Abstract
Purpose
Intestinal failure (IF) is defined by the reduction of gut function under the minimum necessary for adequate absorption of macronutrients and/or electrolytes, requiring home parenteral nutrition (HPN) to maintain health and/or growth. Among the different causes of IF, short bowel syndrome (SBS) is one of the main causes of IF in adults. Management of IF and SBS is complex and requires a multidisciplinary approach. The aim of this study was to review the place and the modalities of conservative surgical procedures performed for IF in adults.
Results-conclusion
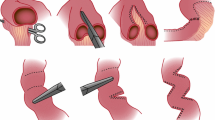
HPN has drastically modified the poor prognosis of these patients, leading to an overall survival around 70–75% at 5 years in patients without cancer. However, HPN is associated with life-threatening long-term complications, including liver failure and catheter-related complications, main causes of deaths for these patients. Surgery can be proposed, in order to try to reduce SBS consequences with either conservative or non-conservative procedures. Simple bowel continuity restoration should be performed as often as possible in order to wean or at least to reduce HPN. Lengthening procedures are proposed to increase the absorption surface of the remnant bowel. These procedures can be only performed on a dilated small bowel. The slowing transit time procedure is represented by segmental reversal of the small bowel. Intestinal transplantation is the last surgical option for patients with IF but is still today associated with high mortality and failure rates. Thus, conservative procedures have a major role in the surgical armentarium for patients with IF.




Similar content being viewed by others
Data availability
Not applicable
Code availability
Not applicable
References
Fleming CR, Remington M (1981) Intestinal failure. In: Hill GL (ed) Nutrition and the surgical patient. Churchill Livingstone, Edinburgh, pp 219–235
O’Keefe SJ (2006) Bacterial overgrowth and liver complications in short bowel intestinal failure patients. Gastroenterology 130:67–69
Pironi L, Arends J, Baxter J, Bozzetti F, Peláez RB, Cuerda C, Forbes A, Gabe S, Gillanders L, Holst M, Jeppesen PB, Joly F, Kelly D, Klek S, Irtun Ø, Olde Damink SW, Panisic M, Rasmussen HH, Staun M, Szczepanek K, van Gossum A, Wanten G, Schneider SM, Shaffer J, Home Artificial Nutrition & Chronic Intestinal Failure, Acute Intestinal Failure Special Interest Groups of ESPEN (2015) ESPEN endorsed recommendations. Definition and classification of intestinal failure in adults. Clin Nutr 34:171–180
Shaffer J (2002) Definition and service development. Clin Nutr 21:144–145
Pironi L, Konrad D, Brandt C, Joly F, Wanten G, Agostini F, Chambrier C, Aimasso U, Zeraschi S, Kelly D, Szczepanek K, Jukes A, di Caro S, Theilla M, Kunecki M, Daniels J, Serlie M, Poullenot F, Wu J, Cooper SC, Rasmussen HH, Compher C, Seguy D, Crivelli A, Pagano MC, Hughes SJ, Guglielmi FW, Kozjek NR, Schneider SM, Gillanders L, Ellegard L, Thibault R, Matras P, Zmarzly A, Matysiak K, van Gossum A, Forbes A, Wyer N, Taus M, Virgili NM, O'Callaghan M, Chapman B, Osland E, Cuerda C, Sahin P, Jones L, Lee ADW, Bertasi V, Orlandoni P, Izbéki F, Spaggiari C, Díez MB, Doitchinova-Simeonova M, Garde C, Serralde-Zúñiga AE, Olveira G, Krznaric Z, Czako L, Kekstas G, Sanz-Paris A, Jáuregui EP, Murillo AZ, Schafer E, Arends J, Suárez-Llanos JP, Shaffer J, Lal S (2018) Clinical classification of adult patients with chronic intestinal failure due to benign disease: an international multicenter cross-sectional survey. Clin Nutr 37:728–738
Nightingale JM (1994) The Sir David Cuthbertson Medal lecture. Clinical problems of a short bowel and their treatment. Proc Nutr Soc 53:373–391
