Abstract
Purpose
Treatment of lateral lymph node metastasis in rectal cancer is still under debate. While these nodes are routinely resected by Japanese teams, neoadjuvant radiochemotherapy alone is performed in Western countries. We aimed to systematically report the current literature assessing the overall and disease-free survivals of patients with rectal cancer treated with total mesorectal resection (TME) with or without lateral lymph node dissection (LLND).
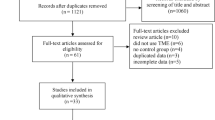
Methods
MEDLINE/Pubmed, Embase, Cochrane, and Web of Science were searched from database implementation until 19 January 2019. Studies reporting overall survival or recurrence-free survival in patients with LLND for rectal cancer were included. We excluded studies including patients with recurrent rectal cancer, multivisceral resection, and/or without control group (patients with rectal surgery without LLND).
Results
Eleven studies were included, accounting for a total of 4159 patients. Overall survival ranged between 55.6 and 92.6% for TME with LLND versus 49.2 and 90.2% for TME alone, with one study reporting statistically significant benefit of LLND. Recurrence-free survival ranged between 58.3 and 74.1% for TME with LLND versus 39.5 and 76.5% for TME alone. Two studies showed statistically significant differences between the two strategies, one randomized controlled trial showed improved recurrence-free survival in TME alone group (74.5% versus 74.1% with LLND at 5 years) and one observational retrospective study reported increased recurrence-free survival with more extensive resection (65.4% versus 39.5% without LLND, at 5 years).
Conclusion
Benefits of LLND are not clear and further randomized controlled trials should be performed to determine which strategy would allow improving survival in rectal cancer patients.
Trial registration
The study protocol was registered in PROSPERO prior to study screening (CRD42019123181) and published in September 2019.

Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin. 65(2):87–108
Schmoll HJ, Van Cutsem E, Stein A, Valentini V, Glimelius B, Haustermans K et al (2012) ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol. 23(10):2479–2516
Herold A, Lehur P-A, Matzel K, O’Connel R (2017) Coloproctology, European Manual of Medicine, 2nd edn. Springer
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin. 69(1):7–34
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet Lond Engl. 1(8496):1479–1482
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken J, Leer JW, van de Velde C, Dutch Colorectal Cancer Group (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 345(9):638–646
Martling A, Holm T, Johansson H, Rutqvist LE, Cedermark B (2001) Stockholm Colorectal Cancer Study Group. The Stockholm II trial on preoperative radiotherapy in rectal carcinoma: long-term follow-up of a population-based study. Cancer. 92(4):896–902
Kusters M, van de Velde CJH, Beets-Tan RGH, Akasu T, Fujita S, Fujida S et al (2009) Patterns of local recurrence in rectal cancer: a single-center experience. Ann Surg Oncol. 16(2):289–296
Takahashi T, Ueno M, Azekura K, Ohta H (2000) Lateral node dissection and total mesorectal excision for rectal cancer. Dis Colon Rectum. 43(10 Suppl):S59–S68
Wang Z, Loh KY, Tan K-Y, Woo EC-H (2012) The role of lateral lymph node dissection in the management of lower rectal cancer. Langenbecks Arch Surg. 397(3):353–361
Shimoyama M, Yamazaki T, Suda T, Hatakeyama K (2003) Prognostic significance of lateral lymph node micrometastases in lower rectal cancer: an immunohistochemical study with CAM5.2. Dis Colon Rectum. 46(3):333–339
Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y et al (2018) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 23(1):1–34
Weiser MR (2018) AJCC 8th Edition: colorectal cancer. Ann Surg Oncol. 25(6):1454–1455
van de Velde CJH, Boelens PG, Borras JM, Coebergh J-W, Cervantes A, Blomqvist L et al (2014) EURECCA colorectal: multidisciplinary management: European consensus conference colon & rectum. Eur J Cancer Oxf Engl 1990 50(1):1.e1–1.e34
Kim TH, Jeong S-Y, Choi DH, Kim DY, Jung KH, Moon SH, Chang HJ, Lim SB, Choi HS, Park JG (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol. 15(3):729–737
Ogura A, Akiyoshi T, Nagasaki T, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Ueno M, Kuroyanagi H (2017) Feasibility of laparoscopic total mesorectal excision with extended lateral pelvic lymph node dissection for advanced lower rectal cancer after preoperative chemoradiotherapy. World J Surg. 41(3):868–875
Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls RJ, Tekkis P (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol. 10(11):1053–1062
