Abstract
Background
Reflux-induced esophagitis might facilitate ablation-induced esophageal lesions (ELs) following pulmonary vein isolation (PVI), and these may progress to atrio-esophageal fistula (AEF). In contrast, preexisting ELs are not prone to progression but may affect procedure planning.
Objective
To study the incidence of preexisting esophageal and upper gastrointestinal (UGI) pathology in patients undergoing PVI, and the relation to ablation-induced ELs.
Methods
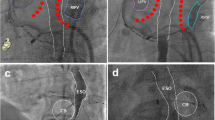
From 08/2018 to 09/2021, consecutive patients undergoing (radiofrequency [RF] or cryoballoon [CB]) PVI were examined by esophagogastroscopy (EGD) before and following ablation. Postprocedural endoscopic ultrasound (EUS) was added in 2021.
Results
412 patients (median age 67.5 [IQR 61.3–75.0] years, 56.1% male) were studied. Preprocedural EGD showed abnormalities in 226/399 patients, 15% in the lower third of the esophagus. Half (99/226) were relevant for PVI, 13 procedures were postponed, 6 due to pathological EGD results.
A third of the patients with new esophageal injury following ablation had preexisting esophagitis which was associated with a trend for a higher incidence of ELs after RF ablation (12.5 vs. 6.9%, p = 0.232), and a six- and two-fold higher rate of food retention after CB-PVI (28.6 vs. 4.5%, p = 0.008) and RF ablation (8.3 vs. 4.4%, p = 0.279), respectively.
Conclusion
(1) EGD before PVI showed UGI abnormalities in > 50% of patients, one-fourth of these relevant for PVI. (2) Esophageal inflammation was associated with a higher incidence of post-ablation (peri)-esophageal injury. Whether having this information before ablation is able to reduce ELs or AEF remains to be shown.


Similar content being viewed by others
Abbreviations
- AF:
-
Atrial fibrillation
- AEF:
-
Atrio-esophageal fistula
- CB:
-
Cryoballoon
- EGD:
-
Esophagogastroscopy
- EL:
-
Esophageal lesion
- EUS:
-
Endoscopic ultrasound
- GERD:
-
Gastro-esophageal reflux disease
- IQR:
-
Interquartile range
- LA:
-
Left atrium/left atrial
- LAPW:
-
Left atrial posterior wall
- LET:
-
Luminal esophageal temperature
- OR:
-
Odds ratio
- PPI:
-
Proton-pump-inhibitor
- PVI:
-
Pulmonary vein isolation
- RF:
-
Radiofrequency
- UGI:
-
Upper gastrointestinal
- vs:
-
Versus
References
Knopp H, Halm U, Lamberts R, Knigge I, Zachaus M, Sommer P et al (2014) Incidental and ablation-induced findings during upper gastrointestinal endoscopy in patients after ablation of atrial fibrillation: a retrospective study of 425 patients. Heart Rhythm 11(4):574–578. https://doi.org/10.1016/j.hrthm.2014.01.010
Marrouche NF, Guenther J, Segerson NM, Daccarett M, Rittger H, Marschang H et al (2007) Randomized comparison between open irrigation technology and intracardiac-echo-guided energy delivery for pulmonary vein antrum isolation: procedural parameters, outcomes, and the effect on esophageal injury. J Cardiovasc Electrophysiol 18(6):583–588. https://doi.org/10.1111/j.1540-8167.2007.00879.x
Kapur S, Barbhaiya C, Deneke T, Michaud GF (2017) Esophageal injury and atrioesophageal fistula caused by ablation for atrial fibrillation. Circulation 136(13):1247–1255. https://doi.org/10.1161/circulationaha.117.025827
Zawada AE, Moszak M, Skrzypczak D, Grzymislawski M (2018) Gastrointestinal complications in patients with diabetes mellitus. Adv Clin Exp Med 27(4):567–572. https://doi.org/10.17219/acem/67961
Schoonderwoerd BA, Smit MD, Pen L, Van Gelder IC (2008) New risk factors for atrial fibrillation: causes of “not-so-lone atrial fibrillation.” Europace 10(6):668–673. https://doi.org/10.1093/europace/eun124
Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP et al (2006) Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 114(2):119–125. https://doi.org/10.1161/CIRCULATIONAHA.105.595140
Furnkranz A, Bordignon S, Schmidt B, Bohmig M, Bohmer MC, Bode F et al (2013) Luminal esophageal temperature predicts esophageal lesions after second-generation cryoballoon pulmonary vein isolation. Heart Rhythm 10(6):789–793. https://doi.org/10.1016/j.hrthm.2013.02.021
Halm U, Gaspar T, Zachaus M, Sack S, Arya A, Piorkowski C et al (2010) Thermal esophageal lesions after radiofrequency catheter ablation of left atrial arrhythmias. Am J Gastroenterol 105(3):551–556. https://doi.org/10.1038/ajg.2009.625
Zellerhoff S, Ullerich H, Lenze F, Meister T, Wasmer K, Monnig G et al (2010) Damage to the esophagus after atrial fibrillation ablation: just the tip of the iceberg? High prevalence of mediastinal changes diagnosed by endosonography. Circ Arrhythm Electrophysiol 3(2):155–159. https://doi.org/10.1161/CIRCEP.109.915918
Sami SS, Ragunath K (2013) The Los Angeles classification of gastroesophageal reflux disease. Video J Encyclopedia GI Endosc 1(1):103–104. https://doi.org/10.1016/S2212-0971(13)70046-3
