Abstract
The relevance of liver dysfunction in the management of critically ill patients is increasingly being recognized. It has been found to affect mortality of patients with septic organ failure in several studies. The increasing prevalence of chronic liver disease among intensive care patients adds importance to the issue of monitoring the various aspects of liver function. An array of liver function tests as part of blood biochemistry testing has long been established. In the context of critical care and chronic liver disease, however, they must be interpreted cautiously. In addition, several dynamic tests of liver function have been developed. Relatively best explored are tests based on the hepatic elimination of indocyanine-green (ICG). Commercially available systems analyzing the plasma disappearance rate of ICG (ICG-PDR) are being marketed but these parameters also are difficult to interpret in the intensive care setting and especially in patients with chronic liver disease. ICG-PDR correlates with mortality in patients with septic organ dysfunction but studies investigating the outcome-oriented results of therapeutic interventions directed by these parameters have not been published. The possible relevance to intensive care management of several other dynamic tests of liver function, as well as interventional and ultrasonografic methods to address liver perfusion, are discussed in the article. As yet, there is no single method to monitor the various aspects of liver function and no method whose clinical value has been proved. Clinicians therefore have to mostly rely on clinical judgement aided by a reasonable selection among existing monitoring tools.
Zusammenfassung
Die Bedeutung von akuten Funktionsstörungen der Leber bei schwerstkranken Patienten findet zunehmende Beachtung. Ihr Einfluss auf die Mortalität wurde in mehreren Studien für Patienten mit septischem Organversagen nachgewiesen. Gleichzeitig stellt die zunehmende Prävalenz chronischer Leberschäden bei Intensivpatienten eine Herausforderung für die Überwachung der Leberfunktion dar. Neben den etablierten Parametern des Routinelabors, deren Bedeutung allerdings gerade bei zirrhotischen Patienten umsichtig zu interpretieren ist, sind es vor allem dynamische Funktionstests, denen das Interesse der Intensivmedizin gilt. Am besten etabliert sind Monitoringverfahren, die auf der hepatischen Elimination von Indozyaningrün (ICG) beruhen. Hierauf basieren auch kommerziell angebotene Systeme zur Beurteilung der ICG-Plasmaverschwinderate (ICGPDR). Die Bedeutung der hiermit ermittelten Daten ist jedoch äußerst zurückhaltend zu beurteilen. Während die ICG-PDR beim septischen Multiorganversgen eine Korrelation mit der Mortalität aufzuweisen scheint, liegen ergebnisbezogene Studien hierauf basierter therapeutischer Interventionen bislang nicht vor. Die mögliche Bedeutung weiterer dynamischer Leberfuntionstests und spezieller interventioneller und sonografischer Untersuchungen zur Beurteilung der Leberperfusion für das intensivmedizinische Management wird diskutiert. Da derzeit keine die vielfältigen Leistungen der Leber umfassende und in ihrer klinischen Relevanz gesicherte Methode des Leberfunktionsmonitorings existiert, wird der Kliniker vorerst auf eine umsichtige Anwendung unterschiedlicher Instrumente und deren Interpretation im klinischen Kontext angewiesen bleiben.