Amiot A, Messing B, Corcos O, Panis Y, Joly F (2013) Determinants of home parenteral nutrition dependence and survival of 268 patients with non-malignant short bowel syndrome. Clin Nutr 32:368–374
Nightingale JM, Lennard-Jones JE (1995) Adult patients with a short bowel due to Crohn’s disease often start with a short normal bowel. Eur J Gastroenterol Hepatol 7:989–991
Nightingale J, Woodward JM (2006) Guidelines for management of patients with a short bowel. Gut 55:iv1–iv12
Jeppesen PB (2014) Spectrum of short bowel syndrome in adults: intestinal insufficiency to intestinal failure. JPEN J Parenter Enteral Nutr 38:8S–13S
Buchman AL, Scolapio J, Fryer J (2003) AGA technical review on short bowel syndrome and intestinal transplantation. Gastroenterology 124:1111–1134
Carbonnel F, Cosnes J, Chevret S, Beaugerie L, Ngô Y, Malafosse M, Parc R, le Quintrec Y, Gendre JP (1996) The role of anatomic factors in nutritional autonomy after extensive small bowel resection. JPEN J Parenter Enteral Nutr 20:275–280
Tappenden KA (2014) Intestinal adaptation following resection. JPEN J Parenter Enteral Nutr 38:23S–31S
Goulet O, Ruemmele F, Lacaille F, Colomb V (2004) Irreversible intestinal failure. J Pediatr Gastroenterol Nutr 38:250–269
Barksdale EM, Stanford A (2002) The surgical management of short bowel syndrome. Curr Gastroenterol Rep 4:229–237
Le Beyec J, Billiauws L, Bado A et al (2020) Short bowel syndrome: a paradigm for intestinal adaptation to nutrition? Annu Rev Nutr 40:299–321
Pironi L (2016) Definitions of intestinal failure and the short bowel syndrome. Best Pract Res Clin Gastroenterol 30:173–185
Jeppesen PB, Gilroy R, Pertkiewicz M, Allard JP, Messing B, O'Keefe SJ (2011) Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 60:902–914
Joly F, Seguy D, Nuzzo A, Chambrier C, Beau P, Poullenot F, Thibault R, Armengol Debeir L, Layec S, Boehm V, Lallemand J, Quilliot D, Schneider SM (2020) Six-month outcomes of teduglutide treatment in adult patients with short bowel syndrome with chronic intestinal failure: a real-world French observational cohort study. Clin Nutr 39:2856–2862
Grant D, Abu-Elmagd K, Mazariegos G, Vianna R, Langnas A, Mangus R, Farmer DG, Lacaille F, Iyer K, Fishbein T, Intestinal Transplant Association (2015) Intestinal transplant registry report: global activity and trends. Am J Transplant 15:210–219
Broviac JW, Scribner BH (1974) Prolonged parenteral nutrition in the home. Surg Gynecol Obstet 139:24–28
Howard L, Ament M, Fleming CR et al (1995) Current use and clinical outcome of home parenteral and enteral nutrition therapies in the United States. Gastroenterology 109:355–365
Pironi L, Boeykens K, Bozzetti F, Joly F, Klek S, Lal S, Lichota M, Mühlebach S, van Gossum A, Wanten G, Wheatley C, Bischoff SC (2020) ESPEN guideline on home parenteral nutrition. Clin Nutr 39:1645–1666
Pironi L, Arends J, Bozzetti F, Cuerda C, Gillanders L, Jeppesen PB, Joly F, Kelly D, Lal S, Staun M, Szczepanek K, van Gossum A, Wanten G, Schneider SM, Home Artificial Nutrition & Chronic Intestinal Failure Special Interest Group of ESPEN (2016) ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr 35:247–307
Abu-Elmagd KM, Armanyous SR, Fujiki M, Parekh NR, Osman M, Scalish M, Newhouse E, Fouda Y, Lennon E, Shatnawei A, Kirby D, Steiger E, Khanna A, Radhakrishnan K, Quintini C, Hashimoto K, Barnes J, Costa G (2019) Management of five hundred patients with gut failure at a single center: surgical innovation versus transplantation with a novel predictive model. Ann Surg 270:656–674
Baldwin-Price HK, Copp D, Singleton AO Jr (1965) Reversed intestinal segments in the management of anenteric malabsorption syndrome. Ann Surg 161:225–230
Rege AS, Sudan DL (2013) Autologous gastrointestinal reconstruction: review of the optimal nontransplant surgical options for adults and children with short bowel syndrome. Nutr Clin Pract 28:65–74
