Abstract
Objectives
The aim of this study was to evaluate possible age-related changes in mesenteric artery and portal venous blood flow dynamics in relation to systemic haemodynamics in order to delineate putative haemodynamic changes relevant for postprandial hypotension in the elderly. Studies were performed over a wide age-range and for the first time in over 85-year-old patients.
Design
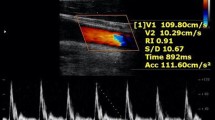
Superior mesenteric artery (SMA) parameters (diameter, peak systolic velocity, enddiastolic velocity, pulsatility index, volume flow) and portal vein (PV) parameters (diameter, portal vein velocity, volume flow) were measured by duplex ultrasound (General Electrics, Vivid 3) in 98 fasting subjects aged from 21 to 96 years. Systemic vascular parameters such as blood pressure, heart rate and cardiac output (echocardiography) were also determined. Excluded were patients with severe heart failure, liver cirrhosis, sepsis and those with mesenteric artery stenosis.
Results
Pulsatility index (PI) was positively correlated with age (r=0.33, p=0.015). In patients over 85 years, PI was significantly increased (p=0.002) as compared to younger controls. Cardiac output was negatively correlated with age (r=–0.247, p=0.005). The other haemodynamic parameters did not show age-dependent alterations.
Conclusion
The increase of PI in the SMA in patients over 85 years represents an increase of vascular resistance in the splanchnic area, because PI is sensitive to resistance changes of small arterial vessels. The pulsatility index in the splanchnic area seems to rise steeply in oldest old patients, probably as an attempt to compensate diminutions in cardiac output seen in this age group. These findings indicate that the splanchnic vascular bed is already used in the fasting state to guarantee systemic haemodynamics. Vasodilatation of this vascular bed as physiologically seen postprandially may therefore easily induce postprandial hypotension in the oldest old.
Zusammenfassung
Einführung
Ziel der vorliegenden Arbeit war die Untersuchung von möglichen Alters-assoziierten Blutflussveränderungen im splanchnischen vaskulären Bett – A. mesenterica superior (SMA) und Portalvene (PV) –, die Ursache für die postprandiale Hypotonie sein könnten. Untersucht wurden hierzu ältere und zum ersten Mal Patienten über 85 Jahre.
Methodik
SMA-Parameter (Durchmesser, peak systolic velocity, enddiastolic velocity, Pulsatilitätsindex, Volumenfluss) und PV-Parameter (Durchmesser, portal vein velocity, Volumenfluss) wurden mittels Doppler-Ultraschall (General Electrics, Vivid 3) in 98 Menschen im Alter von 21–96 Jahren im Nüchternzustand untersucht. Als systemische hämodynamische Parameter wurden der Blutdruck, die Herzfrequenz und das Herzzeitvolumen (CO) (Echokardiographie) gemessen. Ausgeschlossen wurden Patienten mit schwerer Herzinsuffizienz, Leberzirrhose, Sepsis sowie Stenose der A. mesenterica superior.
Resultate
Der Pulsatilitätsindex (PI) zeigte sich positiv mit dem Alter korreliert (r=0,33; p=0,015). In über 85-jährigen Patienten war der PI signifikant höher als bei Jüngeren (p=0,002). Dagegen war der CO negativ mit dem Alter korreliert (r=–0,247; p=0,005). Die anderen gemessenen hämodynamischen Parameter zeigten keine signifikante Altersassoziation.
Zusammenfassung und Schlussfolgerung
Der signifikante Anstieg des PI bei über 85-jährigen Patienten weist auf eine erhöhte vaskuläre splanchnische Resistenz hin, da der PI sensitiv den vaskulären Tonus auf arteriolärer Ebene misst. Der PI steigt bei Hochbetagten steil an, vermutlich als Zeichen hierfür, dass damit versucht wird, den verminderten CO zu kompensieren. Somit scheint das große Blutreservoir im Splanchnikusgebiet schon im Nüchternzustand zur Garantierung der systemischen Hämodynamik mobilisiert zu werden. Vasodilatation auf dieser Ebene – wie physiologischerweise postprandial beobachtet – prädisponiert diese Menschen somit zu einer postprandialen Hypotonie.
