Abstract
Background
Extensive evidence relating to transcatheter aortic valve replacement (TAVR) has accumulated in recent years, but mid-term outcomes are less reported. We investigated 996 patients after implantation of the CoreValve prosthesis for severe aortic stenosis in a real-world setting.
Objective
To report clinical and echocardiographic 3-year results from the ADVANCE study.
Methods
ADVANCE is a prospective, multicenter, fully monitored, nonrandomized clinical study. This analysis assessed valve-related events, predictors of early and mid-term mortality after TAVR, and systolic and diastolic prosthesis performance over 3 years.
Results
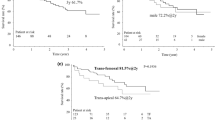
Three years after TAVR, the rate of major adverse cardiac/cerebrovascular events was 38.5%. All-cause mortality was 33.7%; cardiovascular mortality, 22.3%; VARC-1 stroke, 6.5%; and New York Heart Association class III/IV, 19.5%. Mean effective orifice area was consistently 1.7 cm2 from discharge to 3 years, and average mean aortic valve gradient remained ≤10 mmHg. At 3 years, 12.6% of patients had moderate and none had severe paravalvular regurgitation. Multivariable analysis identified Society of Thoracic Surgeons (STS) score, device migration, prior atrial fibrillation, and major vascular complication as predictors of early mortality. Predictors of mid-term mortality included male gender, STS score, history of chronic obstructive pulmonary disease, history of cancer, stroke, life-threatening/disabling or major bleeding, and valve deterioration.
Conclusions
Our 3-year data demonstrate significant hemodynamic benefits and durable symptom relief after CoreValve prosthesis implantation. Postprocedural patient management should be carefully considered, since postprocedural valve-related events were identified as independent predictors of mid-term mortality.
Trial registration
ClinicalTrials.gov, NCT01074658.





Similar content being viewed by others
Change history
04 July 2017
An erratum to this article has been published.
References
van Miegham N, Gerckens U, Modine T et al (2015) First report from the RESPOND study: post-market evaluation of a fully repositionable and retrievable aortic valve in 250 patients treated in routine clinical practice. In: Paper presented at the EuroPCR annual meeting, Paris, 19–22 May 2015
Husser O, Pellegrini C, Kessler T et al (2015) Outcomes after transcatheter aortic valve replacement using a novel balloon-expandable transcatheter heart valve: a single-center experience. JACC Cardiovasc Interv 8(14):1809–1816. doi:10.1016/j.jcin.2015.08.014
Manoharan G, Walton AS, Brecker SJ et al (2015) Treatment of symptomatic severe aortic stenosis with a novel resheathable supra-annular self-expanding transcatheter aortic valve system. JACC Cardiovasc Interv 8(10):1359–1367. doi:10.1016/j.jcin.2015.05.015
Tsai MT, Tang GH, Cohen GN (2016) Year in review: transcatheter aortic valve replacement. Curr Opin Cardiol 31(2):139–147. doi:10.1097/HCO.0000000000000260
Linke A, Wenaweser P, Gerckens U et al (2014) Treatment of aortic stenosis with a self-expanding transcatheter valve: the international multi-centre ADVANCE study. Eur Heart J 35(38):2672–2684. doi:10.1093/eurheartj/ehu162
Leon MB, Piazza N, Nikolsky E et al (2011) Standardized endpoint definitions for transcatheter aortic valve implantation clinical trials: a consensus report from the Valve Academic Research Consortium. J Am Coll Cardiol 57(3):253–269. doi:10.1016/j.jacc.2010.12.005
Zoghbi WA, Chambers JB, Dumesnil JG et al (2009) Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J Am Soc Echocardiogr 22(9):975–1014. doi:10.1016/j.echo.2009.07.013 (quiz 1082–1014)
Deeb GM, Reardon MJ, Chetcuti S et al (2016) Three-year outcomes in high-risk patients who underwent surgical or transcatheter aortic valve replacement. J Am Coll Cardiol 67(22):2565–2574. doi:10.1016/j.jacc.2016.03.506
Kapadia SR, Tuzcu EM, Makkar RR et al (2014) Long-term outcomes of inoperable patients with aortic stenosis randomized to transcatheter aortic valve replacement or standard therapy. Circulation. doi:10.1161/circulationaha.114.009834
Thourani VH (2013) Three-year outcomes after transcatheter or surgical aortic valve replacement in high-risk patients with severe aortic stenosis. In: Presented at: American College of Cardiology annual scientific sessions, San Francisco, 11 March 2013
