Abstract
Purpose
Two subgroups of fecal incontinence (FI) are described in literature and used in clinical practice. However, the pertinence of this classification of FI is still unknown as there are no clear established guidelines. To a better understanding, we performed a systematic review to characterize the different types of FI (active, passive, or mixed) on the basis of clinical presentation and complementary explorations.
Methods
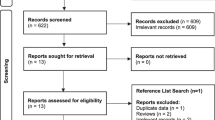
This systematic literature review was performed in reference to recommendations for systematic review using PRISMA guidelines without date restriction, until May 2020. This systematic review was performed without temporal limitation using MEDLINE-PubMed, Cochrane Library, and Google Scholar databases.
Results
Six hundred nine unique citations were identified from all the databases combined. Of those, 21 studies met the inclusion criteria, with 8 retrospective observational studies and 13 prospective observational studies. There was a lack of homogeneity in definitions of passive and urge (active) FI among studies. Prevalence of passive and urge FI was respectively of 4.0–5.0 and 15.0–35.0%. Clinical characteristics, physical examination, and endoanal imaging were not evaluated in most studies. In anorectal manometry, maximal squeeze pressure was higher in passive FI subgroup in most studies and results regarding maximal resting pressure remain discordant. There seemed to be no difference regarding first sensation volume and maximal tolerable volume among subgroups. A few studies evaluated pudendal terminal nerve motor latency with no difference among subgroups.
Conclusion
There is a lack of well-conducted prospective studies comparing the different subtypes of FI with validated definitions in both clinical and paraclinical examinations.

Similar content being viewed by others
Data availability
Not applicable.
References
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, Cottenden A, Davila W, de Ridder D, Dmochowski R, Drake M, Dubeau C, Fry C, Hanno P, Smith JH, Herschorn S, Hosker G, Kelleher C, Koelbl H, Khoury S, Madoff R, Milsom I, Moore K, Newman D, Nitti V, Norton C, Nygaard I, Payne C, Smith A, Staskin D, Tekgul S, Thuroff J, Tubaro A, Vodusek D, Wein A, Wyndaele JJ, Members of Committees, Fourth International Consultation on Incontinence (2010) Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 29:213–240
Whitehead WE, Simren M, Busby-Whitehead J et al (2020) Fecal incontinence diagnosed by the Rome IV criteria in the United States, Canada, and the United Kingdom. Clin Gastroenterol Hepatol 18(2):385–391
Ng K-S, Sivakumaran Y, Nassar N, Gladman MA (2015) Fecal incontinence: community prevalence and associated factors--a systematic review. Dis Colon Rectum 58:1194–1209
Damon H, Schott AM, Barth X, Faucheron JL, Abramowitz L, Siproudhis L, Fayard MO, Colin C, Valancogne G, Bonniaud V, Mion F, The French ORALIA Group (2008) Clinical characteristics and quality of life in a cohort of 621 patients with faecal incontinence. Int J Color Dis 23:845–851
Miner PB (2004) Economic and personal impact of fecal and urinary incontinence. Gastroenterology 126:S8–S13
Mullen PJ (1992) Faecal urge incontinence caused by exercise. BMJ 305:956
Engel AF, Kamm MA, Bartram CI, Nicholls RJ (1995) Relationship of symptoms in faecal incontinence to specific sphincter abnormalities. Int J Color Dis 10:152–155
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Burns PB, Rohrich RJ, Chung KC (2011) The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg 128:305–310
Gee AS, Durdey P (1995) Urge incontinence of faeces is a marker of severe external anal sphincter dysfunction. Br J Surg 82:1179–1182
Vaizey CJ, Kamm MA, Bartram CI (1997) Primary degeneration of the internal anal sphincter as a cause of passive faecal incontinence. Lancet 349:612–615
Herbst F, Kamm M, Morris G et al (1997) Gastrointestinal transit and prolonged ambulatory colonic motility in health and faecal incontinence. Gut 41:381–389
Glia A, Gylin M, Akerlund JE et al (1998) Biofeedback training in patients with fecal incontinence. Dis Colon Rectum 41:359–364
Salvioli B, Bharucha AE, Rath-Harvey D, Pemberton JH, Phillips SF (2001) Rectal compliance, capacity, and rectoanal sensation in fecal incontinence. Am J Gastroenterol 96:2158–2168
Gladman MA, Scott SM, Chan CLH et al (2003) Rectal hyposensitivity: prevalence and clinical impact in patients with intractable constipation and fecal incontinence. Dis Colon Rectum 46:238–246
Soligo M, Salvatore S, Milani R, Lalia M, Malberti S, Digesu GA, Mariani S (2003) Double incontinence in urogynecologic practice: a new insight. Am J Obstet Gynecol 189:438–443
Mimura T, Kaminishi M, Kamm MA (2004) Diagnostic evaluation of patients with faecal incontinence at a specialist institution. Dig Surg 21:235–241 discussion 241
Chan CLH, Scott SM, Williams NS, Lunniss PJ (2005) Rectal hypersensitivity worsens stool frequency, urgency, and lifestyle in patients with urge fecal incontinence. Dis Colon Rectum 48:134–140
Chan CLH, Lunniss PJ, Wang D, Williams NS, Scott SM (2005) Rectal sensorimotor dysfunction in patients with urge faecal incontinence: evidence from prolonged manometric studies. Gut 54:1263–1272
