Abstract
Purpose
Short-stay admissions, with lengths of stay less than 24 h, are used for various surgeries without increasing adverse events. However, it is unclear if short-stay admissions would be safe for loop ileostomy reversals. This review aimed to compare outcomes between short (≤24 hours) and long (>24 hours) admissions for adults undergoing loop ileostomy reversals.
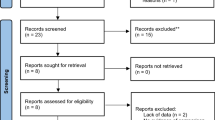
Methods
Medline, Embase, CINAHL, Web of Science, and the Cochrane Library were systematically searched for studies comparing short- to long-stay admissions in adults undergoing loop ileostomy reversals. Meta-analyses were conducted for mortality, reoperation, readmission, and non-reoperative complications. Quality of evidence was assessed with grading of recommendations, assessment, development, and evaluations (GRADE) guidelines.
Results
Four observational studies enrolling 24,628 patients were included. Moderate certainty evidence suggests there is no difference in readmissions between short- and long-stay admissions (relative risk (RR) 0.98, 95% CI 0.75 to 1.28, p 0.86). Low certainty evidence demonstrates that short stays may reduce non-reoperative complications (RR 0.44, 95% CI 0.31 to 0.62, p < 0.01). Very low certainty evidence demonstrates that there is no difference in reoperations between short and long stays (RR 1.14, 95% CI 0.26 to 5.04, p 0.87).
Conclusions
Moderate certainty evidence demonstrates that there is no difference in readmission rates between short- and long-stay admissions for loop ileostomy reversals. Less robust evidence suggests equivalence in reoperations and a decrease in non-reoperative complications. Future prospective trials are required to evaluate the feasibility and efficacy of short-stay admissions.
Trial Registration
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=307381 Prospero (CRD42022307381), January 30, 2022.




Similar content being viewed by others
References
Basse L et al (2000) A clinical pathway to accelerate recovery after colonic resection. Ann Surg 232(1):51
Basse L et al (2004) Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum 47(3):271–278
Ljungqvist O, Young-Fadok T, Demartines N (2017) The history of enhanced recovery after surgery and the ERAS Society. J Laparoendosc Adv Surg Tech 27(9):860-862
Kraft K et al (2011) Indications for ambulatory gastrointestinal and endocrine surgery in adults. J Visc Surg 148(1):69–74
Chow A et al (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 24(6):711
Arezzo A et al (2015) Laparoscopic right colectomy reduces short-term mortality and morbidity. Results of a systematic review and meta-analysis. Int J Colorectal Dis 30(11): p. 1457-1472
Luglio G et al (2011) Loop ileostomy reversal after colon and rectal surgery: a single institutional 5-year experience in 944 patients. Arch Surg 146(10):1191–1196
Levy BF et al (2009) 23-hour-stay laparoscopic colectomy. Dis Colon Rectum 52(7):1239–1243
Wong KS et al (2005) Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum 48(2):243–250
Moran MR (1997) Same-day surgery ileostomy closure. Am J Manag Care 3(7):1003–1006
Bhalla A et al (2015) Day-case closure of ileostomy: feasible, safe and efficient. Colorectal Dis 17(9):820–823
Peacock O et al (2013) Twenty-three-hour stay loop ileostomy closures: a pilot study. Tech Coloproctol 17(1):45–49
Camilleri-Brennan J, Steele R (2002) Prospective analysis of quality of life after reversal of a defunctioning loop ileostomy. Colorectal Dis 4(3):167–171
Bollinger AJ et al (2015) Is scheduled intravenous acetaminophen effective in the pain management protocol of geriatric hip fractures? Geriatr Orthop Surg Rehabil 6(3):202–208
Katayama H et al (2016) Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today 46(6):668–685
Baiocchi GL et al (2020) Incidence and grading of complications after gastrectomy for cancer using the GASTRODATA Registry: a European retrospective observational study. Ann Surg 272(5)
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205
Waterland P et al (2015) Defunctioning ileostomy reversal rates and reasons for delayed reversal: does delay impact on complications of ileostomy reversal? A Study of 170 Defunctioning Ileostomies. J Clinic Med Res 7(9):685–9
Bell C et al (2005) A comparison of complications associated with colostomy reversal versus ileostomy reversal. Am J Surg 190(5):717–720
El-Hussuna A, Lauritsen M, Bülow S (2012) Relatively high incidence of complications after loop ileostomy reversal. Dan Med J 59(10):A4517
Veritas Health Innovation, Covidence systematic review software. 2021: Melbourne, Australia.