Sinning JM, Petronio AS, Van Mieghem N et al (2017) Relation between clinical best practices and 6-month outcomes after transcatheter aortic valve implantation with CoreValve (from the ADVANCE II Study). Am J Cardiol 119(1):84–90. doi:10.1016/j.amjcard.2016.09.016
Petronio AS, Sinning JM, Van Mieghem N et al (2015) Optimal implantation depth and adherence to guidelines on permanent pacing to improve the results of transcatheter aortic valve replacement with the Medtronic CoreValve System: the CoreValve prospective, International Post-Market ADVANCE-II Study. JACC Cardiovasc Interv 8(6):837–846. doi:10.1016/j.jcin.2015.02.005
Bleiziffer S, Mazzitelli D, Opitz A et al (2012) Beyond the short-term: clinical outcome and valve performance 2 years after transcatheter aortic valve implantation in 227 patients. J Thorac Cardiovasc Surg 143(2):310–317. doi:10.1016/j.jtcvs.2011.10.060
Barbanti M, Schiltgen M, Verdoliva S et al (2016) Three-year outcomes of transcatheter aortic valve implantation in patients with varying levels of surgical risk (from the CoreValve ADVANCE study). Am J Cardiol 117(5):820–827. doi:10.1016/j.amjcard.2015.11.066
Duncan A, Ludman P, Banya W et al (2015) Long-term outcomes after transcatheter aortic valve replacement in high-risk patients with severe aortic stenosis: the U.K. Transcatheter Aortic Valve Implantation Registry. JACC Cardiovasc Interv 8(5):645–653. doi:10.1016/j.jcin.2015.01.009
Ussia GP, Barbanti M, Petronio AS et al (2012) Transcatheter aortic valve implantation: 3-year outcomes of self-expanding CoreValve prosthesis. Eur Heart J 33(8):969–976. doi:10.1093/eurheartj/ehr491
Gilard M, Eltchaninoff H, Donzeau-Gouge P et al (2016) Late outcomes of transcatheter aortic valve replacement in high-risk patients: the FRANCE-2 registry. J Am Coll Cardiol 68(15):1637–1647. doi:10.1016/j.jacc.2016.07.747
Barbanti M, Petronio AS, Ettori F et al (2015) 5-year outcomes after transcatheter aortic valve implantation with CoreValve prosthesis. JACC Cardiovasc Interv 8(8):1084–1091. doi:10.1016/j.jcin.2015.03.024
Tamburino C, Capodanno D, Ramondo A et al (2011) Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation 123(3):299–308. doi:10.1161/circulationaha.110.946533
Arnold SV, Reynolds MR, Lei Y et al (2014) Predictors of poor outcomes after transcatheter aortic valve replacement: results from the PARTNER (Placement of Aortic Transcatheter Valve) trial. Circulation 129(25):2682–2690. doi:10.1161/circulationaha.113.007477
Rodes-Cabau J, Webb JG, Cheung A et al (2012) Long-term outcomes after transcatheter aortic valve implantation: insights on prognostic factors and valve durability from the Canadian multicenter experience. J Am Coll Cardiol 60(19):1864–1875. doi:10.1016/j.jacc.2012.08.960
Moat NE, Ludman P, de Belder MA et al (2011) Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U.K. TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J Am Coll Cardiol 58(20):2130–2138. doi:10.1016/j.jacc.2011.08.050
Pilgrim T, Kalesan B, Wenaweser P et al (2012) Predictors of clinical outcomes in patients with severe aortic stenosis undergoing TAVI: a multistate analysis. Circ Cardiovasc Interv. doi:10.1161/circinterventions.112.974899
Thomas M, Schymik G, Walther T et al (2011) One-year outcomes of cohort 1 in the Edwards SAPIEN Aortic Bioprosthesis European Outcome (SOURCE) registry: the European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation 124(4):425–433. doi:10.1161/circulationaha.110.001545
Green P, Woglom AE, Genereux P et al (2012) The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single-center experience. JACC Cardiovasc Interv 5(9):974–981. doi:10.1016/j.jcin.2012.06.011
Saia F, Latib A, Ciuca C et al (2014) Causes and timing of death during long-term follow-up after transcatheter aortic valve replacement. Am Heart J 168(5):798–806. doi:10.1016/j.ahj.2014.07.023
Hermiller JB Jr, Yakubov SJ, Reardon MJ et al (2016) Predicting early and late mortality after transcatheter aortic valve replacement. J Am Coll Cardiol 68(4):343–352. doi:10.1016/j.jacc.2016.04.057
Rodes-Cabau J, Webb JG, Cheung A et al (2010) Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk: acute and late outcomes of the multicenter Canadian experience. J Am Coll Cardiol 55(11):1080–1090. doi:10.1016/j.jacc.2009.12.014
Dewey TM, Brown DL, Herbert MA et al (2010) Effect of concomitant coronary artery disease on procedural and late outcomes of transcatheter aortic valve implantation. Ann Thorac Surg 89(3):758–767. doi:10.1016/j.athoracsur.2009.12.033 (discussion 767)