Bharucha AE, Zinsmeister AR, Locke GR et al (2006) Symptoms and quality of life in community women with fecal incontinence. Clin Gastroenterol Hepatol 4:1004–1009
Deutekom M, Dobben AC, Terra MP, Engel AF, Stoker J, Bossuyt PMM, Boeckxstaens GEE (2007) Clinical presentation of fecal incontinence and anorectal function: what is the relationship? Am J Gastroenterol 102:351–361
Rodger CJ, Nicol L, Anderson JH, McKee RF, Finlay IG (2010) Abnormal colonic motility: a possible association with urge fecal incontinence. Dis Colon Rectum 53:409–413
Hornung BR, Mitchell PJ, Carlson GL, Klarskov N, Lose G, Kiff ES (2012) Comparative study of anal acoustic reflectometry and anal manometry in the assessment of faecal incontinence. Br J Surg 99:1718–1724
Muñoz-Yagüe T, Solís-Muñoz P, Ciriza de los Ríos C et al (2014) Fecal incontinence in men: causes and clinical and manometric features. World J Gastroenterol 20:7933–7940
van Meegdenburg MM, Heineman E, Broens PMA (2015) Pudendal neuropathy alone results in urge incontinence rather than in complete fecal incontinence. Dis Colon Rectum 58:1186–1193
Thiruppathy K, Mason J, Akbari K, Raeburn A, Emmanuel A (2017) Physiological study of the anorectal reflex in patients with functional anorectal and defecation disorders. J Dig Dis 18:222–228
van Meegdenburg MM, Meinds RJ, Trzpis M, Broens PMA (2018) Subtypes and symptoms of fecal incontinence in the Dutch population: a cross-sectional study. Int J Color Dis 33:919–925
Pahwa AK, Khanijow KD, Harvie HS et al (2020) Comparison of patient impact and clinical characteristics between urgency and passive fecal incontinence phenotypes. Female Pelvic Med Reconstr Surg 6(9):570–574
Heitmann PT, Rabbitt P, Schloithe A, Patton V, Skuza PP, Wattchow DA, Dinning PG (2019) Relationships between the results of anorectal investigations and symptom severity in patients with faecal incontinence. Int J Color Dis 34:1445–1454
Lynch AC, Wong C, Anthony A, Dobbs BR, Frizelle FA (2000) Bowel dysfunction following spinal cord injury: a description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord 38:717–723
Anon Drossman L, Chey WE, Kellow J et al (2016) Functional gastrointestinal disorders; disorders of gut-brain interaction. Raleigh, North Carolina: Rome Foundation
Bharucha AE, Dunivan G, Goode PS, Lukacz ES, Markland AD, Matthews CA, Mott L, Rogers RG, Zinsmeister AR, Whitehead WE, Rao SSC, Hamilton FA (2015) Epidemiology, pathophysiology, and classification of fecal incontinence: state of the science summary for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) workshop. Am J Gastroenterol 110:127–136
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Pescatori M, Anastasio G, Bottini C, Mentasti A (1992) New grading and scoring for anal incontinence. Evaluation of 335 patients. Dis Colon Rectum 35:482–487
Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC (1999) Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum 42:1525–1532
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Cotterill N, Norton C, Avery KNL, Abrams P, Donovan JL (2011) Psychometric evaluation of a new patient-completed questionnaire for evaluating anal incontinence symptoms and impact on quality of life: the ICIQ-B. Dis Colon Rectum 54:1235–1250
Sansoni J, Hawthorne G, Fleming G, Marosszeky N (2013) The revised faecal incontinence scale: a clinical validation of a new, short measure for assessment and outcomes evaluation. Dis Colon Rectum 56:652–659
Kwon S, Visco AG, Fitzgerald MP, Ye W, Whitehead WE, Pelvic Floor Disorders Network (PFDN) (2005) Validity and reliability of the Modified Manchester Health Questionnaire in assessing patients with fecal incontinence. Dis Colon Rectum 48:323–331 discussion 331-334
Knowles CH (2018) Human studies of anorectal sensory function. Ir J Med Sci 187:1143–1147
Ng K-S, Brookes SJ, Montes-Adrian NA, Mahns DA, Gladman MA (2016) Electrophysiological characterization of human rectal afferents. Am J Physiol Gastrointest Liver Physiol 311:G1047–G1055
Gladman MA, Aziz Q, Scott SM et al (2009) Rectal hyposensitivity: pathophysiological mechanisms. Neurogastroenterol Motil 21:508–516 e4-5
Chan CLH, Scott SM, Birch MJ et al (2003) Rectal heat thresholds: a novel test of the sensory afferent pathway. Dis Colon Rectum 46:590–595
Author information
Authors and Affiliations
Contributions
DC, AG, and TN designed the research study and wrote the paper, and DC, TN, CC, MP, TM, HR, FLB, LAM, HC, and AG contributed to the editing of the manuscript. All authors approved the final version of the article, including the authorship list.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guarantor of article Professor Gerard Amarenco
Rights and permissions
About this article
Cite this article
Desprez, C., Turmel, N., Chesnel, C. et al. Comparison of clinical and paraclinical characteristics of patients with urge, mixed, and passive fecal incontinence: a systematic literature review. Int J Colorectal Dis 36, 633–644 (2021). https://doi.org/10.1007/s00384-020-03803-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03803-8