Abstract
Aims
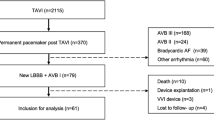
Approximately every fifth patient undergoing transcatheter aortic valve implantation (TAVI) requires a permanent pacemaker (PPM) after the procedure. The aim of this study was to analyse predictors of atrioventricular block III° (AVBIII) persistence with concurrent PPM dependency after TAVI.
Methods and results
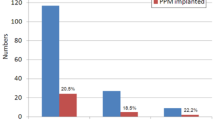
Between 2010 and 2015 a total of 1198 patients underwent TAVI at the Kerckhoff Heart and Thorax Center, Germany. After exclusion of patients with prior PPM (n = 173) 14.7% (n = 176) of the patients underwent PPM implantation after the procedure. Independent predictors of PPM implantation were pre-existing right bundle branch block (RBBB, p < 0.001) and implantation of a CoreValve prosthesis (p < 0.001). A subgroup of patients with a newly implanted PPM (n = 102) were followed-up for a median of 73 (IQR 62–85) days. The leading indication for PPM implantation was AVBIII in 74.5% (76/102). Of these patients only 22.4% (17/76) had persistent AVBIII at follow-up. Predictors of AVBIII persistence were prior RBBB (p = 0.04), postdilatation (p = 0.006) and higher mean aortic valve gradient prior to implantation (p = 0.013). PPMs were implanted earlier in patients with persisting AVBIII [1 day (IQR0–2.5) vs. 4 days (IQR2–7); p < 0.001]. Early PPM implantation after TAVI was the only independent predictor of persistent AVBIII [OR 1.36 (95% 1.05–1.75); p = 0.02].
Conclusion
The long-term persistence of AVBIII is generally low after TAVI. Therefore, it may be wise to postpone the indication for PPM implantation for a couple of days. The only predictors of a lack of recovery of the AVB are prior RBBB, higher mean aortic valve gradients and postdilatation of the prosthesis.





Similar content being viewed by others
References
Smith C, Leon M, Mack M et al (2011) Transcatheter versus surgical aotic-valve replacement in high-risk patients. N Engl J Med 364:2187–2198
Leon M, Smith C, Mack M et al (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Gaede L, Möllmann H (2015) Transcatheter aortic valve implantation (TAVI): current perspectives. Herz 54:742–751
Gaede L, Kim W-K, Blumenstein J et al (2017) Temporal trends in transcatheter and surgical aortic valve replacement. Herz 42:316–324
Gaede L, Blumenstein J, Kim W-K et al (2017) Trends in aortic valve replacement in Germany in 2015: transcatheter versus isolated surgical aortic valve repair. Clin Res Cardiol 106:411–419
Möllmann H, Bestehorn K, Bestehorn M et al (2016) In-hospital outcome of transcatheter vs. surgical aortic valve replacement in patients with aortic valve stenosis—complete dataset of patients treated in 2013 in Germany. Clin Res Cardiol 105:553–559
Doenst T, Strüning C, Moschovas A et al (2016) Cardiac surgery 2015 reviewed. Clin Res Cardiol 105:801–814
Seidler T, M H, Puls M et al (2016) Feasibility and outcomes of interventional treatment for vascular access site complications following transfemoral aortic valve implantation. Clin Res Cardiol 106:183–191
Arsalan M, Filardo G, Kim WK et al (2016) Prognostic value of body mass index and body surface area on clinical outcomes after transcatheter aortic valve implantation. Clin Res Cardiol 105:1042–1048
Erkapic D, De Rosa S, Kelava A et al (2012) Risk for permanent pacemaker after transcatheter aortic valve implantation: a comprehensive analysis of the literature. J Cardiovasc Electrophysiol 23:391–397
Walther T, Hamm CW, Schuler G et al (2015) Peri-operative results and complications in 15,964 transcatheter aortic valve implantations from the German Aortic valve RegistrY (GARY). J Am Coll Cardiol 65:2173–2180
Leon MB, Smith CR, Mack MJ et al (2016) Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med NEJM 374:1609–1620
Reardon MJ, Van Mieghem NM, Popma JJ et al (2017) Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med 376:1321–1331
Mohr FW, Holzhey D, Möllmann H et al (2014) The German Aortic Valve Registry: 1-year results from 13,680 patients with aortic valve disease†. Eur J cardio-thoracic Surg 46:808–816
Fraccaro C, Buja G, Tarantini G et al (2011) Incidence, predictors, and outcome of conduction disorders after transcatheter self-expandable aortic valve implantation. Am J Cardiol 107:747–754
Nazif TM, Dizon JM, Hahn RT et al (2015) Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement. JACC Cardiovasc Interv 8:60–69
Urena M, Rodés-Cabau J (2015) Permanent pacemaker implantation following transcatheter aortic valve replacement. JACC Cardiovasc Interv 8:70–73
Schymik G, Tzamalis P, Bramlage P et al (2015) Retro Clinical impact of a new left bundle branch block following TAVI implantation: 1-year results of the TAVIK cohort. Clin Res Cardiol 104:351–362
