Abstract
Background
Data on preferred ICD lead type and optimal RV lead position in patients undergoing CRT-D implantation are limited.
Objectives
To compare dual- versus single-coil ICD leads and non-apical versus apical RV lead position and their impact on clinical parameters and survival in CRT-D recipients.
Methods
A total of 563 consecutive patients with advanced heart failure and indication for CRT-D implantation were enrolled in two European tertiary centers. Endpoints were improvement in NYHA functional class, changes in echo- and electrocardiographic parameters, and all-cause and cardiovascular mortality.
Results
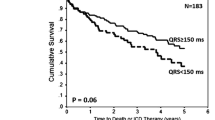
In this retrospective analysis, a total of 313 (56%) dual- and 250 (44%) single-coil ICD leads were used. RV leads were placed non-apically in 262 (47%) and apically in 296 (53%) patients, respectively. Over a mean follow-up of 41 ± 34 months, all-cause mortality and cardiovascular mortality were similar for patients with dual- versus single-coil ICD lead (adjusted HR 0.81, 95% CI 0.58–1.12 and aHR 1.22, 95% CI 0.73–2.04) and non-apical versus apical RV lead position (aHR 0.98, 95% CI 0.71–1.36 and aHR 0.76, 95% CI 0.44–1.31). Non-apical RV lead position was associated with greater reduction in QRS duration after CRT implantation (− 14.4 ± 32.1 vs. − 4.3 ± 34.3 ms, p < 0.001).
Conclusions
We found no association between ICD lead type or RV lead position and outcomes in CRT-D recipients. Non-apical RV lead position was associated with larger reduction in QRS duration.



Similar content being viewed by others
References
Cazeau S, Leclercq C, Lavergne T et al (2001) Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med 344:873–880. https://doi.org/10.1056/NEJM200103223441202
Abraham WT, Fisher WG, Smith AL et al (2002) Cardiac resynchronization in chronic heart failure. N Engl J Med 346:1845–1853. https://doi.org/10.1056/NEJMoa013168
Bristow MR, Saxon LA, Boehmer J et al (2004) Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 350:2140–2150. https://doi.org/10.1056/NEJMoa032423
Cleland JGF, Daubert J-C, Erdmann E et al (2005) The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 352:1539–1549. https://doi.org/10.1056/NEJMoa050496
Moss AJ, Hall WJ, Cannom DS et al (2009) Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med 361:1329–1338. https://doi.org/10.1056/NEJMoa0906431
Birnie DH, Ha A, Higginson L et al (2013) Impact of QRS morphology and duration on outcomes after cardiac resynchronization therapy: results from the resynchronization-defibrillation for ambulatory heart failure trial (RAFT). Circ Heart Fail 6:1190–1198. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000380
Gold MR, Daubert J-C, Abraham WT et al (2013) Implantable defibrillators improve survival in patients with mildly symptomatic heart failure receiving cardiac resynchronization therapy: analysis of the long-term follow-up of remodeling in systolic left ventricular dysfunction (REVERSE). Circulation 6:1163–1168. https://doi.org/10.1161/CIRCEP.113.000570
Stockburger M, Moss AJ, Klein HU et al (2016) Sustained clinical benefit of cardiac resynchronization therapy in non-LBBB patients with prolonged PR-interval: MADIT-CRT long-term follow-up. Clin Res Cardiol 105:944–952. https://doi.org/10.1007/s00392-016-1003-z
Franke J, Keppler J, Abadei AK et al (2016) Long-term outcome of patients with and without super-response to CRT-D. Clin Res Cardiol 105:341–348. https://doi.org/10.1007/s00392-015-0926-0
Kutyifa V, Cannom D, Klein HU, Moss AJ (2017) Discrepancies in the U.S. and European guidelines involving the implantable cardioverter-defibrillator and cardiac resynchronization therapy: need for a single shared international publication. Heart Rhythm 14:474–475. https://doi.org/10.1016/j.hrthm.2016.12.031