Sterne JA et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355
Boutron I et al (2022) Cochrane handbook for systematic reviews of interventions version 6.3. Chapter 7: considering bias and conflicts of interest among the included studies 2022 February 2022 [cited 2022 March 2022]; Available from: https://training.cochrane.org/handbook/current/chapter-07
Deeks J, Higgins J, Altman D (2021) Chapter 9: Summarizing study characteristics and preparing for synthesis. Cochrane Handbook for Systematic Reviews of Intervention 2021 [cited 2021 January]; Available from: https://training.cochrane.org/handbook/current/chapter-09
Cummings P (2009) The relative merits of risk ratios and odds ratios. Arch Pediatr Adolesc Med 163(5):438–445
McMaster University and Evidence Prime, GRADEpro GDT: Gradepro Guideline Development Tool 2021
The Cochrane Collaboration, Review Manager (RevMan). The Cochrane Collaboration
Sajid MS, Bhatti MI, Miles WF (2015) Systematic review and meta-analysis of published randomized controlled trials comparing purse-string vs conventional linear closure of the wound following ileostomy (stoma) closure. Curr Gastroenterol Rep 3(2):156–161
Madani R et al (2019) Hand-sewn versus stapled closure of loop ileostomy: a meta-analysis. Dig Surg 36(3):183–194
Young MT et al (2015) Laparoscopic versus open loop ileostomy reversal: is there an advantage to a minimally invasive approach? World J Surg 39(11):2805–2811
Leung TT et al (2008) Comparison of stapled versus handsewn loop ileostomy closure: a meta-analysis. J Gastrointest Surg 12(5):939–944
Wan X et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135
Weir CJ et al (2018) Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: a systematic review. BMC Med Res Methodol 18(1):25
Afshari K et al (2021) Loop-ileostomy reversal in a 23-h stay setting is safe with high patient satisfaction. Scand J Gastroenterol 56(9):1126–1130
Kalady MF et al (2003) Loop ileostomy closure at an ambulatory surgery facility: a safe and cost-effective alternative to routine hospitalization. Dis Colon Rectum 46(4):486–90
Nguyen JMV, Bouchard-Fortier G, Covens A (2020) Same-day discharge of Gynecologic Oncology patients following ileostomy closure is feasible and safe. Gynecol Oncol 156(2):446–450
Taylor JP et al (2019) The safety of outpatient stoma closure: on the verge of a paradigm shift? J Gastrointest Surg 23(10):2019–2026
Nguyen J, Bouchard-Fortier G, Covens A (2018) Same-day discharge following ileostomy closure is feasible and safe. Int J Gynecol Cancer 28(Supplement 2):977
Fast Track Multimodal Management Versus Standard Care study, g. and g. Enhanced Recovery After Surgery, Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg 2006. 93(7):800-809
Spanjersberg WR et al (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev (2)
McKenna NP et al (2020) Is same-day and next-day discharge after laparoscopic colectomy reasonable in select patients? Dis Colon Rectum 63(10):1427–1435
Delaney CP (2008) Outcome of discharge within 24 to 72 hours after laparoscopic colorectal surgery. Dis Colon Rectum 51(2):181–185
Gignoux B et al (2019) Short-term outcomes of ambulatory colectomy for 157 consecutive patients. Ann Surg 270(2):317–321
Curfman KR et al (2022) Ambulatory colectomy: a pilot protocol for same day discharge in minimally invasive colorectal surgery. Am J Surg 224(2):757–760
Cavallaro P, Bordeianou L (2019) Implementation of an ERAS pathway in colorectal surgery. Clin Colon Rectal Surg 32(02):102–108
Kahokehr A et al (2009) Implementation of ERAS and how to overcome the barriers. Int J Surg 7(1):16–19
Phatak UR et al (2014) Impact of ileostomy-related complications on the multidisciplinary treatment of rectal cancer. Ann Surg Oncol 21(2):507–512
Younis J et al (2012) Focused preoperative patient stoma education, prior to ileostomy formation after anterior resection, contributes to a reduction in delayed discharge within the enhanced recovery programme. Int J Colorectal Dis 27(1):43–7
McGillion MH et al (2021) Post-discharge after surgery Virtual Care with Remote Automated Monitoring-1 (PVC-RAM-1) technology versus standard care: randomised controlled trial. BMJ 374:n2209
Colegate-Stone T et al (2011) Audit of trauma case load suitable for a day surgery trauma list and cost analysis. The Surgeon 9(5):241–244
Stephen AE, Berger DL (2003) Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery 133(3):277–82