Similar content being viewed by others
Literatur
Oellerich M, Armstrong VW (2001) The MEGX test: a tool for the realtime assessment of hepatic function. Ther Drug Monit 23:81–92
Sakka SG (2007) Assessing liver function. Curr Opin Crit Care 13:207–214
Shaver WA, Bhatt H, Combes B (1986) Low serum alkaline phosphatase activity in Wilson’s disease. Hepatology 6:859–863
Hawker F (1991) Liver dysfunction in critical illness. Anaesth Intensive Care 19:165–181
Berk PD, Wolkoff AW, Berlin NI (1975) Inborn errors of bilirubin metabolism. Med Clin North Am 59:803–816
Ching N, Grossi CE, Angers J, Zurawinsky HS, Jham G, Mills CB, Nealon TF Jr (1980) The outcome of surgical treatment as related to the response of the serum albumin level to nutritional support. Surg Gynecol Obstet 151:199–202
Bradley JA, Cunningham KJ, Jackson VJ, Hamilton DN, Ledingham IM (1981) Serum protein levels in critically ill surgical patients. Intensive Care Med 7:291–295
Apelgren KN, Rombeau JL, Twomey PL, Miller RA (1982) Comparison of nutritional indices and outcomes in critically ill patients. Crit Care Med 10:305–307
Golub R, Sorrento JJ Jr, Cantu R Jr, Nierman DM, Moideen A, Stein HD (1994) Efficacy of albumin supplementation in the surgical intensive care unit: a prospective, randomized study. Crit Care Med 22:613–619
Fleck A, Raines G, Hawker F, Trotter J, Wallace PI, Ledingham IM, Calman KC (1985) Increased vascular permeability: a major cause of hypoalbuminaemia in disease and injury. Lancet 325:781–784
Tripodi A, Salerno F, Chantarangkul V, Clerici M, Cazzaniga M, Primignani M, Mannucci PM (2005) Evidence of normal thrombin generation in cirrhosis despite abnormal conventional coagulation tests. Hepatology 41:553–558
Montalto P, Vlachogiannakos J, Cox DJ, Pastacaldi S, Patch D, Burroughs AK (2002) Bacterial infection in cirrhosis impairs coagulation by a heparin effect: a prospective study. J Hepatol 37:463–470
Noris M, Remuzzi G (1999) Uremic bleeding: closing the circle after 30 years of controversies? Blood 94:2569–2574
Laffi G, Marra F, Tarquini R, Abbate R (2006) Coagulation defects in cirrhosis- old dogmas not yet ready for burial. J Thromb Haemost 4:2068–2069
Clemmesen JO, Larsen FS, Kondrup J, Hansen BA, Ott P (1999) Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 29:648–653
Ong JP, Aggarwal A, Krieger D, Easley KA, Karafa MT, Van Lente F, Arroliga AC, Mullen KD (2003) Correlation between ammonia levels and the severity of hepatic encephalopathy. Am J Med 114:188–193
Ott P (1998) Hepatic elimination of indocyanine green with special reference to distribution kinetics and the influence of plasma protein binding. Pharmacol Toxicol 83:1–48
Bradley SE, Ingelfinger FJ, Bradley GP, Curry JJ (1945) The estimation of hepatic blood flow in man. J Clin Invest 24:890–897
Leevy CM, Mendenhall CL, Lesko W, Howard MM (1962) Estimation of hepatic blood flow with indocyanine green. J Clin Invest 41:1169–1179
Ott P, Bass L, Keiding S (1997) Hepatic ICG removal in the pig depends on plasma protein and hematocrit: evidence of sinusoidal binding disequilibrium and unstirred water layer effects. Hepatology 26:679–690
Lund M, Kang L, Tygstrup N, Wolkoff AW, Ott P (1999) Effects of LPS on transport of indocyanine green and alanine uptake in perfused rat liver. Am J Physiol 277:G91–100
Chijiiwa K, Mizuta A, Ueda J, Takamatsu Y, Nakamura K, Watanabe M, Kuroki S, Tanaka M (2002) Relation of biliary bile acid output to hepatic adenosine triphosphate level and biliary indocyanine green excretion in humans. World J Surg 26:457–461
