Summary
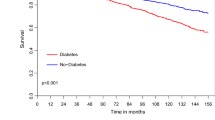
Patients with diabetes nowadays are not directly endangered by dysglycemia, but they suffer vascular complications. The diabetic patient with existing cardiovascular (CV) disease has a particularly high risk for further CV complications and, therefore, requires specific attention. These patients need an intense and multimodal therapeutic approach which includes a strong interdisciplinary cooperation between the cardiologist and the diabetologist. Cardiac rehabilitation can effectively improve prognosis of CV patients with numbers needed to treat (NNT) comparable to standard pharmacological treatment. In diabetics, after coronary surgery, metabolism frequently and markedly deteriorates, and this requires strict metabolic monitoring and close cooperation between the diabetes team and the other professionals (cardiologist, nurses, physiotherapists, psychologists . . .) to reduce complications arising from hyperglycemia and also hypoglycemia and to improve the CV risk factors by lifestyle changes. Frequently, diabetes is only diagnosed during the hospital stay for CV complication; therefore, in these patients, specific attention is required for teaching and inauguration of therapy.
Due to the high risk of these patients and the need of qualified metabolic co-treatment, following CV surgery, diabetic patients should be treated preferentially in rehabilitation centres specialised in both cardiac and metabolic care. Recent studies indicate that a multimodal and aggressive approach in CV diabetic patients can markedly improve their prognosis.
Zusammenfassung
Der herzkranke Diabetiker nach koronarchirurgischen Eingriffen stellt aufgrund seiner hohen vaskulären Gefährdung und der vielfältigen Probleme im Bereich des Stoffwechsels eine besondere Herausforderung für die kardio-metabolische Rehabilitation dar. Eine optimierte Versorgung dieser Patienten erfordert eine engmaschige Kooperation zwischen Patient, Arzt und Diabetesberater bzw. Diabetesassistent, letztendlich unter der Supervision durch einen erfahrenen Diabetologen. Rehabilitationskliniken weisen ein multiprofessionelles Team an Schwestern, Psychologen, Sport- und Bewegungstherapeuten, Sozialarbeitern sowie Ernährungsberatern auf, die im Umgang mit chronisch Kranken besondere Erfahrung besitzen und damit die beste Voraussetzungen für eine umfassende Betreuung dieser kardiovaskulären Patienten haben.
Aufgrund der Komplexität der postoperativen Stoffwechselführung und -neueinstellung sowie der hohen kardiovaskulären Gefährdung der diabetischen Patienten sollten diese besonders nach herzchirurgischen Eingriffen bevorzugt in Rehabilitationskliniken verlegt werden, in denen die Strukturqualität und Stoffwechselexpertise für eine engmaschige qualifizierte Versorgung der Patienten gegeben ist.
Similar content being viewed by others
References
Becker A, Bos G, de Vegt F, Kostense PJ, Dekker JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD (2003) Cardiovascular events in type 2 diabetes: comparison with nondiabetic individuals without and with prior cardiovascular disease. 10-year follow-up of the Hoorn Study. Eur Heart J 24(15):1406–1413
Church TS, Cheng YJ, Earnest CP, Barlow CE, Gibbons LW, Priest EL, Blair SN (2004) Exercise capacity and body composition as predictors of mortality among men with diabetes. Diabetes Care 27(1):83–88
Dalal H, Evans PH, Campbell JL (2004) Recent developments in secondary prevention and cardiac rehabilitation after acute myocardial infarction BMJ 328:693–697
DECODE Study Group. Glucose tolerance and cardiovascular mortality: comparison of the fasting and the 2-hour diagnostic criteria. Arch Intern Med 161:397–404
de Lorgeril M, Salen P, Martin JL et al (1999) Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 99:779–785
Dendale P, Berger J, Hansen D, Vaes J, Benit E, Weymans M (2005) Cardiac rehabilitation reduces the rate of major adverse cardiac events after percutaneous coronary intervention. Eur J Cardiovasc Nurs 4(2):113–116
Gæde P, Vedel N, Larsen GVH, Jensen HH, Parving OP (2003) Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. New Engl Journal Med Volume 348:383–393
Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339:229–234
Hambrecht R, Walther C, Mobius-Winkler S, Gielen S, Linke A, Conradi K, Erbs S, Kluge R, Kendziorra K, Sabri O, Sick P, Schuler G (2004) Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: a randomized trial. Circulation. 109:1371–1378
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L (2001) Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24(4):683–689
Jacob S, Keulen L, Jacob F, Balletshofer B, Häring HU, Lang R (2004) Typ 2 Diabetes, Störungen des Glukose-Stoffwechsels und vaskuläre Erkrankungen. Journal für Kardiologie 11:392–395
Jacob S, Scherer SJ, Klimm HD, Renn W, Keulen L, Scharnagl H, Schlageter S, Keller H, Weismann G, Austin HJ, März W, Häring HU (2004) Insulin resistance and disorders of glucose metabolism in survivors of myocardial infarction. Perfusion 17:228–234
Jacob S, Motz W, Steinhagen-Thiessen E, Tschöpe D (2003) Minimal metabolic data set for patients at high vascular risk. Exp Clin Endocrinol Diabetes 111:471–474
Jacob S (2005) Antihyperglykämika. In: Meinertz T, Rösen P, Schömig A, Tschöpe D, Ziegler D (Hrsg) Diabetes und Herz, 1. Aufl. Steinkopff, Darmstadt, S 354–362
Kuusisto J, Lempiäinen P, Mykkänen L, Laakso M (2001) Insulin resistance syndrome predicts coronary heart disease events in elderly type 2 diabetic men. Diabetes Care 24:1629–1633
Kowalska I, Prokop J, Bachorzewska-Gajewska H, Telejko B, Kinalskal I, Kochmn W, Musial W (2001) Disturbances of glucose metabolism in men referred for coronary arteriography. Postload glycemia as predictor for coronary artherosclerosis. Diabeste Care 24:897–901
Lazar HL, Chipkin SR, Fitzgerald CA, Bao Y, Cabral H, Apstein CS (2004) Tight glycemic control in diabetic coronary artery bypass graft patients improves perioperative outcomes and decreases recurrent ischemic events. Circulation 109:1497–1502
Malmberg K, Rydén L, Wedel H, Birkeland K, Bootsma A, Dickstein K, Efendic S, Fisher M, Hamsten A, Herlitz J, Hildebrandt P, MacLeod K, Laakso M, Torp-Pedersen C, Waldenström A for the DIGAMI 2 Investigators (2005) Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2): effects on mortality and morbidity. European Heart Journal 26:650–661
Meigs JB, Nathan DM, D’Agostino RB, Wilson PWF (2002) Fasting and postchallenge glycemia and cardiovascular disease risk. The Framingham Offspring Study Diabetes Care 25:1845–1850
Murchie P, Campbell NC, Ritchie LD, Simpson JA, Thain J (2003) Secondary prevention clinics for coronary heart disease: four year follow up of a randomised controlled trial in primary care. BMJ (326)84:1–6
Norhammer A, Tenerz A, Nilsson G, Hamsten A, Efendic S, Ryden L, Malmberg K (2002) Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet 359:2140–2144
Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ (1998) Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280:2001–2007
Qiao Q, Tuomilehto J, Borch-Johnsen K (2003) Post-challenge hyperglycaemia is associated with premature death and macrovascular complications. Diabetologia 46(Suppl 1):M17–21
Schnell O, Schafer O, Kleybrink S, Doering W, Standl E, Otter W (2004) Munich registry: intensification of therapeutic approaches reduces mortality in diabetic patients with acute myocardial infarction: the Munich registry. Diabetes Care 27:455–460
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258):405–412
Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefebvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Koranyi L, Laakso M, Mokan M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J (2005) PROactive investigators. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial in macroVascular Events): a randomised controlled trial. Lancet 366(9493):1279–1289
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacob, S. Die Bedeutung der Rehabilitation beim herzkranken Diabetiker nach chirurgischen Eingriffen. Clin Res Cardiol 95 (Suppl 1), i103–i109 (2006). https://doi.org/10.1007/s00392-006-1108-x
Issue Date:
DOI: https://doi.org/10.1007/s00392-006-1108-x