Abstract
Background
Few studies to date have investigated morphological changes after neoadjuvant treatment (NAT) and their implications in total mesorectal excision (TME). This study was primarily designed to evaluate whether tissue changes associated with NAT affected the quality of TME and additionally to suggest a more objective method evaluating TME quality.
Methods
This study enrolled 1322 consecutive patients who underwent curative robot-assisted surgery for rectal cancer. Patients who did and did not receive NAT were subjected to propensity-score matching, yielding 402 patients in each group.
Results
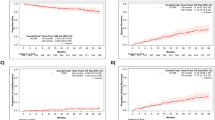
NAT independently reduced complete achievement of TME [odds ratio (OR) = 2.056, p = 0.017]. Intraoperative evaluation identified seven tissue changes significantly associated with NAT, including tumor perforation, mucin pool, necrosis, fibrosis, fat degeneration, and rectal or perirectal edema NAT (p < 0.001–0.05). Tumor perforation (OR = 5.299, p = 0.001) and mucin pool (OR = 14.053, p = 0.002) were independently associated with inappropriate (near-complete + incomplete) TME. Complete TME resulted in significantly reduced local recurrence (4.3% vs 15.3%, p = 0.003) and increased 5-year DFS rate (80.6% vs 67.6%, p = 0.047) compared with inappropriate one. By contrast, two tiers of complete and near-complete TMEs vs incomplete TME did not. Notably, among patients with complete TME, those who received NAT had a lower 5-year DFS than those who did not (77.8% vs 83.3%, p = 0.048).
Conclusions
NAT-associated tissue changes, somewhat interrupting complete TME, may provide unsolved clue to the relative inability of NAT to improve overall survival. The conventional three-tier grading of TME seems to be simplified into two tiers as complete and inappropriate.





Similar content being viewed by others
References
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH; Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Kim JC, Yu CS, Lim SB et al (2021) Re-evaluation of controversial issues in the treatment of cT3N0-2 rectal cancer: a 10-year cohort analysis using propensity-score matching. Int J Colorectal Dis 36:2649–2659
Kreis ME, Ruppert R, Kube R et al (2020) MRI-based use of neoadjuvant chemoradiotherapy in rectal carcinoma: surgical quality and histopathological outcome of the OCUM trial. Ann Surg Oncol 27:417–427
Glynne-Jones F, Wyrwicz L, Tiret E et al (2017) Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 28(Suppl 4):iv22-iv40
Mariathasan AB, Boye K, Giercksky KE et al (2018) Beyond total mesorectal excision in locally advanced rectal cancer with organ or pelvic side-wall involvement. Eur J Surg Oncol 44:1226–1232
Quirke P (2003) Training and quality assurance for rectal cancer: 20 years of data is enough. Lancet Oncol 4:695–702
Nagtegaal ID, van de Velde CJ, Marijnen CA, van Krieken JH, Quirke P (2005) Low rectal cancer: a call for a change of approach in abdominoperineal resection. J Clin Oncol 23:9257–9264
Campa-Thompson M, Weir R, Calcetera N, Quirke P, Carmack S (2015) Pathologic processing of the total mesorectal excision. Clin Colon Rectal Surg 28:43–52
Kim JC, Kim CW, Lee JL et al (2021) Complete intersphincteric longitudinal muscle excision may be key to reducing local recurrence during intersphincteric resection. Eur J Surg Oncol 47:1629–1636
van Gijn W, Marijnen CA, Nagtegaal ID et al (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12:575–582
Wibe A, Eriksen MT, Syse A, Myrvold HE, Søreide O; Norwegian Rectal Cancer Group (2003) Total mesorectal excision for rectal cancer-what can be achieved by a national audit? Colorectal Dis 5:471–477
Lansu J, Braam PM, van Werkhoven E et al (2021) A moderate dose of preoperative radiotherapy may improve resectability in myxoid liposarcoma. Eur J Surg Oncol 47:2633–2639