Beno DW, Uhing MR, Goto M, Chen Y, Jiyamapa-Serna VA, Kimura RE (2001) Endotoxin-induced reduction in biliary indocyanine green excretion rate in a chronically catheterized rat model. Am J Physiol Gastrointest Liver Physiol 280:G858–G865
Uusaro A, Ruokonen E, Takala J (1994) Estimation of splanchnic blood flow by the Fick principle in man and problems in the use of indocyanine green. Cardiovasc Res 30:106–112
Sakka SG, Koeck H, Meier-Hellmann A (2004) Measurement of indocyanine green plasma disappearance rate by two different dosages. Intensive Care Med 30:506–509
Sakka SG, van Hout N (2006) Relation between indocyanine green (ICG) plasma disappearance rate and ICG blood clearance in critically ill patients. Intensive Care Med 32:766–769
Sakka SG, Reinhart K, Meier-Hellmann A (2000) Comparison of invasive and noninvasive measurements of indocyanine green plasma disappearance rate in critically ill patients with mechanical ventilation and stable hemodynamics. Intensive Care Med 26:1553–1556
Faybik P, Krenn CG, Baker A, Lahner D, Berlakovich G, Steltzer H, Hetz H (2004) Comparison of invasive and noninvasive measurement of plasma disappearance rate of indocyanine green in patients undergoing liver transplantation: a prospective investigator- blinded study. Liver Transpl 10:1060–1064
Pollack DS, Sufian S, Matsumoto T (1979) Indocyanine green clearance in critically ill patients. Surg Gynecol Obstet 149:852–854
Kholoussy AM, Pollack D, Matsumoto T (1984) Prognostic significance of indocyanine green clearance in critically ill surgical patients. Crit Care Med 12:115–116
Maynard ND, Bihari DJ, Dalton RN, Beale R, Smithies MN, Mason RC (1997) Liver function and splanchnic ischemia in critically ill patients. Chest 111:180–187
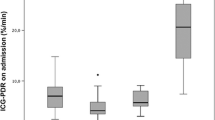
Sakka SG, Reinhart K, Meier-Hellmann A (2002) Prognostic value of the indocyanine green plasma disappearance rate in critically ill patients. Chest 122:1715–1720
Kimura S, Yoshioka T, Shibuya M, Sakano T, Tanaka R, Matsuyama S (2001) Indocyanine green elimination rate detects hepatocellular dysfunction early in septic shock and correlates with survival. Crit Care Med 29:1159–1163
Malbrain MLNG, Molnar Z (2006) Prognostic value of indocyanine green clearance in severe sepsis. Intensive Care Med 32:S8
Rank N, Michel C, Haertel C, Lenhart A, Welte M, Meier-Hellmann A, Spies C (2000) N-acetylcysteine increases liver blood flow and improves liver function in septic shock patients: results of a prospective, randomized, double-blind study. Crit Care Med 28:3799–3807
Devlin J, Ellis AE, McPeake J, Heaton N, Wendon JA, Williams R (1997) N-acetylcysteine improves indocyanine green extraction and oxygen transport during hepatic dysfunction. Crit Care Med 25:236–242
Smithies M, Yee TH, Jackson L, Beale R, Bihari D (1994) Protecting the gut and the liver in the critically ill: effects of dopexamine. Crit Care Med 22:789–795
Maynard ND, Bihari DJ, Dalton RN, Smithies MN, Mason RC (1995) Increasing splanchnic blood flow in the critically III. Chest 108:1648–1654
Birnbaum J, Lehmann C, Taymoorian K, Krausch D, Wauer H, Gründling M, Spies C, Kox WJ (2003) Einfluss von Dopexamin und Iloprost auf die Plasma-Disappearance-Rate von Indozyaningrün bei Patienten im septischen Schock. Anaesthesist 52:1014–1019
Meier-Hellmann A, Bredle DL, Specht M, Hannemann L, Reinhart K (1999) Dopexamine increases splanchnic blood flow but decreases gastric mucosal pH in severe septic patients treated with dobutamine. Crit Care Med
