Abstract
Background and purpose
The National Cardiovascular Data Registry (NCDR) risk scores for mortality, bleeding and acute kidney injury (AKI) are accurate outcome predictors of coronary catheterization procedures in North American populations. However, their application in German clinical practice remained elusive and we thus aimed to verify their use.
Methods
NCDR scores for mortality, bleeding and AKI and corresponding clinical outcomes were retrospectively assessed in patients undergoing catheterization for ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI) or for elective coronary procedures at a German Heart Center from 2014 to 2017. Risk model performance was assessed using receiver-operating-characteristic curves (discrimination) and graphical analysis/logistic regression (calibration).
Results
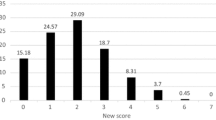
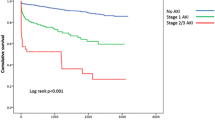
A total of 1637 patients were included, procedures were performed for STEMI (565 patients, 34.5%), NSTEMI (572 patients, 34.9%) and elective purposes (500 patients, 30.5%); 6% (13% of STEMI and 5% of NSTEMI patients) presented in cardiogenic shock and 3% with resuscitated cardiac arrest. Radial access was used in 38% of procedures and cross-over was necessary in 5%; PCI was performed in 60% of procedures. In-hospital mortality was 6.3% (STEMI 14.5%; NSTEMI 3.7%; elective 0%) and major bleedings occurred in 5.6% (STEMI 10.6%; NSTEMI 5.4%; elective 0.2%); AKI was detected in 18.1% of patients (STEMI 23.7%; NSTEMI 27.3%; elective 1.4%), amounting to KDIGO stage I/II/III in 11.5%/3.5%/3.2%. NCDR risk models discriminated very well for mortality [AUC 0.93 with 95% confidence interval (CI) 0.91–0.95] and well for major bleeding (AUC 0.82, CI 0.78–0.86) and any AKI (AUC 0.83, CI 0.81–0.86). Discrimination in the subgroup of patients with PCI was comparable (mortality: AUC 0.90; major bleeding: AUC 0.78; any AKI: AUC 0.79). However, calibration showed considerable underestimation of mortality and AKI in high-risk patients, while major bleeding was consistently overestimated (Hosmer–Lemeshow p < 0.02 for all outcomes).
Conclusions
The NCDR risk models showed excellent performance in discriminating high-risk from low-risk patients in contemporary German interventional cardiology. Model calibration for adverse event probability prediction, however, is limited and demands recalibration, especially in high-risk patients.
Graphic abstract



Similar content being viewed by others
Abbreviations
- AKI:
-
Acute kidney injury
- AUC:
-
Area-under-the-curve
- BARC:
-
Bleeding Academic Research Consortium
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CKD:
-
Chronic kidney disease
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- GFR:
-
Glomerular filtration rate
- N/A:
-
Not available
- NCDR:
-
National Cardiovascular Data Registry
- NSTEMI:
-
Non-ST-segment elevation myocardial infarction
- NYHA:
-
New York Heart Association
- PAD:
-
Peripheral artery disease
- PCI:
-
Percutaneous coronary intervention
- STEMI:
-
ST-segment elevation myocardial infarction
References
Block PC, Peterson ED, Krone R, Kesler K, Hannan E, O'Connor GT et al (1998) Identification of variables needed to risk adjust outcomes of coronary interventions: evidence-based guidelines for efficient data collection. J Am Coll Cardiol 32(1):275–282
Moscucci M, O'Connor GT, Ellis SG, Malenka DJ, Sievers J, Bates ER et al (1999) Validation of risk adjustment models for in-hospital percutaneous transluminal coronary angioplasty mortality on an independent data set. J Am Coll Cardiol 34(3):692–697
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H et al (2018) 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39(2):119–177
American College of Emergency P, Society for Cardiovascular A, Interventions, O'Gara PT, Kushner FG, Ascheim DD et al (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61(4):485–510
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F et al (2016) 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 37(3):267–315
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr et al (2014) 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130(25):e344–e426
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B et al (2011) 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 124(23):e574–e651
Authors/Task Force M, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J et al (2014) 2014 ESC/EACTS guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35(37):2541–2619
Brennan JM, Curtis JP, Dai D, Fitzgerald S, Khandelwal AK, Spertus JA et al (2013) Enhanced mortality risk prediction with a focus on high-risk percutaneous coronary intervention: results from 1,208,137 procedures in the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv 6(8):790–799
Peterson ED, Dai D, DeLong ER, Brennan JM, Singh M, Rao SV et al (2010) Contemporary mortality risk prediction for percutaneous coronary intervention: results from 588,398 procedures in the National Cardiovascular Data Registry. J Am Coll Cardiol 55(18):1923–1932
Rao SV, McCoy LA, Spertus JA, Krone RJ, Singh M, Fitzgerald S et al (2013) An updated bleeding model to predict the risk of post-procedure bleeding among patients undergoing percutaneous coronary intervention: a report using an expanded bleeding definition from the National Cardiovascular Data Registry CathPCI Registry. JACC Cardiovasc Interv 6(9):897–904
