Summary
Background
The objective of this paper was to analyze demographic and clinical characteristics of diabetic patients undergoing coronary artery bypass grafting on the basis of a significant number of cases.
Methods
The data of 8,195 patients who have undergone coronary bypass operations between 1996 and 2003 were analyzed. Non-diabetic patients (no DM), oral treated diabetics (DM oral) and insulin-treated diabetics (DM insulin) were compared in terms of their pre-operative, intra-operative and post-operative characteristics. The statistical analyses were performed with the support of SPSS 11.5 under application of chi-square and student-t tests.
Results
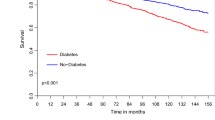
In cardiosurgery, diabetics differ in various ways from non-diabetic patients. They show a significantly higher prevalence of the known cardiovascular risk factors such as raised body mass index, age and hypertension. Furthermore they present a higher prevalence of vascular comorbidity such as peripheral vascular disease and carotid disease. At the postoperative stage, cerebral dysfunction occurred more often among the diabetic patients (no DM 5.2% vs. DM oral 7.3% vs. DM insulin 10.5%; p<0.05), they suffered from apoplexies more frequently (no DM 1.9% vs. DM oral 2.1% vs. DM insulin 3.2%; p<0.05), and they required re-intubation more frequently (no DM 2.6% vs. DM oral 3.1% vs. DM insulin 5.6%; p<0.05). Peri-operative mortality was highest in the group of insulin-treated diabetics (no DM 1.1% vs. DM oral 1.6% vs. DM insulin 1.8%; p<0.05).
Conclusion
In coronary surgery, diabetic patients represent an especially challenging patient group with an independent risk profile, who require specific consideration as far as the selection of the operative approach, on, one hand, and the post-operative follow-up, on the other hand, are concerned.
Zusammenfassung
Einleitung
Anhand eines aussagekräftigen Patientenkollektivs sollten die demographischen, klinischen, operativen und postoperativen Daten diabetischer Koronarpatienten mit nichtdiabetischen Patienten verglichen werden.
Methoden und Ergebnisse
Es wurden die Daten von 8 195 Patienten untersucht, die sich im Zeitraumvon 1996 bis 2002 koronaren Bypassoperationen unterzogen. Nichtdiabetische Patienten (kein DM), mit oralen Antidiabetika therapierte Diabetiker (DM oral) und mit Insulin therapierte Diabetiker (DM Insulin) wurden hinsichtlich ihrer präoperativen Charakteristika und Risikofaktoren und hinsichtlich der Ergebnisse des postoperativen Verlaufs miteinander verglichen. Es zeigte sich, dass diabetische Koronarpatienten signifikant häufiger zahlreiche kardiovaskuläre Risikofaktoren und eine höhere vaskuläre Komorbidität aufwiesen als nichtdiabetische Patienten. Postoperativ litten Diabetiker häufiger unter Verwirrtheitszuständen (kein DM 5,2% vs. DM oral 7,3% vs. DM Insulin 10,5%; p<0,05), erlitten häufiger Schlaganfälle (kein DM 1,9% vs. DM oral 2,1% vs. DM Insulin 3,2%; p<0,05) und mussten häufiger reintubiert werden (kein DM 2,6% vs. DM oral 3,1% vs. DM Insulin 5,6%; p<0,05). Die 30-Tage-Mortalität war unter den Diabetikern signifikant erhöht (kein DM 1,1% vs. DM oral 1,6% vs. DM Insulin 1,8%; p<0,05).
Schlussfolgerung
Die Ergebnisse der vorliegenden Studie zeigen, dass diabetische Koronarpatienten in der Herzchirurgie ein eigenständiges Risikoprofil aufweisen, das in der Wahl der operativen Strategien und im postoperativen Verlauf eine besondere Herausforderung darstellt.