Lehmann C, Taymoorian K, Wauer H, Krausch D, Birnbaum J, Kox WJ (2000) Effects of the stable prostacyclin analogue iloprost on the plasma disappearance rate of indocyanine green in human septic shock. Intensive Care Med 26:1557–1560
Scheingraber S, Richter S, Igna D, Girndt M, Flesch S, Kleinschmidt S, Schilling MK (2007) Indocyanine green elimination but not bilirubin indicates improvement of graft function during MARS therapy. Clin Transplant 21:689–695
Tsubono T, Todo S, Jabbour N, Mizoe A, Warty V, Demetris AJ, Starzl TE (1996) Indocyanine green elimination test in orthotopic liver recipients. Hepatology 24:1165–1171
Plevris JN, Jalan R, Bzeizi KI, Dollinger MM, Lee A, Garden OJ, Hayes PC (1999) Indocyanine green clearance reflects reperfusion injury following liver transplantation and is an early predictor of graft function. J Hepatol 30:142–148
Daz S, Pérez-Peña J, Sanz J, Olmedilla L, Garutti I, Barrio JM (2003) Haemodynamic monitoring and liver function evaluation by pulsion cold system Z-201 (PCS) during orthotopic liver transplantation. Clin Transplant 17:47–55
Oellerich M, Raude E, Burdelski M, Schulz M, Schmidt FW, Ringe B, Lamesch P, Pichlmayr R, Raith H, Scheruhn M et al (1987) Monoethylglycinexylidide formation kinetics: a novel approach to assessment of liver function. J Clin Chem Clin Biochem 25:845–853
Orlando R, Piccoli P, De Martin S, Padrini R, Floreani M, Palatini P (2004) Cytochrome P450 1A2 is a major determinant of lidocaine metabolism in vivo: effects of liver function. Clin Pharmacol Ther 75:80–88
Schröter J, Wandel C, Böhrer H, Schmidt H, Böttiger BW, Martin E (1995) Lignocaine metabolite formation: an indicator for liver dysfunction and predictor of survival in surgical intensive care patients. Anaesthesia 50:850–854
Liu YT, Hao HP, Liu CX, Wang GJ, Xie HG (2007) Drugs as CYP3A probes, inducers, and inhibitors. Drug Metab Rev 39:699–721
Tortorici MA, Kochanek PM, Poloyac SM (2007) Effects of hypothermia on drug disposition, metabolism, and response: a focus of hypothermiamediated alterations on the cytochrome P450 enzyme system. Crit Care Med 35:2196–2204
McKindley DS, Boulet J, Sachdeva K, Wang P, Chichester C (2002) Endotoxic shock alters the pharmacokinetics of lidocaine and monoethylglycinexylidide. Shock 17:199–204
Jakob SM, Ruokonen E, Rosenberg PH, Takala J (2002) Effect of dopamine- induced changes in splanchnic blood flow on MEGX production from lidocaine in septic and cardiac surgery patients. Shock 18:1–7
Hepner GW, Vesell ES (1975) Quantitative assessment of hepatic function by breath analysis after oral administration of (14C)aminopyrine. Ann Intern Med 83:632–638
Novotny AR, Emmanuel K, Maier S, Westerholt A, Weighardt H, Stadler J, Bartels H, Schwaiger M, Siewert JR, Holzmann B, Heidecke CD (2007) Cytochrome P450 activity mirrors nitric oxide levels in postoperative sepsis: predictive indicators of lethal outcome. Surgery 141:376–384
Tygstrup N (1964) The galactose elimination capacity in control subjects and in patients with cirrhosis of the liver. Acta Med Scand 175:281–289
Tengström B (1969) The discriminatory ability of a galactose tolerance test and some other tests in the diagnosis of cirrhosis of the liver, hepatitis and biliary obstruction. Scand J Clin Lab Invest 23:159–168
Ranek L, Andreasen PB, Tygstrup N (1976) Galactose elimination capacity as a prognostic index in patients with fulminant liver failure. Gut 17:959–964