Figueroa-Colon R, Harris PR, Birdsong E, Franklin FA, Georgeson KE (1996) Impact of intestinal lengthening on the nutritional outcome for children with short bowel syndrome. J Pediatr Surg 31:912–916
Kim HB, Fauza D, Garza J, Oh JT, Nurko S, Jaksic T (2003) Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg 38:425–429
Brolin RE (1986) Colon interposition for extreme short bowel syndrome: a case report. Surgery 100:576–580
Murphy F, Khalil BA, Gozzini S, King B, Bianchi A, Morabito A (2011) Controlled tissue expansion in the initial management of the short bowel state. World J Surg 35:1142–1145
Sogawa H, Costa G, Armanyous S et al (2019) Twenty years of gut transplantation for chronic intestinal pseudo-obstruction: technical innovation, long-term outcome, quality of life, and disease recurrence. Ann Surg 273:325–333
Thompson JS (2016) Reversed intestinal segment revisited. Transplant Proc 48:453–456
Messing B, Crenn P, Beau P, Boutron-Ruault MC, Rambaud JC, Matuchansky C (1999) Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 117:1043–1050
Adaba F, Rajendran A, Patel A, Cheung YK, Grant K, Vaizey CJ, Gabe SM, Warusavitarne J, Nightingale JMD (2015) Mesenteric infarction clinical outcomes after restoration of bowel continuity. Ann Surg 262:1059–1064
Cruz RJ, McGurgan J, Butera L et al (2020) Gastrointestinal tract reconstruction in adults with ultra-short bowel syndrome: surgical and nutritional outcomes. Surgery 168:297–304
Bianchi A (1980) Intestinal loop lengthening-a technique for increasing small intestinal length. J Pediatr Surg 15:145–151
Aigrain Y, Cornet D, Cezard JP, Boureau M (1985) Longitudinal division of small intestine: a surgical possibility for children with the very short bowel syndrome. Z Kinderchir 40:233–236
Boeckman CR, Traylor R (1981) Bowel lengthening for short gut syndrome. J Pediatr Surg 16:996–997
Weber TR, Powell MA (1996) Early improvement in intestinal function after isoperistaltic bowel lengthening. J Pediatr Surg 31:61–64
Chang RW, Javid PJ, Oh JT, Andreoli S, Kim HB, Fauza D, Jaksic T (2006) Serial transverse enteroplasty enhances intestinal function in a model of short bowel syndrome. Ann Surg 243:223–228
Sudan D, Thompson J, Botha J, Grant W, Antonson D, Raynor S, Langnas A (2007) Comparison of intestinal lengthening procedures for patients with short bowel syndrome. Ann Surg 246:593–601
Miyasaka EA, Brown PI, Teitelbaum DH (2011) Redilation of bowel after intestinal lengthening procedures-an indicator for poor outcome. J Pediatr Surg 46:145–149
Cserni T, Biszku B, Guthy I, Dicso F, Szaloki L, Folaranmi S, Murphy F, Rakoczy G, Bianchi A, Morabito A (2014) The first clinical application of the spiral intestinal lengthening and tailoring (silt) in extreme short bowel syndrome. J Gastrointest Surg 18:1852–1857
Coletta R, Aldeiri B, Morabito A (2018) Institutional experience with spiral intestinal lengthening and tailoring. Eur J Pediatr Surg 29:412–416
Panis Y, Messing B, Rivet P et al (1997) Segmental reversal of the small bowel as an alternative to intestinal transplantation in patients with-short bowel syndrome. Ann Surg 225:401–407
Beyer-Berjot L, Joly F, Maggiori L, Corcos O, Bouhnik Y, Bretagnol F, Panis Y (2012) Segmental reversal of the small bowel can end permanent parenteral nutrition dependency: an experience of 38 adults with short bowel syndrome. Ann Surg 256:739–745
Layec S, Beyer L, Corcos O, Alves A, Dray X, Amiot A, Stefanescu C, Coffin B, Bretagnol F, Bouhnik Y, Messing B, Panis Y, Kapel N, Joly F (2013) Increased intestinal absorption by segmental reversal of the small bowel in adult patients with short-bowel syndrome: a case-control study. Am J Clin Nutr 97:100–108
Hutcher NE, Salzberg AM (1971) Pre-ileal transposition of colon to prevent the development of short bowel syndrome in puppied with 90 percent small intestinal resection. Surgery 70:189–197