Bosmans J, Bleiziffer S, Gerckens U et al (2015) The incidence and predictors of early- and mid-term clinically relevant neurological events after transcatheter aortic valve replacement in real-world patients. J Am Coll Cardiol 66(3):209–217. doi:10.1016/j.jacc.2015.05.025
Mack MJ, Leon MB, Smith CR et al (2015) 5-Year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385(9986):2477–2484. doi:10.1016/S0140-6736(15)60308-7
Popma JJ, Adams DH, Reardon MJ et al (2014) Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol 63(19):1972–1981. doi:10.1016/j.jacc.2014.02.556
Hahn RT, Pibarot P, Stewart WJ et al (2013) Comparison of transcatheter and surgical aortic valve replacement in severe aortic stenosis: a longitudinal study of echo parameters in cohort A of the PARTNER trial. J Am Coll Cardiol 61(25):2514–2521. doi:10.1016/j.jacc.2013.02.087
Van Belle E, Juthier F, Susen S et al (2014) Postprocedural aortic regurgitation in balloon-expandable and self-expandable transcatheter aortic valve replacement procedures: analysis of predictors and impact on long-term mortality: insights from the FRANCE2 Registry. Circulation 129(13):1415–1427. doi:10.1161/CIRCULATIONAHA.113.002677
Kodali SK, Williams MR, Smith CR et al (2012) Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 366(18):1686–1695. doi:10.1056/NEJMoa1200384
Lemos PA, Saia F, Mariani J Jr et al (2012) Residual aortic regurgitation is a major determinant of late mortality after transcatheter aortic valve implantation. Int J Cardiol 157(2):288–289. doi:10.1016/j.ijcard.2012.03.099
Athappan G, Patvardhan E, Tuzcu EM et al (2013) Incidence, predictors and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol. doi:10.1016/j.jacc.2013.01.047
Acknowledgements
This study was funded by Medtronic. The authors thank Medtronic employees Francesca Barbieri, MD, PhD, Maarten Hollander, MSc, and Hanne Gonnissen, PhD, for study management responsibilities, Jia Guo, PhD, for statistical support, and Julie Linick, ELS, CMPP, and Jessica Dries-Devlin, PhD, for editorial assistance and preparation of figures and tables. In addition, they thank Sarah Verdoliva, MS, of NAMSA, for completion of statistical analyses.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Dr. Bleiziffer has served as a consultant and proctor for Medtronic, a proctor for JenaValve, a proctor for Boston Scientific, and has received travel expenses from Medtronic. Dr. Bosmans serves as a proctor for Medtronic. Dr. Brecker has received consultant fees from Medtronic and Boston Scientific. Dr. Gerckens has received consulting and lecture fees and study-related travel expenses from Medtronic and Edwards Lifesciences, and serves as a proctor for Medtronic and Boston Scientific. Dr. Wenaweser has received consulting fees from Medtronic and Edwards Lifesciences, and has received remuneration from Medtronic for study-related travel and for development of educational materials. Dr. Tamburino has no relevant relationships to disclose. Dr. Linke has received speaker honoraria or served as a consultant for the following companies: Medtronic, St. Jude Medical, Claret Medical Inc., Boston Scientific, Edwards Lifesciences, Symetis, and Bard, and holds stock options from Claret Medical Inc. In addition, he received grant support from Medtronic and Claret Medical Inc.
Additional information
The original version of this article was revised: The sentence in the Discussion describing the new pacemaker rate was incorrect. The correct version of the sentence is: The new pacemaker rate at 3 years of 31.4% is slightly higher than the 28% reported in the CoreValve US Pivotal High Risk Trial [8], and considerably higher than that reported with balloon-expanding devices [9,10].
In the Limitations, the sentence describing echocardiographic follow-up was incorrect. The correct sentence is: Echocardiographic compliance was 67%, as reported in the Results section.
An erratum to this article is available at https://doi.org/10.1007/s00392-017-1124-z.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bleiziffer, S., Bosmans, J., Brecker, S. et al. Insights on mid-term TAVR performance: 3-year clinical and echocardiographic results from the CoreValve ADVANCE study. Clin Res Cardiol 106, 784–795 (2017). https://doi.org/10.1007/s00392-017-1120-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1120-3