Tracy CM, Epstein AE, Darbar D et al (2012) 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 60:1297–1313. https://doi.org/10.1016/j.jacc.2012.07.009
Brignole M, Auricchio A, Baron-Esquivias G et al (2014) 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy. Rev Esp Cardiol 67:58. https://doi.org/10.1016/j.rec.2013.11.003
Hayes DL, Boehmer JP, Day JD et al (2011) Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm 8:1469–1475. https://doi.org/10.1016/j.hrthm.2011.04.015
Singh JP, Klein HU, Huang DT et al (2011) Left ventricular lead position and clinical outcome in the multicenter automatic defibrillator implantation trial-cardiac resynchronization therapy (MADIT-CRT) trial. Circulation 123:1159–1166. https://doi.org/10.1161/CIRCULATIONAHA.110.000646
Saxon LA, Olshansky B, Volosin K et al (2009) Influence of left ventricular lead location on outcomes in the COMPANION study. J Cardiovasc Electrophysiol 20:764–768. https://doi.org/10.1111/j.1540-8167.2009.01444.x
Khan FZ, Virdee MS, Palmer CR et al (2012) Targeted left ventricular lead placement to guide cardiac resynchronization therapy: the TARGET study: a randomized, controlled trial. J Am Coll Cardiol 59:1509–1518. https://doi.org/10.1016/j.jacc.2011.12.030
Thebault C, Donal E, Meunier C et al (2012) Sites of left and right ventricular lead implantation and response to cardiac resynchronization therapy observations from the REVERSE trial. Eur Heart J 33:2662–2671. https://doi.org/10.1093/eurheartj/ehr505
Gold MR, Olsovsky MR, Pelini MA, Peters RW, Shorofsky SR (1998) Comparison of single- and dual-coil active pectoral defibrillation lead systems. J Am Coll Cardiol 31(6):1391–1394
Bardy GH, Lee KL, Mark DB et al (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352:225–237. https://doi.org/10.1056/NEJMoa043399
Aoukar PS, Poole JE, Johnson GW et al (2013) No benefit of a dual coil over a single coil ICD lead: evidence from the Sudden Cardiac Death in Heart Failure Trial. Heart Rhythm 10:970–976. https://doi.org/10.1016/j.hrthm.2013.03.046
Sunderland N, Kaura A, Murgatroyd F, Dhillon P, Scott PA (2017) Outcomes with single-coil versus dual-coil implantable cardioverter defibrillators: a meta-analysis. Europace. https://doi.org/10.1093/europace/euw438
Wilkoff BL, Cook JR, Epstein AE et al (2002) Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial. JAMA 288(24):3115–3123
Curtis AB, Worley SJ, Adamson PB et al (2013) Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med 368:1585–1593. https://doi.org/10.1056/NEJMoa1210356
Shimony A, Eisenberg MJ, Filion KB, Amit G (2012) Beneficial effects of right ventricular non-apical vs. apical pacing: a systematic review and meta-analysis of randomized-controlled trials. Europace 14:81–91. https://doi.org/10.1093/europace/eur240
Amit G, Wang J, Connolly SJ et al (2016) Apical versus non-apical lead: is ICD lead position important for successful defibrillation? J Cardiovasc Electrophysiol 27:581–586. https://doi.org/10.1111/jce.12952
Healey JS, Hohnloser SH, Glikson M et al (2015) Cardioverter defibrillator implantation without induction of ventricular fibrillation: a single-blind, non-inferiority, randomised controlled trial (SIMPLE). Lancet 385:785–791. https://doi.org/10.1016/S0140-6736(14)61903-6
Riedlbauchova L, Cihak R, Bytesnik J et al (2006) Optimization of right ventricular lead position in cardiac resynchronisation therapy. Eur J Heart Fail 8:609–614. https://doi.org/10.1016/j.ejheart.2005.11.009
