Abstract
Purpose
Brain metastasis (BM) in colorectal cancer patients is rare and is associated with dismal outcomes. Our study aims to evaluate the incidence and predictors of BM in patients with colorectal cancer.
Methods
We performed a retrospective analysis (2010–2017) of patients with a primary diagnosis of colorectal cancer (CRC). Patients were stratified into two groups (BM vs. No-BM). Outcome measures were the incidence and predictors of BM. Multivariate logistic regression analysis was performed.
Results
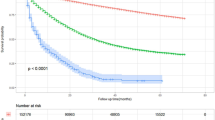
A total of 230,806 patients were analyzed. A total of 0.30% (n = 691) of the patients were found to have BM. On multivariate logistics regression, bone (OR: 5.39 [3.36–8.65], p < 0.001), lung (OR: 3.75 [2.67–5.28], < 0.001), and distant node metastasis (OR: 32.75 [20.47–52.41], p < 0.001) were independent predictors of BM.
Conclusion
Our study supports the low incidence of brain metastasis in patients with colorectal cancer. A unique set of characteristics is identified to confer an increased risk of brain metastases.
Similar content being viewed by others
Data availability
Not applicable.
Code availability
Surveillance, Epidemiology, and End Results Program (SEER) Data.
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA: A Cancer J Clinic. 69(1):7–34. https://doi.org/10.3322/caac.21551
Kuipers EJ, Grady WM, Lieberman D, Seufferlein T, Sung JJ, Boelens PG, van de Velde CJ, Watanabe T (2015) Colorectal cancer. Nat Rev Dis Prime 1:15065. https://doi.org/10.1038/nrdp.2015.65
Disibio G, French SW (2008) Metastatic patterns of cancers: results from a large autopsy study. Arch Pathol Lab Med 132:931–939
Hess KR, Varadhachary GR, Taylor SH, Wei W, Raber MN, Lenzi R, Abbruzzese JL (2006) Metastatic patterns in adenocarcinoma. Cancer 106:1624–1633
Weiss L, Grundmann E, Torhorst J, Hartveit F, Moberg I, Eder M, Fenoglio-Preiser CM, Napier J, Horne CH, Lopez MJ et al (1986) Haematogenous metastatic patterns in colonic carcinoma: an analysis of 1541 necropsies. J Pathol 150:195–203
Go PH, Klaassen Z, Meadows MC, Chamberlain RS (2011) Gastrointestinal cancer and brain metastasis: a rare and ominous sign. Cancer 117(16):3630–3640. https://doi.org/10.1002/cncr.25940
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14(1):48–54
Damiens K, Ayoub JP, Lemieux B, Aubin F, Saliba W, Campeau MP, Tehfe M (2012) Clinical features and course of brain metastases in colorectal cancer: an experience from a single institution. Current Oncol (Toronto, Ont.), 19(5), 254–258. https://doi.org/10.3747/co.19.1048
Lemke J, Scheele J, Kapapa T et al (2014) Brain metastases in gastrointestinal cancers: is there a role for surgery? Int J Mol Sci 15(9):16816–16830. https://doi.org/10.3390/ijms150916816
Christensen TD, Palshof JA, Larsen FO, Høgdall E, Poulsen TS, Pfeiffer P, Jensen BV, Yilmaz MK, Christensen IJ, Nielsen D (2017) Risk factors for brain metastases in patients with metastatic colorectal cancer. Acta Oncol 56(5):639–645. https://doi.org/10.1080/0284186X.2017.1290272 (Epub 2017 Feb 22 PubMed PMID: 28447565)
Nozawa H, Ishihara S, Kawai K, Sasaki K, Murono K, Otani K, Nishikawa T, Tanaka T, Kiyomatsu T, Hata K, Watanabe T (2017) Brain metastasis from colorectal cancer: predictors and treatment outcomes. Oncology 93(5):309–314. https://doi.org/10.1159/000478661 (Epub 2017 Jul 13 PubMed PMID: 28700994)
Mostafa G, Matthews BD, Norton HJ, Kercher KW, Sing RF, Heniford BT (2004) Influence of demographics on colorectal cancer. Am Surg 70(3):259–264 (PubMed PMID: 15055851)
Surveillance, Epidemiology, and End Results (SEER) (2018) Program (www.seer.cancer.gov) SEER*Stat Database: Populations - Total U.S. (1969–2017) <Katrina/Rita Adjustment> - Linked To County Attributes - Total U.S., 1969–2017 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released December 2018
Padera TP, Meijer EF, Munn LL (2016) The lymphatic system in disease processes and cancer progression. Annu Rev Biomed Eng 18:125–158. https://doi.org/10.1146/annurev-bioeng-112315-031200
Jones D, Pereira ER, Padera TP (2018) Growth and immune evasion of lymph node metastasis. Front Oncol 8:36. Published 2018 Feb 21. https://doi.org/10.3389/fonc.2018.00036
Mo S, Cai X, Zhou Z et al (2020) Nomograms for predicting specific distant metastatic sites and overall survival of colorectal cancer patients: a large population-based real-world study. Clin Transl Med 10(1):169–181. https://doi.org/10.1002/ctm2.20
Hugen N, van De Velde CJH, Wilt JHWD, Nagtegaal ID (2014) Metastatic pattern in colorectal cancer is strongly influenced by histological subtype. Ann Oncol 2014;25(3):651–657. https://doi.org/10.1093/annonc/mdt591
Hall SA, Kaufman JS, Ricketts TC (2006) Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health 83(2):162–175. https://doi.org/10.1007/s11524-005-9016-3
Mathot L, Stenninger J (2012) Behavior of seeds and soil in the mechanism of metastasis: a deeper understanding. Cancer Sci 103:626–631. https://doi.org/10.1111/j.1349-7006.2011.02195.x
Yaeger R, Cowell E, Chou JF, Gewirtz AN, Borsu L, Vakiani E, Solit DB, Rosen N, Capanu M, Ladanyi M, Kemeny N (2015) RAS mutations affect pattern of metastatic spread and increase propensity for brain metastasis in colorectal cancer. Cancer 121(8):1195–203. https://doi.org/10.1002/cncr.29196. Epub 2014 Dec 9. PMID: 25491172; PMCID: PMC4523078
Brain metastases from colorectal cancer: risk factors, incidence, and the possible role of chemokines, clinical colorectal cancer (2009) 8(2):100–105. ISSN 1533–0028. https://doi.org/10.3816/CCC.2009.n.016.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Data acquisition was performed by Elishia Thompson BS, Shoujit Banerjee BA, Sierra Thompson MSc, and Andrew Muse BS. The statistical analysis was performed by Elishia Thompson BS and Andrew Muse BS. The manuscript writing and critical revisions were performed by all the authors. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Poster Presentation at the Western Surgical Association, November 2019; Las Vegas, Nevada, USA
Rights and permissions
About this article
Cite this article
Thompson, E., Banerjee, S., Thompson, S. et al. Incidence and predictors of brain metastasis in colorectal cancer patients. Int J Colorectal Dis 37, 153–159 (2022). https://doi.org/10.1007/s00384-021-04041-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-04041-2