Watanabe T, Tsurita G, Muto T, Sawada T, Sunouchi K, Higuchi Y, Komuro Y, Kanazawa T, Iijima T, Miyaki M, Nagawa H (2002) Extended lymphadenectomy and preoperative radiotherapy for lower rectal cancers. Surgery. 132(1):27–33
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Meyer J, Christou N, Combescure C, Buchs N, Ris F (2019) Does lateral lymph node dissection for low rectal cancer improve overall survival? Protocol for a systematic review and meta-analysis. Int J Surg Protoc. 17:1–2
Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Bandou H, Katsumata K, Murata K, Akagi Y, Takiguchi N, Saida Y, Nakamura K, Fukuda H, Akasu T, Moriya Y, Colorectal Cancer Study Group of Japan Clinical Oncology Group (2017) Mesorectal excision with or without lateral nymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 266(2):201–207
Nagawa H, Muto T, Sunouchi K, Higuchi Y, Tsurita G, Watanabe T, Sawada T (2001) Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum. 44(9):1274–1280
Havenga K, Enker WE, Norstein J, Moriya Y, Heald RJ, van Houwelingen HC et al (1999) Improved survival and local control after total mesorectal excision or D3 lymphadenectomy in the treatment of primary rectal cancer: an international analysis of 1411 patients. Eur J Surg Oncol. 25(4):368–374
Dong X-S, Xu H-T, Yu Z-W, Liu M, Cu B-B, Zhao P et al (2003) Effect of extended radical resection for rectal cancer. World J Gastroenterol. 9(5):970–973
Hasdemir O, Cöl C, Yalçin E, Tunç G, Bilgen K, Kuçukpinar T (2005) Local recurrence and survival rates after extended systematic lymph-node dissection for surgical treatment of rectal cancer. Hepatogastroenterology. 52(62):455–459
Shiozawa M, Akaike M, Yamada R, Godai T, Yamamoto N, Saito H et al (2007) Lateral lymph node dissection for lower rectal cancer. Hepatogastroenterology. 54(76):1066–1070
Kobayashi H, Mochizuki H, Kato T, Mori T, Kameoka S, Shirouzu K, Sugihara K (2009r) Outcomes of surgery alone for lower rectal cancer with and without pelvic sidewall dissection. Dis Colon Rectum. 52(4):567–576
Akiyoshi T, Ueno M, Matsueda K, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Unno T, Kano A, Kuroyanagi H, Oya M, Yamaguchi T, Watanabe T, Muto T (2014) Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 21(1):189–196
Kim HJ, Choi G-S, Park JS, Park SY, Cho SH, Lee SJ, Kang BW, Kim JG (2017) Optimal treatment strategies for clinically suspicious lateral pelvic lymph node metastasis in rectal cancer. Oncotarget. 8(59):100724–100733
Matsuda T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2018) Outcomes and prognostic factors of selective lateral pelvic lymph node dissection with preoperative chemoradiotherapy for locally advanced rectal cancer. Int J Colorectal Dis. 33(4):367–374
Kinugasa T, Akagi Y, Shirouzu K (2014) Benefit of lateral lymph node dissection for rectal cancer: long-term analysis of 944 cases undergoing surgery at a single center (1975-2004). Anticancer Res. 34(8):4633–4639
Oki E, Shimokawa M, Ando K, Murata A, Takahashi T, Maeda K, Kusumoto T, Munemoto Y, Nakanishi R, Nakashima Y, Saeki H, Maehara Y (2019) Effect of lateral lymph node dissection for mid and low rectal cancer: an ad-hoc analysis of the ACTS-RC (JFMC35-C1) randomized clinical trial. Surgery. 165(3):586–592
Ozawa H, Kotake K, Hosaka M, Hirata A, Sugihara K (2016) Impact of lateral pelvic lymph node dissection on the survival of patients with T3 and T4 low rectal cancer. World J Surg. 40(6):1492–1499
Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T (2006) Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 49(11):1663–1672
Cheng H, Deng Z, Wang Z, Zhang W, Su J (2011) Lateral lymph node dissection with radical surgery versus single radical surgery for rectal cancer: a meta-analysis. Asian Pac J Cancer Prev APJCP. 12(10):2517–2521
Acknowledgments
The authors thank Christophe Combescure (Division of Epidemiology, University Hospitals of Geneva) for his contribution to data acquisition and interpretation.
Author information
Authors and Affiliations
Contributions
GL, JM, and NC conceived and designed the study. GL, JM, and NC acquired the data. GL, JM, NC, SP, ER, CT, NB, and FR interpreted the data. GL, JM, NC, SP, ER, CT, NB, and FR contributed to the writing of the manuscript and to its critical revision. GL, JM, NC, SP, ER, CT, NB, and FR approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
Not applicable
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 38 kb)
Rights and permissions
About this article
Cite this article
Longchamp, G., Meyer, J., Christou, N. et al. Total mesorectal excision with and without lateral lymph node dissection: a systematic review of the literature. Int J Colorectal Dis 35, 1183–1192 (2020). https://doi.org/10.1007/s00384-020-03623-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03623-w