Similar content being viewed by others
Abbreviations
- SMA:
-
superior mesenteric artery
- SMA_PI:
-
SMA pulsatility index
- SMA_RI:
-
SMA resistance index
- SMA_PSV:
-
SMA peak systolic velocity in cm/s
- SMA_EDV:
-
SMA enddiastolic velocity in cm/s
- SMA_VF:
-
SMA volume flow in l/min
- SMA_VFCO:
-
SMA volume flow in % of CO
- SMA_dia:
-
SMA diameter in mm
- PV_V:
-
mean portal velocity in cm/s
- PV_F:
-
portal venous blood flow in ml/min
- PV_F-CO:
-
portal venous blood flow in % of Co
- Dia 1 and Dia 2:
-
the diameters of the cross sectional area of the vessel in mm
- RR syst:
-
systolic blood pressure in mmHg
- RR diast:
-
diastolic blood pressure in mmHg
- PP:
-
pulse pressure in mmHg
- MAP:
-
mean arterial pressure in mmHg
- Temp:
-
body temperature in °C
References
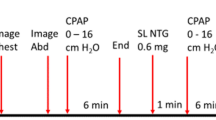
Sieber C, Beglinger C, Jäger K, Hildebrand P, Stalder GA (1991) Regulation of postprandial mesenteric blood flow in humans: evidence for a cholinergic reflex. Gut 32:361–366
Mottet C, Sieber CC, Nauer A, Drewe J, Fried R, Larsen F, Beglinger C (1998) Hemodynamic effects of the somatostatin analog lanreotide in humans: placebo-controlled, cross-over dose-ranging Echo-Doppler study. Hepatology 27:920–925
Lubart E, Segal R, Baumoehl Y, Matron M, Leibovitz A (2006) Postprandial hypotension in long-term care elderly patients on enteral feeding. J Am Geriatr Soc 54:1377–1781
Staneczek O, Abbas-Terki N, Loew F, Sieber CC (2001) A full stomach but an empty head. J Am Geriatr Soc 49:1262–1263
Vloet LC, Pel-Little RE, Jansen PA, Jansen RW (2005) High prevalence of postprandial and orthostatic hypotension among geriatric patients admitted to Dutch hospitals. J Gerontol A Biol Sci Med Sci 60:1271–1277
Fisher AA, Davis MW, Srikusalanukul W, Budge MM (2005) Postprandial hypotension predicts all-cause mortality in older, low-level care residents. J Am Geriatr Soc 53:1313–1320
Gentilcore D, Jones KL, O'Donovan DG, Horowitz M (2006) Postprandial hypotension – novel insights into pathophysiology and therapeutic implications. Curr Vasc Pharmacol 4:161–171
Sabba C, Merkel C, Zoli M et al (1995) Intraobserver and interequipment variability of echo-duplex examination of the portal vein: Effect of a cooperative training program. Hepatology 21:428–433
Szinnai C, Mottet C, Gutzwiller JP, Drewe J, Beglinger C, Sieber CC (2001) Role of gender upon basal and postprandial systemic and splanchnic haemodynamics in humans. Scand J Gastroenterol 36:540–544
Lim HK, Lee WJ, Kim SH, Lee SJ et al (1999) Splanchnic arterial stenosis or occlusion: diagnosis at Doppler US. Radiology 211:405–410
Zwolak RM, Fillinger MF, Walsh DB et al (1998) Mesenteric and celiac duplex scanning: a validation study. J Vasc Surg 27:1078–1087
Moneta GL (2001) Screening for mesenteric vascular insufficiency and follow-up of mesenteric artery bypass procedures. Semin Vasc Surg 14:186–192
Perko MJ, Perko G, Just S et al (1996) Changes in superior mesenteric artery Doppler waveform during reduction of cardiac stroke volume and hypotension. Ultrasound Med Biol 22:11–18
Rizzo RJ, Sandager G, Astleford P et al (1990) Mesenteric flow velocity variations as a function of angle of insonation. J Vasc Surg 11:688–694
Mottet C, Sieber CC, Nauer A et al (1998) Hemodynamic effects of the somatostatin analog lancreotide in humans: placebo controlled, crossover dose ranging Echo-Doppler Study. Hepatology 27:920–925
Perko MJ (2001) Duplex ultrasound for assessment of superior mesenteric artery blood flow. Eur J Vasc Surg 21:106–117
Moriyasu F, Ban N, Nishida D et al (1984) Quantitative measurement of portal blood flow in patients with chronic liver disease using an ultrasound Duplex system consisting of a pulsed Doppler flowmeter and Bmode electroscanner. Gastroenterology Jpn 19:529–538
Maurer MS, Karmally W, Rivadeneira H, Parides MK, Bloomfield DM (2000) Upright posture and postprandial hypotension in elderly persons. Ann Intern Med 133:533–536
Ray-Chaudhuri K, Ryder SA, Thomaides et al (1994) The relationship between blood flow and pulsatility index in the superior mesenteric artery at rest and during constrictor stimuli in normal subjects. J Clin Ultrasound 22:149–160
Sieber C, Beglinger C, Jäger K, Stalder GA (1992) Intestinal phase of superior mesenteric artery blood flow in man. Gut 33:497–501
Mehagnoul-Schipper DJ, Boerman RH, Hoefnagels WH, Jansen RW (2001) Effect of levodopa on orthostatic and postprandial hypotension in elderly Parkinsonian patients. J Gerontol A Biol Sci Med 56:M749–M755
Idiaquez J, Rios L, Sandoval E (1997) Postprandial hypotension in Alzheimer's disease. Clin Auton Res 7:119–120
Kawaguchi R, Nomura M, Miyajima H, Nakaya Y, Mouri S, Ito S (2002) Postprandial hypotension in elderly subjects: spectral analysis of heart rate variability and electrocardiograms. J Gastroenterol 37:87–93
Polio J, Sieber CC, Lerner E et al (1993) Cardiovascular hyporesponsiveness to norepinephrine, propanolol and nitroglycerin in portal hypertensive and aged rats. Hepatology 18:128–136
Zoli M, Magalotti D, Bianchi G et al (1999) Total and functional blood flow decreases in parallel with aging. Age and Ageing 28:29–33
Puisieux F, Court D, Baheu E et al (2002) Intraindividual reproducibility of postprandial hypotension. Gerontology 48:315–320
O'Donovan D, Feinle-Bisset C, Chong C, Cameron A, Tonkin A, Wishart J, Horowitz M, Jones KL (2005) Intraduodenal guar attenuates the fall in blood pressure induced by glucose in healthy older adults. J Gerontol A Biol Sci Med Sci 60:940–946
Jones KL, MacIntosh C, Su YC, Wells F, Chapman IM, Tomkin A, Horowitz M (2001) Guar gum reduces postprandial hypotension in older people. J Am Geriatr Soc 49:162–167
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wicklein, S., Mühlberg, W., Richter, B. et al. Increased splanchnic arterial vascular resistance in oldest old patients. Z Gerontol Geriatr 40, 37–42 (2007). https://doi.org/10.1007/s00391-007-0431-9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00391-007-0431-9