Schmidt LE, Ott P, Tygstrup N (2004) Galactose elimination capacity as a prognostic marker in patients with severe acetaminophen-induced hepatotoxicity: 10 years’ experience. Clin Gastroenterol Hepatol 2:418–424
Henrion J, Descamps O, Luwaert R, Schapira M, Parfonry A, Heller F (1994) Hypoxic hepatitis in patients with cardiac failure: incidence in a coronary care unit and measurement of hepatic blood flow. J Hepatol 21:696–703
Butler MA, Iwasaki M, Guengerich FP, Kadlubar FF (1989) Human cytochrome P-450PA (P-450IA2), the phenacetin O-deethylase, is primarily responsible for the hepatic 3-demethylation of caffeine and N-oxidation of carcinogenic arylamines. Proc Natl Aca Sci USA 86:7696–7700
Renner E, Wietholtz H, Huguenin P, Arnaud MJ, Preisig R (1984) Caffeine: a model compound for measuring liver function. Hepatology 4:38–46
Schaad HJ, Renner EL, Wietholtz H, Arnaud MJ, Preisig R (1995) Caffeine demethylation measured by breath analysis in experimental liver injury in the rat. J Hepatol 22:82–87
Tanaka E, Ishikawa A, Yamamoto Y, Osada A, Tsuji K, Fukao K, Misawa S, Iwasaki Y (1992) A simple useful method for the determination of hepatic function in patients with liver cirrhosis using caffeine and its three major dimethylmetabolites. Int J Clin Pharmacol Ther Toxicol 30:336–341
Wirts CW, Bradford BK (1948) The biliary excretion od bromsulfalein as a test of liver function in a group of patients following hepatitis or serum jaundice. J Clin Invest 27:600–608
Yamanaka N, Shimizu S, Chijiiwa K, Nishiyama K, Noshiro H, Yamaguchi K, Tanaka M (2001) Hepatectomy and marked retention of indocyanine green and bromosulfophtalein. Hepatogastroenterology 48:1450–1452
Conti F, Dousset B, Cherruau B, Guérin C, Soubrane O, Houssin D, Calmus Y (2004) Use of lidocaine metabolism to test liver function during the long-term follow-up of liver transplant recipients. Clin Transplant 18:235–241
Moitinho E, Escorsell A, Bandi JC, Salmerón JM, Garca-Pagán JC, Rodés J, Bosch J (1999) Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology, pp 626–631
Monescillo A, Martínez-Lagares F, Ruiz-del-Arbol L, Sierra A, Guevara C, Jiménez E, Marrero JM, Buceta E, Sánchez J, Castellot A, Peñate M, Cruz A, Peña E (2004) Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology 40:793–801
Alpern MB, Rubin JM, Williams DM, Capek P (1987) Porta hepatis: duplex Doppler US with angiographic correlation. Radiology 162:53–56
Hellinger A, Roll C, Stracke A, Erhard J, Eigler FW (1996) Impact of colour Doppler sonography on detection of thrombosis of the hepatic artery and the portal vein after liver transplantation. Langenbecks Arch Chir
Martínez-Noguera A, Montserrat E, Torrubia S, Villalba J (2002) Doppler in hepatic cirrhosis and chronic hepatitis. Semin Ultrasound CT MR 23:19–36
Paulson EK, Kliewer MA, Frederick MG, Keogan MT, DeLong DM, Nelson RC (1997) Doppler US measurement of portal venous flow: variability in healthy fasting volunteers. Radiology 202:721–724
Author information
Authors and Affiliations
Corresponding author
Additional information
Wenn’s da kein Problem haben, dann ham’s was übersehen. Ursula Schweigart
Serie:Neue Technologien in der IntensivmedizinHerausgegeben von J. Langgartner (Regensburg) und R.M. Schmid (München)
Rights and permissions
About this article
Cite this article
Umgelter, A., Geisler, F. & Schulte-Frohlinde, E. Die Überwachung der Leberfunktionen in der Intensivmedizin. Intensivmed 45, 413–423 (2008). https://doi.org/10.1007/s00390-008-0895-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00390-008-0895-x