Gonska B, Seeger J, Keßler M et al (2017) Predictors for permanent pacemaker implantation in patients undergoing transfemoral aortic valve implantation with the Edwards Sapien 3 valve. Clin Res Cardiol. doi:10.1007/s00392-017-1093-2 (epub ahead of print)
Kempfert J, Meyer A, Kim W-K et al (2016) Comparison of two valve systems for transapical aortic valve implantation: a propensity score-matched analysis. Eur J Cardio Thoracic Surg 49:486–492
Kim W-K, Rolf A, Liebetrau C et al (2014) Detection of myocardial injury by CMR after transcatheter aortic valve replacement. J Am Coll Cardiol 64:349–357
Möllmann H, Kim W-K, Kempfert J et al (2014) Transfemoral aortic valve implantation of edwards SAPIEN XT without predilatation is feasible. Clin Cardiol 37:667–671
Walther T, Möllmann H, van Linden A, Kempfert J (2011) Transcatheter aortic valve implantation transapical: step by step. Semin Thorac Cardiovasc Surg 23:55–61
Möllmann H, Kempfert J, Hamm CW, Walther T (2010) Transcatheter aortic valve implantation. Herz 35:62–68
Abdel-Wahab M, Mehilli J, Frerker C et al (2014) Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement. JAMA 311:1503–1514
Ramazzina C, Knecht S, Jeger R et al (2014) Pacemaker implantation and need for ventricular pacing during follow-up after transcatheter aortic valve implantation. Pacing Clin Electrophysiol 37:1592–1601
Boerlage -VAN, Dijk K, Kooiman KM, Yong ZY et al (2014) Predictors and permanency of cardiac conduction disorders and necessity of pacing after transcatheter aortic valve implantation. Pacing Clin Electrophysiol 37:1520–1529
Jilaihawi H, Chin D, Vasa-Nicotera M et al (2009) Predictors for permanent pacemaker requirement after transcatheter aortic valve implantation with the CoreValve bioprosthesis. Am Heart J 157:860–866
van der Boon RMA, Van Mieghem NM, Theuns DA et al (2013) Pacemaker dependency after transcatheter aortic valve implantation with the self-expanding Medtronic CoreValve System. Int J Cardiol 168:1269–1273
Urena M, Webb JG, Tamburino C et al (2014) Permanent pacemaker implantation after transcatheter aortic valve implantation: impact on late clinical outcomes and left ventricular function. Circulation 129:1233–1243
Urena M, Rodés-cabau J, Hospital BB, Heart Q (2015) EuroIntervention Managing heart block after transcatheter aortic valve implantation: from monitoring to device selection and pacemaker indications. EuroIntervention 11:W101–W105
Brignole M, Auricchio A, Baron-Esquivias G et al (2013) 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association. Eur Heart J 34:2281–2329
van der Boon RM, Nuis R-J, Van Mieghem NM et al (2012) New conduction abnormalities after TAVI-frequency and causes. Nat Rev Cardiol 9:454–463
Kindermann M, Hennen B, Jung J et al (2006) Biventricular versus conventional right ventricular stimulation for patients with standard pacing indication and left ventricular dysfunction. J Am Coll Cardiol 47:1927–1937
Chan JYS, Fang F, Zhang Q et al (2011) Biventricular pacing is superior to right ventricular pacing in bradycardia patients with preserved systolic function: 2-year results of the PACE trial. Eur Heart J 32:2533–2540
Stockburger M, Gomez-Doblas JJ, Lamas G et al (2011) Preventing ventricular dysfunction in pacemaker patients without advanced heart failure: results from a multicentre international randomized trial (PREVENT-HF). Eur J Heart Fail 13:633–641. doi:10.1093/eurjhf/hfr041
Acknowledgements
We thank Elizabeth Martinson, Ph.D., of the KHFI Editorial Office for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The ethics board of the state of Hessen, Germany, approved the study (FF 87/2010), which complies with the Declaration of Helsinki.
Conflict of interest
Helge Möllmann received speaker honoraria and/or travel grants from Edwards Lifesciences, St. Jude Medical, Boston Scientific (former Symetis SA). Luise Gaede and Johannes Blumenstein received travel grants from Edwards Lifesciences, St. Jude Medical, Boston Scientific (former Symetis SA). Won Keun Kim is a proctor for St. Jude Medical and Boston Scientific (former Symetis SA). Christian Hamm is part of the Medtronic Advisory Board. Johannes Sperzel received lecture honoria from Abbott and Zoll. All other authors have no conflict of interest regarding the submitted work.
Rights and permissions
About this article
Cite this article
Gaede, L., Kim, WK., Liebetrau, C. et al. Pacemaker implantation after TAVI: predictors of AV block persistence. Clin Res Cardiol 107, 60–69 (2018). https://doi.org/10.1007/s00392-017-1158-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1158-2