Borrelli MR, Patel RA, Sokol J et al (2019) Fat chance: The rejuvenation of irradiated skin. Plast Reconstr Surg Glob Open 7:e2092
Vazzano J, Frankel WL, Wolfe AR, Williams TM, Chen W (2021) Morphologic changes associated with neoadjuvant-treated pancreatic ductal adenocarcinoma and comparison of two tumor regression grading systems. Hum Pathol 109:1–11
Leonard D, Penninckx F, Fieuws S et al (2010) Factors predicting the quality of total mesorectal excision for rectal cancer. Ann Surg 252:982–988
Sirák I, Pohanková D, Ferko A et al (2020) The time between chemoradiation and surgery for rectal carcinoma negatively influences mesorectal excision quality. Pathol Oncol Res 26:1565–1572
Reggiani Bonetti L, Domati F, Farinetti A, Migaldi M, Manenti A (2015) Radiotherapy-induced mesorectum alterations: histological evaluation of 90 consecutive cases. Scand J Gastroenterol 50:197–203
Trott KR, Doerr W, Facoetti A et al (2012) Biological mechanisms of normal tissue damage: importance for the design of NTCP models. Radiother Oncol 105:79–85
O’Sullivan B, Davis AM, Turcotte T et al (2002) Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limb: a randomized trial. Lancet 359:2235–2241
Nagtegaal I, Gaspar C, Marijnen C, Van De Velde C, Fodde R, Van Krieken H (2004) Morphological changes in tumour type after radiotherapy are accompanied by changes in gene expression profile but not in clinical behaviour. J Pathol 204:183–192
Nikberg M, Kindler C, Chabok A, Letocha H, Shetye J, Smedh K (2015) Circumferential resection margin as a prognostic marker in the modern multidisciplinary management of rectal cancer. Dis Colon Rectum 58:275–282
Lee J, Chen F, Steel M, Keck J, Mackay J (2006) Perforated rectal cancer associated with neoadjuvant radiotherapy: report of four cases. Dis Colon Rectum 49:1629–1632
Sebag-Montefiore D, Stephens RJ, Steele R et al (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet 373:811–820
Sauer R, Liersch T, Merkel S et al (2012) Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol 30:1926–1933
Tanaka S, Martling A, Lindholm J, Holm T, Palmer G (2015) Remaining cancer cells within the fibrosis after neo-adjuvant treatment for locally advanced rectal cancer. Eur J Surg Oncol 41:1204–1209
Rose BS, Winer EP, Mamon HJ (2016) Perils of the pathologic complete response. J Clin Oncol 34:3959–3962
Moreno CC, Sullivan PS, Mittal PK (2018) Rectal MRI for cancer staging and surveillance. Gastroenterol Clin North Am 47:537–552
Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH (2002) Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol 26:350–357
Acknowledgements
The authors would like to thank Hyo Seon Yu, MD, Mi Young Park, MD, Jay Jung, MD, Hyun Joo Jeong, RN, and Jung Rang Kim, RN., for their support with data enrollment, collection, and update.
Author information
Authors and Affiliations
Contributions
Jin Cheon Kim, and Tae Won Kim contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jin Cheon Kim, Seong Ho Park, Jihun Kim, Chan Wook Kim, In Ja Park, Yong Sik Yoon, Jong Lyul Lee, Jong Hoon Kim, Yong Sang Hong, and Tae Won Kim. The first draft of the manuscript was written by Jin Cheon Kim and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approved by the Institutional Review Board of Asan Medical Center (registration number: 2021–1851).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, J.C., Park, S.H., Kim, J. et al. Involvement of tissue changes induced by neoadjuvant treatment in total mesorectal excision (TME): novel suggestions for determining TME quality. Int J Colorectal Dis 37, 1289–1300 (2022). https://doi.org/10.1007/s00384-022-04165-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04165-z