KT, FAF, K-HY; methodology: Y-KT, H-LL, Q-WR, J-YH, M-ZW, CK-LL, S-YY, DH, H-FT, FAF, K-HY; formal analysis and investigation: Y-KT; writing—original draft preparation: Y-KT, FAF, K-HY; writing—review and editing: Y-KT, H-LL, FAF, K-HY; funding acquisition: K-HY; supervision: H-FT, FAF, K-HY.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee of the West Cluster Hospital Authority of Hong Kong (UW 13–169).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tse, YK., Li, HL., Ren, QW. et al. Morphological and functional types of tricuspid regurgitation: prognostic value in patients undergoing tricuspid annuloplasty during left-sided valvular surgery. Clin Res Cardiol 112, 1463–1474 (2023). https://doi.org/10.1007/s00392-023-02265-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-023-02265-6