Glick PL, de Lorimier AA, Scott Adzick N, Harrison MR (1984) Colon interposition: an adjuvant operation for short-gut syndrome. J Pediatr Surg 19:719–725
Kono K, Sekikawa T, Iizuka H, Takahashi A, Amemiya H, Takehana T, Ooi A, Fujii H, Matsumoto Y (2001) Interposed colon between remnants of the small intestine exhibits small bowel features in a patient with short bowel syndrome. Dig Surg 18:237–241
Taha MO, Ribeiro MA, de Oliveira Gomes P et al (1999) Evaluation of the longitudinal musculature of segments of the distal colon interposed following extended jejunum-ileum resection. Microsurgery 19:306–310
Grieco GA, Reyes HM, Ostrovsky E (1983) The role of a modified intussusception jejunocolic valve in short-bowel syndrome. J Pediatr Surg 18:354–358
Jeppesen PB, Hartmann B, Thulesen J, Graff J, Lohmann J, Hansen BS, Tofteng F, Poulsen SS, Madsen JL, Holst JJ, Mortensen PB (2001) Glucagon-like peptide 2 improves nutrient absorption and nutritional status in short-bowel patients with no colon. Gastroenterology 120:806–815
Jeppesen PB, Gabe SM, Seidner DL, Lee HM, Olivier C (2018) Factors associated with response to teduglutide in patients with short-bowel syndrome and intestinal failure. Gastroenterology 154:874–885
Slim GM, Lansing M, Wizzard P, Nation PN, Wheeler SE, Brubaker PL, Jeppesen PB, Wales PW, Turner JM (2019) Novel long-acting GLP-2 analogue, FE 203799 (apraglutide), enhances adaptation and linear intestinal growth in a neonatal piglet model of short bowel syndrome with total resection of the ileum. JPEN J Parenter Enteral Nutr 43:891–898
Hvistendahl MK, Naimi RM, Enevoldsen LH, Madsen JL, Fuglsang S, Jeppesen PB (2020) Effect of glepaglutide, a long-acting glucagon-like peptide-2 analog, on gastrointestinal transit time and motility in patients with short bowel syndrome: findings from a randomized trial. JPEN J Parenter Enteral Nutr 44:1535–1544
Naimi RM, Hvistendahl M, Enevoldsen LH, Madsen JL, Fuglsang S, Poulsen SS, Kissow H, Pedersen J, Nerup N, Ambrus R, Achiam MP, Svendsen LB, Holst JJ, Hartmann B, Hansen SH, Dragsted LO, Steensberg A, Mouritzen U, Hansen MB, Jeppesen PB (2019) Glepaglutide, a novel long-acting glucagon-like peptide-2 analogue, for patients with short bowel syndrome: a randomised phase 2 trial. Lancet Gastroenterol Hepatol 4:354–363
Lauro A, Panaro F, Iyer KR (2017) An overview of EU and USA intestinal transplant current activity. J Visc Surg 154:105–114
Beyer-Berjot L, Joly F, Dokmak S, Bretagnol F, Corcos O, Bouhnik Y, Belghiti J, Panis Y (2012) Intestinal transplantation: indications and prospects. J Visc Surg 149:380–384
Ueno T, Fukuzawa M (2010) Current status of intestinal transplantation. Surg Today 40:1112–1122
Pironi L, Joly F, Forbes A, Colomb V, Lyszkowska M, Baxter J, Gabe S, Hebuterne X, Gambarara M, Gottrand F, Cuerda C, Thul P, Messing B, Goulet O, Staun M, van Gossum A, Home Artificial Nutrition & Chronic Intestinal Failure Working Group of the European Society for Clinical Nutrition and Metabolism (ESPEN) (2011) Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut 60:17–25
Jones BA, Hull MA, Potanos KM, Zurakowski D, Fitzgibbons SC, Ching YA, Duggan C, Jaksic T, Kim HB, International STEP Data Registry (2013) Report of 111 consecutive patients enrolled in the International Serial Transverse Enteroplasty (STEP) Data Registry: a retrospective observational study. J Am Coll Surg 216:438–446
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aubert, M., Mege, D., Billiauws, L. et al. State-of-the-art colorectal disease: conservative surgical management of intestinal failure in adults. Int J Colorectal Dis 36, 1597–1607 (2021). https://doi.org/10.1007/s00384-021-03863-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03863-4