Lee L et al (2015) Cost-effectiveness of enhanced recovery versus conventional perioperative management for colorectal surgery. Ann Surg 262(6):1026–1033
Allart KK et al (2021) Short-term outcomes of day-case stoma closure: a prospective, observational study. Dis Colon Rectum 64(11):1407–1416
Azin A et al (2017) The safety and feasibility of early discharge following ileostomy reversal: a National Surgical Quality Improvement Program analysis. J Surg Res 217:247–251
Berger NG et al (2017) Loop ileostomy closure as an overnight procedure: institutional comparison with the national surgical quality improvement project data set. Dis Colon Rectum 60(8):852–859
Bhalla A, Peacock O, Lund JN (2015) Response to: Ileostomy closure in an enhanced recovery setting. Colorectal Dis 17(10):929
Blane C, Chaudhary B, Pullyblank A (2015) Closure of ileostomy: can we improve efficiency without compromising patient safety? Int J Surg 23(SUPPL. 1):S50
Baraza W et al (2010) Postoperative management after loop ileostomy closure: are we keeping patients in hospital too long? Ann R Coll Surg Engl 92(1):51–5
Bracey E et al (2015) Ileostomy closure in an enhanced recovery setting. Colorectal Dis 17(10):917–21
Fahlke J et al (2004) Oncosurgical therapies in outpatient and short term inpatient surgery. Chir 75(2):144–152
Gatt M, Reddy BS, Mainprize KS (2007) Day-case stoma surgery: Is it feasible? Surgeon 5(3):143–147
Herrod PJJ, Lund JN (2017) Ileostomy reversal: length of stay can be safely decreased further to same-day discharge in many. Dis Colon Rectum 60(11):e632–e633
Hughes K, Hargreaves A, Arthur J (2012) Ileostomy reversal: is discharge within 23H feasible? Colorectal Dis 14(SUPPL. 2):50
Ihedioha U et al (2010) Closure of loop ileostomies: is early discharge safe and achievable? Scot Med J 55(1):27–9
Joh Y-G et al (2008) Standardized postoperative pathway: accelerating recovery after ileostomy closure. Dis Colon Rectum 51(12):1786–9
Karavaggelis A et al (2017) 23 hour closure of ileostomy-who will succeed? Colorectal Dis 19(Supplement 4):61
Keller DS et al (2014) Readmissions after ileostomy closure: cause to revisit a standardized enhanced recovery pathway? Am J Surg 208(4):650–655
Langelotz C et al (2008) “Fast-track” rehabilitation to enhance recovery after ileostomy closure - A prospective clinical trial. Zentralbl Chir 133(5):486–490
Lee L et al (2021) Enhanced recovery 2.0 — same day discharge with mobile app follow-up after minimally invasive colorectal surgery. Ann Surg 2021
Liang J et al (2021) Short stay (1 day) diverting loop ileostomy closure can be selectively implemented without an increase in readmission and complication rates: an ACS-NSQIP analysis. Dis Colon Rectum 64(5):229–230
Moran MR (1997) Same-day surgery ileostomy closure? Am J Manag Care 3(7):1003–6
Paré X, Morin G, Letarte F (2019) Loop ileostomy closure as a 23-hour stay procedure, a multi-center randomized controlled trial (ILEO). CHU de Quebec-Universite Laval
Peacock O et al (2011) Closure of loop ileostomy: potentially a daycase procedure? Colorectal Dis 13(SUPPL. 4):35
Peacock O et al (2012) A 23-h discharge protocol for loop ileostomy closures. Colorectal Dis 14(SUPPL. 2):5–6
Sabbagh C et al (2018) Identifying patients eligible for a short hospital stay after stoma closure. J Invest Surg 31(3):168–172
Springer-Verlag Erratum (2003) Dis Colon Rectum 46(7):903
Van Meter A et al (2013) Ileostomy take down in the outpatient setting: facilitated by the paravertebral block as a perioperative intervention. Ann Oncol 24 (SUPPL. 4)
Zhou PG, Hrabe J, Byrn J (2016) A retrospective, single-institution review of loop ileostomy reversal outcomes. Ostomy Wound Manag 62(8):22–33
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Victoria Archer designed the literature search. Victoria Archer, Zacharie Cloutier, and Annie Berg contributed to data extraction and analysis. Victoria Archer wrote the first draft of the manuscript. Tyler McKechnie, Wojtek Wiercioch, and Cagla Eskicioglu performed revisions and aided in the preparation of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Archer, V., Cloutier, Z., Berg, A. et al. Short-stay compared to long-stay admissions for loop ileostomy reversals: a systematic review and meta-analysis. Int J Colorectal Dis 37, 2113–2124 (2022). https://doi.org/10.1007/s00384-022-04256-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04256-x