Cordes F, Ellermann C, Dechering DG, Frommeyer G, Kochhauser S, Lange PS et al (2021) Pre-procedural proton pump inhibition is associated with fewer peri-oesophageal lesions after cryoballoon pulmonary vein isolation. Sci Rep 11(1):4728. https://doi.org/10.1038/s41598-021-83928-0
Kadado AJ, Akar JG, Hummel JP (2019) Luminal esophageal temperature monitoring to reduce esophageal thermal injury during catheter ablation for atrial fibrillation: a review. Trends Cardiovasc Med 29(5):264–271. https://doi.org/10.1016/j.tcm.2018.09.010
Meininghaus DG, Blembel K, Waniek C, Kruells-Muench J, Ernst H, Kleemann T et al (2021) Temperature Monitoring and temperature-driven irrigated radiofrequency energy titration do not prevent thermally-induced esophageal lesions in pulmonary vein isolation a randomized study controlled by esophagoscopy before and after catheter ablation. Heart Rhythm. https://doi.org/10.1016/j.hrthm.2021.02.003
Jacobs V, May HT, Crandall BG, Ballantyne B, Chisum B, Johnson D et al (2018) Vagus nerve injury symptoms after catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol 41(4):389–395. https://doi.org/10.1111/pace.13304
Martinek M, Hassanein S, Bencsik G, Aichinger J, Schoefl R, Bachl A et al (2009) Acute development of gastroesophageal reflux after radiofrequency catheter ablation of atrial fibrillation. Heart Rhythm 6(10):1457–1462. https://doi.org/10.1016/j.hrthm.2009.06.022
Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D’Ambra MN, Eltzschig HK (2010) Safety of transesophageal echocardiography. J Am Soc Echocardiogr 23(11):1115–1127. https://doi.org/10.1016/j.echo.2010.08.013
Pasricha PJ, Fleischer DE, Kalloo AN (1994) Endoscopic perforations of the upper digestive tract: a review of their pathogenesis, prevention, and management. Gastroenterology 106(3):787–802. https://doi.org/10.1016/0016-5085(94)90717-x
Sarairah SY, Woodbury B, Methachittiphan N, Tregoning DM, Sridhar AR, Akoum N (2019) Esophageal thermal injury following cryoballoon ablation for atrial fibrillation. JACC Clin Electrophysiol. https://doi.org/10.1016/j.jacep.2019.10.014
Cordes F, Ellermann C, Dechering DG, Frommeyer G, Kochhauser S, Lange PS et al (2019) Time-to-isolation-guided cryoballoon ablation reduces oesophageal and mediastinal alterations detected by endoscopic ultrasound: results of the MADE-PVI trial. Europace 21(9):1325–1333. https://doi.org/10.1093/europace/euz142
Ayoub T, El Hajjar AH, Singh Sidhu GD, Bhatnagar A, Zhang Y, Mekhael M et al (2022) Esophageal temperature during atrial fibrillation ablation poorly predicts esophageal injury: an observational study. Heart Rhythm O2. https://doi.org/10.1016/j.hroo.2021.11.002
Singh SM, d’Avila A, Singh SK, Stelzer P, Saad EB, Skanes A et al (2013) Clinical outcomes after repair of left atrial esophageal fistulas occurring after atrial fibrillation ablation procedures. Heart Rhythm 10(11):1591–1597. https://doi.org/10.1016/j.hrthm.2013.08.012
Han J, Good E, Morady F, Oral H (2004) Images in cardiovascular medicine. Esophageal migration during left atrial catheter ablation for atrial fibrillation. Circulation 110(24):e528. https://doi.org/10.1161/01.CIR.0000149750.18875.8C
Cochet H, Nakatani Y, Sridi-Cheniti S, Cheniti G, Ramirez FD, Nakashima T et al (2021) Pulsed field ablation selectively spares the oesophagus during pulmonary vein isolation for atrial fibrillation. Europace. https://doi.org/10.1093/europace/euab090
Levy I, Gralnek IM (2016) Complications of diagnostic colonoscopy, upper endoscopy, and enteroscopy. Best Pract Res Clin Gastroenterol 30(5):705–718. https://doi.org/10.1016/j.bpg.2016.09.00
Funding
RF was supported by the German Federal Ministry of Education and Research (Medical Informatics Initiative, 01ZZ1802A-Z, AB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, conduct and design. Material preparation, data collection and analysis were performed by Dirk Grosse Meininghaus and Robert Freund. The first draft of the manuscript was written by Dirk Grosse Meininghaus and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
JCG is a consultant for Abbott, Medtronic, Biotronik, Boston Scientific, Daiichi Sankyo, Pfizer, and has received speaker fees from AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Pfizer, Sanofi Aventis, Biotronik, Boston Scientific, Medtronic, and Abbott. The authors have no relevant financial or non-financial interests to disclose.
Rights and permissions
About this article
Cite this article
Grosse Meininghaus, D., Freund, R., Heimbaecher, L. et al. Incidence and clinical relevance of upper gastrointestinal pathology during preprocedural endoscopy in patients undergoing pulmonary vein isolation. Clin Res Cardiol 111, 1069–1076 (2022). https://doi.org/10.1007/s00392-022-02050-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-022-02050-x