Similar content being viewed by others
References
Abramov D, Tamariz MG, Fremes SE, Guru V, Borger MA, Christakis GT, Bhatnagar G, Sever JY, Goldman BS (2000) Trends in coronary artery bypass surgery results: a recent 9-year study. Ann Thorac Surg 70:84–90
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH (2002) Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol 40(3):418–423
Cohen Y, Raz I, Merin G, Mozes B (1998) Comparison of factors associated with 30-day mortality after coronary artery bypass grafting in patients with versus without diabetes mellitus. Am J Cardiol 81:7–11
Detre KM, Lombardero MS, Brooks MM, et al (2000) The effect of previous coronary-artery bypass surgery on the prognosis of patients with diabetes who have acute myocardial infarction. N Engl J Med 342:989–997
Endo M, Tomzawa Y, Nishida H (2003) Bilateral versus unilateral mammary revascularization in patients with diabetes. Circulation 108:1343–1349
Furnary AP, Zerr KJ, Grunkemeier GL, Starr A (1999) Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg 67:352–360
Garcia MJ, McNamara PM, Gordon T, Kannel WB (1974) Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up. Diabetes 23:105–111
Goldberg RB, Mellies MJ, Sacks FM, Moyé LA, Howard BV, Howard WJ, Davis BR, Cole TG, Pfeffer MA, Braunwald E (1998) Cardiovascular Events and Their Reduction With Pravastatin in Diabetic and Glucose-Intolerant Myocardial Infarction Survivors With Average Cholesterol Levels: Subgroup Analyses in the Cholesterol And Recurrent Events (CARE) Trial Circulation 98:2513–2519
Goldman MD (2003) Lung dysfunction in diabetes. Diabetes Care 26:1915–1918
Grimble RF (2002) Inflammatory status and insulin resistance. Curr Opin Clin Nutr Metab Care 5:551–559
Grossi EA, Esposito R, Harris LJ, et al (1991) Sternal wound infections and use of internal mammary artery grafts. J Thorac Cardiovasc Surg 102(3):342–346; discussion 346–347
He GW, Ryan WH, Acuff TE, et al (1994) Risk factors for operative mortality and sternal wound infection in bilateral internal mammary artery grafting. J Thorac Cardiovasc Surg. 107(1):196–202
Jacoby RM, Nesto RW (1992) Acute myocardial infarction in the diabetic patient: pathophysiology, clinical course and prognosis. J Am Coll Cardiol 20:736–744
Kannel WB, McGee DL (1979) Diabetes and cardiovascular risk factors: the Framingham Study. Circulation 59:8–13
Koenig W (2002) Insulin resistance, heart disease and inflammation. Identifying the “at risk” patient: the earlier the better? The role of inflammatory markers. Int J Clin Pract Supp 132:23–30
Kramer L, Fasching P, Madl C, et al (1998) Previous episodes of hypoglycemic coma are not associated with permanent cognitive brain dysfunction in IDDM patients on intensive insulin treatment. Diabetes 47:1909–1914
Lev-Ran O, Braunstein R, Nesher N, Ben-Gal Y, Bolotin G, Uretzky G. (2004) Bilateral versus single internal thoracic artery grafting in oral-treated diabetic subsets: comparative seven-year outcome analysis. Ann Thorac Surg 77(6):2039–2045
Morris JJ, Smith LR, Jones RH, et al (1991) Influence of diabetes and mammary artery grafting on survival after coronary bypass. Circulation 84(Suppl 3):275–284
Nashef SAM, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. the EuroSCORE study group (1999) European system for cardiac operative risk evaluation (Euro-SCORE). Eur J Cardio-thorac Surg 16:9–13
Newman MF, Wolman R, Kanchuger M, et al (1996) Multicenter preoperative stroke risk index for patients undergoing coronary artery bypass graft surgery. Multicenter Study of Perioperative Ischemia (McSPI) Research Group. Circulation 94(9 Suppl):II74–80
Peduzzi P, Detre K, Murphy ML, Thomsen J, Hultgren H, Takaro T (1991) Ten-year incidence of myocardial infarction and prognosis after infarction. Department of Veterans Affairs Cooperative Study of Coronary Artery Bypass Surgery. Circulation 83(3):747–755
Pozzessere G, Valle E, De Crignis S, et al (1991) Abnormalities of cognitive function in IDDM revealed by P300 event-related potential analysis. Diabetes 40:952–958
Roach GW, Kanchuger M, Mangano CM, et al (1996) Adverse cerebral outcomes after coronary bypass surgery. N Engl J Med 335:1857–1863
Sinisalo J, Paronen J, Mattila KJ et al (2000) Relation of inflammation to vascular function in patients with coronary heart disease. Artherosclerosis 149:403–411
Stamler J, Vaccaro O, Neaton JD, Wentworth D (1993) Diabetes, other risk factors, and 12 year cardiovascular mortality for men screened in the multiple rsik factor intervention trial. Diabetes Care 16:434–444
The Bypass Angioplasty Revascularization Investigation (BARI) Investigators (1997) Influence of diabetes on 5-year mortality and morbidity in a randomized trial comparing CABG and PTCA in patients with multivessel disease: the Bypass Angioplasty Revascularization Investigation. Circulation 96:1761–1769
Thourani VH, Weintraub WS, Stein B, et al (1999). Influence of diabetes mellitus on early and late outcome after coronary artery bypass grafting. Ann Thorac Surg 67:1045–1052
Weintraub WS, Wenger NK, Jones EL, Craver JM, Guyton RA (1993) Changing clinical characteristics of coronary surgery patients. Differences between men and women. Circulation 88:79–86
Weynand B, Jonckheere A, Frans A, Rahier J (1999) Diabetes mellitus induces a thickening of the pulmonary basal lamina. Respiration 66:14–19
Zarich S, Waxman S, Freeman RT, Mittleman M, Hegarty P, Nesto RW (1994) Effect of autonomic nervous system dysfunction on the circadian pattern of myocardial ischemia in diabetes mellitus. J Am Coll Cardiol 24(4):956–962
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lauruschkat, A.H., Albert, A., Arnrich, B. et al. Erfahrungen mit Diabetikern in der Koronarchirurgie—. Clin Res Cardiol 95 (Suppl 1), i7–i13 (2006). https://doi.org/10.1007/s00392-006-1110-3
Issue Date:
DOI: https://doi.org/10.1007/s00392-006-1110-3