Abstract
Purpose
Noninvasive markers for predicting endoscopic remission (ER) in patients with ulcerative colitis (UC) who are in clinical remission (CR) are important for the determination of appropriate treatment modality. C-reactive protein (CRP) is a surrogate marker for assessing disease activity, albeit with a low sensitivity and specificity when the cut-off value is 0.3 or 0.5 mg/dL, which is usually considered normal. The CRP test has been improved, and even fine values within the normal range can be measured. The aim of this study was to determine the appropriate cut-off value of CRP below 0.3 mg/dL for the prediction of ER in UC patients with CR.
Methods
A total of 132 patients who underwent endoscopic evaluation during CR were retrospectively reviewed. Clinical and endoscopic activity was measured using a simple clinical colitis activity index (SCCAI) and Mayo endoscopic subscore (MES). ER was defined as MES 0 or 1.
Results
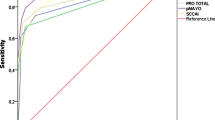
In UC patients in CR, the CRP level was significantly lower in ER (0.05, 0.03–2.57) vs. non-ER (0.14, 0.03–2.81) (p < 0.001). The CRP value predicted ER [area under the curve (AUC = 0.710)] with a sensitivity of 71.4% and a specificity of 71.7% at a cut-off value of 0.09 mg/dL. In contrast, the value of normal CRP (< 0.3 mg/dL) did not show sufficient predictive value (sensitivity, 27.3%; and specificity, 90.9%).
Conclusions
In UC patients in CR, it may be helpful to lower the CRP cut-off value that predict ER other than 0.3 mg/dL, which is usually considered normal.



Similar content being viewed by others
References
Ordas I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ (2012) Ulcerative colitis. Lancet 380:1606–1619
Choi CH, Jung SA, Lee BI, Lee KM, Kim JS, Han DS, I. B. D. Study Group of the Korean Association of the Study of Intestinal Diseases (2009) Diagnostic guideline of ulcerative colitis. Korean J Gastroenterol 53:145–160
Gross V, Andus T, Caesar I, Roth M, Scholmerich J (1992) Evidence for continuous stimulation of interleukin-6 production in Crohn’s disease. Gastroenterology 102:514–519
D'Haens G, Sandborn WJ, Feagan BG, Geboes K, Hanauer SB, Irvine EJ, Lemann M, Marteau P, Rutgeerts P, Scholmerich J, Sutherland LR (2007) A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology 132:763–786
Peyrin-Biroulet L, Sandborn W, Sands BE, Reinisch W, Bemelman W, Bryant RV, D'Haens G, Dotan I, Dubinsky M, Feagan B, Fiorino G, Gearry R, Krishnareddy S, Lakatos PL, Loftus EV Jr, Marteau P, Munkholm P, Murdoch TB, Ordas I, Panaccione R, Riddell RH, Ruel J, Rubin DT, Samaan M, Siegel CA, Silverberg MS, Stoker J, Schreiber S, Travis S, Van Assche G, Danese S, Panes J, Bouguen G, O'Donnell S, Pariente B, Winer S, Hanauer S, Colombel JF (2015) Selecting therapeutic targets in inflammatory bowel disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol 110:1324–1338
Yoon JG, Choi MJ, Yoon JW, Noh JY, Song JY, Cheong HJ, Kim WJ (2017) Seroprevalence and disease burden of acute hepatitis A in adult population in South Korea. PLoS One 12:e0186257
Neurath MF, Travis SP (2012) Mucosal healing in inflammatory bowel diseases: a systematic review. Gut 61:1619–1635
Parragi L, Fournier N, Zeitz J, Scharl M, Greuter T, Schreiner P, Misselwitz B, Safroneeva E, Schoepfer AM, Vavricka SR, Rogler G, Biedermann L, Swiss I. B. D. Cohort Study Group (2018) Colectomy rates in ulcerative colitis are low and decreasing: 10-year follow-up data from the Swiss IBD cohort study. J Crohns Colitis 12:811–818
Narang V, Kaur R, Garg B, Mahajan R, Midha V, Sood N, Sood A (2018) Association of endoscopic and histological remission with clinical course in patients of ulcerative colitis. Intest Res 16:55–61
Castaño-Milla C, Chaparro M, Gisbert JP (2014) Systematic review with meta-analysis: the declining risk of colorectal cancer in ulcerative colitis. Aliment Pharmacol Ther 39:645–659