Tsai TT, Patel UD, Chang TI, Kennedy KF, Masoudi FA, Matheny ME et al (2014) Validated contemporary risk model of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the National Cardiovascular Data Registry Cath-PCI Registry. J Am Heart Assoc 3(6):e001380
Weintraub WS, Grau-Sepulveda MV, Weiss JM, Delong ER, Peterson ED, O'Brien SM et al (2012) Prediction of long-term mortality after percutaneous coronary intervention in older adults: results from the National Cardiovascular Data Registry. Circulation 125(12):1501–1510
Couto-Mallon D, Rodriguez-Garrido JL, Aldama-Lopez G, Calvino-Santos R, Pinon-Esteban P, Salgado-Fernandez J et al (2013) Validation of the National Cardiovascular Data Registry (NCDR) score for 30-day mortality prediction after Percutaneous Coronary Intervention (PCI) in a European cohort. Eur Heart J 34(suppl_1):P1220
Inohara T, Kohsaka S, Miyata H, Ueda I, Maekawa Y, Fukuda K et al (2016) Performance and validation of the US NCDR acute kidney injury prediction model in Japan. J Am Coll Cardiol 67(14):1715–1722
Timoteo AT, Monteiro AV, Portugal G, Teixeira P, Aidos H, Ferreira ML et al (2016) Validation of two US risk scores for percutaneous coronary intervention in a single-center Portuguese population of patients with acute coronary syndrome. Rev Port Cardiol 35(2):73–78
Wall JJS, Iqbal J, Andrews M, Teare D, Ghobrial M, Hinton T et al (2017) Development and validation of a clinical risk score to predict mortality after percutaneous coronary intervention. Open Heart 4(2):e000576
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J et al (2011) Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation 123(23):2736–2747
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL et al (2012) Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2(1):1–138. https://doi.org/10.1038/kisup.2012.1
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Pencina MJ, D'Agostino RB Sr (2015) Evaluating discrimination of risk prediction models: the C statistic. JAMA 314(10):1063–1064
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35
Hosmer DWJ, Lemeshow Sturdivant XR (2013) Applied logistic regression, 3rd edn. Wiley, Hoboken
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N et al (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21(1):128–138
DeFilippis AP, Young R, Carrubba CJ, McEvoy JW, Budoff MJ, Blumenthal RS et al (2015) An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med 162(4):266–275
Matheny ME, Ohno-Machado L, Resnic FS (2005) Discrimination and calibration of mortality risk prediction models in interventional cardiology. J Biomed Inform 38(5):367–375
Dobies DR, Barber KR, Cohoon AL (2015) Validity of a PCI Bleeding Risk Score in patient subsets stratified for body mass index. Open Heart 2(1):e000088
Stefanini GG, Holmes DR Jr (2013) Drug-eluting coronary-artery stents. N Engl J Med 368(3):254–265
Navarese EP, Andreotti F, Kolodziejczak M, Schulze V, Wolff G, Dias S et al (2015) Comparative efficacy and safety of anticoagulant strategies for acute coronary syndromes. Comprehensive network meta-analysis of 42 randomised trials involving 117,353 patients. Thromb Haemost 114(5):933–944
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S et al (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357(20):2001–2015
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361(11):1045–1057
Hohnloser SH, Basic E, Nabauer M (2017) Comparative risk of major bleeding with new oral anticoagulants (NOACs) and phenprocoumon in patients with atrial fibrillation: a post-marketing surveillance study. Clin Res Cardiol 106(8):618–628
Grotti S, Bolognese L (2017) Interventional cardiology is changing: demographic, clinical and economic considerations. J Cardiovasc Med (Hagerstown) 18(Suppl 1):e67–e70
Timmis A, Townsend N, Gale C, Grobbee R, Maniadakis N, Flather M et al (2018) European Society of Cardiology: cardiovascular disease statistics 2017. Eur Heart J 39(7):508–579
Valgimigli M, Gagnor A, Calabro P, Frigoli E, Leonardi S, Zaro T et al (2015) Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet 385(9986):2465–2476
Feldkamp T, Luedemann M, Spehlmann ME, Freitag-Wolf S, Gaensbacher J, Schulte K et al (2018) Radial access protects from contrast media induced nephropathy after cardiac catheterization procedures. Clin Res Cardiol 107(2):148–157
Funding
This work was supported by the Forschungskommission of the Medical Faculty of the Heinrich-Heine-University Düsseldorf (no. 2018-32 to GW).
Author information
Authors and Affiliations
Contributions
GW, MK and VS conceived and designed the study; JQ, SB and LK collected and analyzed data; GW and YL analyzed and interpreted data and drafted the manuscript; MB, AK, YH, CP, TK and SP supported data acquisition and analysis and critically revised the manuscript; MK, AI, AA and VS assumed project supervision, interpreted data and critically revised the manuscript. All authors read and accepted the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Rights and permissions
About this article
Cite this article
Wolff, G., Lin, Y., Quade, J. et al. Validation of National Cardiovascular Data Registry risk models for mortality, bleeding and acute kidney injury in interventional cardiology at a German Heart Center. Clin Res Cardiol 109, 235–245 (2020). https://doi.org/10.1007/s00392-019-01506-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01506-x