Khan FZ, Salahshouri P, Duehmke R et al (2011) The impact of the right ventricular lead position on response to cardiac resynchronization therapy. Pacing Clin Electrophysiol 34:467–474. https://doi.org/10.1111/j.1540-8159.2010.02995.x
Bulava A, Lukl J (2009) Similar long-term benefits conferred by apical versus mid-septal implantation of the right ventricular lead in recipients of cardiac resynchronization therapy systems. Pacing Clin Electrophysiol 32(Suppl 1):S32–S327. https://doi.org/10.1111/j.1540-8159.2008.02224.x
Kutyifa V, Bloch Thomsen PE, Huang DT et al (2013) Impact of the right ventricular lead position on clinical outcome and on the incidence of ventricular tachyarrhythmias in patients with CRT-D. Heart Rhythm 10:1770–1777. https://doi.org/10.1016/j.hrthm.2013.08.020
Kolb C, Solzbach U, Biermann J et al (2014) Safety of mid-septal electrode placement in implantable cardioverter defibrillator recipients–results of the SPICE (Septal Positioning of ventricular ICD Electrodes) study. Int J Cardiol 174:713–720. https://doi.org/10.1016/j.ijcard.2014.04.229
Leclercq C, Sadoul N, Mont L et al (2016) Comparison of right ventricular septal pacing and right ventricular apical pacing in patients receiving cardiac resynchronization therapy defibrillators: the SEPTAL CRT study. Eur Heart J 37:473–483. https://doi.org/10.1093/eurheartj/ehv422
Zografos TA, Siontis KC, Jastrzebski M et al (2015) Apical vs. non-apical right ventricular pacing in cardiac resynchronization therapy: a meta-analysis. Europace 17:1259–1266. https://doi.org/10.1093/europace/euv048
Kronborg MB, Johansen JB, Riahi S et al (2017) Association between right ventricular lead position and clinical outcomes in patients with cardiac resynchronization therapy. Europace. https://doi.org/10.1093/europace/euw424
Bryant AR, Wilton SB, Lai MP, Exner DV (2013) Association between QRS duration and outcome with cardiac resynchronization therapy: a systematic review and meta-analysis. J Electrocardiol 46:147–155. https://doi.org/10.1016/j.jelectrocard.2012.12.003
Iler MA, Hu T, Ayyagari S et al (2008) Prognostic value of electrocardiographic measurements before and after cardiac resynchronization device implantation in patients with heart failure due to ischemic or nonischemic cardiomyopathy. Am J Cardiol 101:359–363. https://doi.org/10.1016/j.amjcard.2007.08.043
Acknowledgements
The assistance of Antje Steidl is greatly appreciated by the authors. We thank Prof. Eva Herrmann for her advice in the statistical part of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alexander P. Benz reports support to attend a scientific meeting from St. Jude Medical/Abbott. Mate Vamos reports lecture fees from Bayer, Pfizer and Spectranetics and support to attend scientific meetings from Bayer, Boston Scientific, Pfizer, and SJM, outside the submitted work. Julia W. Erath reports receiving lecture fees and support to attend scientific meetings from Zoll Medical and Servier, and is a fellow of the Boston Scientific heart rhythm fellowship program, outside the submitted work. Peter Bogyi has nothing to report. Gabor Z. Duray received lecture and consulting fees from Medtronic, Biotronik, SJM, and Johnson&Johnson, outside the submitted work. Stefan H. Hohnloser received consulting fees Bayer, BI, Boston Scientific, BMS, Cardiome, Gilead, J&J, Medtronic, Pfizer, SJM, Sanofi-Aventis, and Zoll Medical, outside the submitted work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Benz, A.P., Vamos, M., Erath, J.W. et al. ICD lead type and RV lead position in CRT-D recipients. Clin Res Cardiol 107, 1122–1130 (2018). https://doi.org/10.1007/s00392-018-1286-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1286-3