Yamaguchi S, Takeuchi Y, Arai K, Fukuda K, Kuroki Y, Asonuma K, Takahashi H, Saruta M, Yoshida H (2016) Fecal calprotectin is a clinically relevant biomarker of mucosal healing in patients with quiescent ulcerative colitis. J Gastroenterol Hepatol 31:93–98
Navaneethan U, Parasa S, Venkatesh PG, Trikudanathan G, Shen B (2011) Prevalence and risk factors for colonic perforation during colonoscopy in hospitalized inflammatory bowel disease patients. J Crohns Colitis 5:189–195
Schoepfer AM, Beglinger C, Straumann A, Trummler M, Renzulli P, Seibold F (2009) Ulcerative colitis: correlation of the Rachmilewitz endoscopic activity index with fecal calprotectin, clinical activity, C-reactive protein, and blood leukocytes. Inflamm Bowel Dis 15:1851–1858
Wei SC (2016) Could fecal calprotectin enter mainstream use for diagnosing and monitoring inflammatory bowel disease? Intest Res 14:293–294
Lopez RN, Leach ST, Lemberg DA, Duvoisin G, Gearry RB, Day AS (2017) Fecal biomarkers in inflammatory bowel disease. J Gastroenterol Hepatol 32:577–582
Zittan E, Kelly OB, Kirsch R, Milgrom R, Burns J, Nguyen GC, Croitoru K, Van Assche G, Silverberg MS, Steinhart AH (2016) Low fecal calprotectin correlates with histological remission and mucosal healing in ulcerative colitis and colonic Crohn;s disease. Inflamm Bowel Dis 22:623–630
Kim DJ, Jeoun YM, Lee DW, Koo JS, Lee SW (2018) Usefulness of fecal immunochemical test and fecal calprotectin for detection of active ulcerative colitis. Intest Res 16:563–570
Lasson A, Stotzer PO, Ohman L, Isaksson S, Sapnara M, Strid H (2015) The intra-individual variability of faecal calprotectin: a prospective study in patients with active ulcerative colitis. J Crohns Colitis 9:26–32
Wei SC, Tung CC, Weng MT, Wong JM (2018) Experience of patients with inflammatory bowel disease in using a home fecal calprotectin test as an objective reported outcome for self-monitoring. Intest Res 16:546–553
Vermeire S, Van Assche G, Rutgeerts P (2006) Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut 55:426–431
Langhorst J, Boone J, Lauche R, Rueffer A, Dobos G (2016) Faecal lactoferrin, calprotectin, PMN-elastase, CRP, and white blood cell count as indicators for mucosal healing and clinical course of disease in patients with mild to moderate ulcerative colitis: post hoc analysis of a prospective clinical trial. J Crohns Colitis 10:786–794
Zilberman L, Maharshak N, Arbel Y, Rogowski O, Rozenblat M, Shapira I, Berliner S, Arber N, Dotan I (2006) Correlated expression of high-sensitivity C-reactive protein in relation to disease activity in inflammatory bowel disease: lack of differences between Crohn’s disease and ulcerative colitis. Digestion 73:205–209
Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, Burisch J, Gecse KB, Hart AL, Hindryckx P, Langner C, Limdi JK, Pellino G, Zagorowicz E, Raine T, Harbord M, Rieder F, European Crohn’s Colitis Organisation (2017) Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis 11:649–670
Tysk C, Järnerot G (1992) Ulcerative proctocolitis in Örebro, Sweden: a retrospective epidemiologic study, 1963–1987. Saudi J Gastroenterol 27:945–950
Yang SK, Hong WS, Min YI, Kim HY, Yoo JY, Rhee PL, Rhee JC, Chang DK, Song IS, Jung SA, Park EB, Yoo HM, Lee DK, Kim YK (2000) Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol 15:1037–1042
Walmsley RS, Ayres RC, Pounder RE, Allan RN (1998) A simple clinical colitis activity index. Gut 43:29–32
Sandborn W, Reinisch W, Rachmilewitz D, Hanauer S, Lichtenstein G, de Villiers W, Olson A, Johanns J, Travers S, Colombel J (2005) Infliximab induction and maintenance therapy for ulcerative colitis: the Act 2 trial. Z Gastroenterol 43:V6
Schroeder KW, Tremaine WJ, Ilstrup DM (1987) Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med 317:1625–1629
Frøslie KF, Jahnsen J, Moum BA, Vatn MH, Group I (2007) Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology 133:412–422
Velayos FS, Terdiman JP, Walsh JM (2005) Effect of 5-aminosalicylate use on colorectal cancer and dysplasia risk: a systematic review and metaanalysis of observational studies. Am J Gastroenterol 100:1345–1353
Tang J, Sharif O, Pai C, Silverman AL (2010) Mesalamine protects against colorectal cancer in inflammatory bowel disease. Dig Dis Sci 55:1696–1703
Meucci G, Fasoli R, Saibeni S, Valpiani D, Gullotta R, Colombo E, D’Inca R, Terpin M, Lombardi G, Ig IBD (2012) Prognostic significance of endoscopic remission in patients with active ulcerative colitis treated with oral and topical mesalazine: a prospective, multicenter study. Inflamm Bowel Dis 18:1006–1010
Bitton A, Peppercorn MA, Antonioli DA, Niles JL, Shah S, Bousvaros A, Ransil B, Wild G, Cohen A, Edwardes MDD (2001) Clinical, biological, and histologic parameters as predictors of relapse in ulcerative colitis. Gastroenterology 120:13–20
Linskens RK, van Bodegraven AA, Schoorl M, Tuynman HA, Bartels P (2001) Predictive value of inflammatory and coagulation parameters in the course of severe ulcerative colitis. Dig Dis Sci 46:644–648
Fagan EA, Dyck RF, Maton PN, Hodgson HJ, Chadwick VS, Petrie A, Pepys MB (1982) Serum levels of C-reactive protein in Crohn’s disease and ulcerative colitis. Eur J Clin Investig 12:351–359
Pepys MB, Druguet M, Klass HJ, Dash AC, Mirjah DD, Petrie A (1977) Immunological studies in inflammatory bowel disease. CIBA Found Symp 46:283–304
Karoui S, Laz S, Serghini M, Bibani N, Boubaker J, Filali A (2011) Correlation of C-reactive protein with clinical and endoscopic activity in patients with ulcerative colitis. Dig Dis Sci 56:1801–1805
Hassan EA, Ramadan HK, Ismael AA, Mohamed KF, El-Attar MM, Alhelali I (2017) Noninvasive biomarkers as surrogate predictors of clinical and endoscopic remission after infliximab induction in patients with refractory ulcerative colitis. Saudi J Gastroenterol 23:238–245
Rodgers AD, Cummins AG (2007) CRP correlates with clinical score in ulcerative colitis but not in Crohn’s disease. Dig Dis Sci 52:2063–2068
Hart L, Chavannes M, Kherad O, Maedler C, Mourad N, Marcus V, Afif W, Bitton A, Lakatos PL, Brassard P, Bessissow T (2020) Faecal calprotectin predicts endoscopic and histological activity in clinically quiescent ulcerative colitis. J Crohns Colitis 14:46–52
Nakov R, Velikova T, Nakov V, Gerova V, Tankova L (2019) Trefoil factor 3 is highly predictive of complete mucosal healing independently and in combination with C-reactive protein in patients with ulcerative colitis. J Gastrointestin Liver Dis 28:169–174
Yoshimura K, Saku A, Karayama M, Inui N, Sugimura H, Suda T (2020) Leucine-rich α2-glycoprotein as a potential biomarker for immune-related colitis after anti–PD-L1 therapy: a report of a case series. Clin Lung Cancer. https://doi.org/10.1016/j.cllc.2020.04.005
Oikonomou K, Kapsoritakis A, Theodoridou C, Karangelis D, Germenis A, Stefanidis I, Potamianos S (2012) Neutrophil gelatinase-associated lipocalin (NGAL) in inflammatory bowel disease: association with pathophysiology of inflammation, established markers, and disease activity. J Gastroenterol 47:519–530
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant awarded by the Korean government (MSIP) (no. NRF-2017R1A2B4006767).
Author information
Authors and Affiliations
Contributions
J Shin made substantial contribution to the conception and design, data acquisition, analysis, or interpretation and drafted the initial manuscripts, and reviewed and revised the final manuscript. Sung Min Kong and Gyeol Seong contributed to the conception and design, data acquisition, analysis, and interpretation. YH Kim was responsible for the conception and design of the study, data acquisition, analysis and interpretation, as well as drafting of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 120 kb)
Rights and permissions
About this article
Cite this article
Shin, J., Kong, S.M., Seong, G. et al. What is the appropriate cut-off value of CRP to predict endoscopic remission in patients with ulcerative colitis in clinical remission?. Int J Colorectal Dis 35, 2249–2255 (2020). https://doi.org/10.1007/s00384-020-03705-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03705-9