Abstract
Purposes
Lateral pelvic lymph node (LPLN) dissection represents a technically challenging procedure with a high potential risk of surgical morbidity. The purpose of this study was to compare the technical feasibility, safety, and oncological efficacy of laparoscopic LPLN dissection (LPLD) following total mesorectal excision (TME) with open LPLD for locally advanced low rectal cancer (LALRC).
Methods
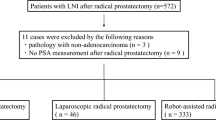
Between January 2010 and December 2016, consecutive patients with LALRC and swollen LPLNs who underwent laparoscopic or open TME with LPLD at our institution were enrolled in this retrospective observational study. Data regarding patient demographics, perioperative characteristics, and oncological outcomes were analyzed and compared.
Results
A total of 64 patients met the inclusion criteria. Thirty-four patients underwent open procedure, and 30 underwent laparoscopic procedure. The mean blood loss volume was significantly less in the laparoscopic group than in the open group (165 vs. 422 mL; P = 0.012). The mean operative time was not significantly different between the laparoscopic and the open groups (354 ± 91 vs. 315 ± 78 min; P = 0.522). The overall postoperative complication rates were 30.0% and 35.3% for the laparoscopic and open groups (P = 0.428), respectively. Postoperative urinary retention was significantly less in the laparoscopic group than in the open group (14.7 vs. 0%; P = 0.036).The duration of postoperative hospital stay was significantly shorter in the laparoscopic group (8.5 ± 3.8 vs. 13.6 ± 6.5 days; P = 0.025). The numbers of harvested lymph nodes and positive resection margin rates showed no significant differences. Pathological LPLN metastases were confirmed in 10 patients (29.4%) in the open group and 11 (36.7%) in the laparoscopic group (P = 0.537). The median follow-up duration was 41.5 months (range 3–98). The laparoscopic and open groups also showed a similar 3-year overall survival rate (88.2% vs. 85.3%; P = 0.577), relapse-free survival rate (73.3% vs. 67.6%; P = 0.889), and local recurrence rate (3.3 vs. 5.9%; P = 0.653).
Conclusions
Laparoscopic TME with LPLD is technically feasible and safe in selected patients with LALRC and is associated with similar oncological outcomes as open approach.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132
Ueno M, Oya M, Azekura K, Yamaguchi T, Muto T (2005) Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg 92:756–763
Yano H, Moran BJ (2008) The incidence of lateral pelvic side-wall nodal involvement in low rectal cancer may be similar in Japan and the West. Br J Surg 95:33–49
Kusters M, Beets GL, van de Velde CJ, Beets-Tan RG, Marijnen CA, Rutten HJ, Putter H, Moriya Y (2009) A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg 249:229–235
Kim TH, Jeong SY, Choi DH, Kim DY, Jung KH, Moon SH, Chang HJ, Lim SB, Choi HS, Park JG (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 15:729–737
Akiyoshi T, Ueno M, Matsueda K, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Unno T, Kano A, Kuroyanagi H, Oya M, Yamaguchi T, Watanabe T, Muto T (2014) Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol 21:189–196
Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls RJ, Tekkis P (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a metaanalysis. Lancet Oncol 10:1053–1062
Kim TG, Park W, Choi DH, Park HC, Kim SH, Cho YB, Yun SH, Kim HC, Lee WY, Lee J, Park JO, Park YS, Lim HY, Kang WK, Chun HK (2014) Factors associated with lateral pelvic recurrence after curative resection following neoadjuvant chemoradiotherapy in rectal cancer patients. Int J Color Dis 29:193–200
Kim MJ, Kim TH, Kim DY, Kim SY, Baek JY, Chang HJ, Park SC, Park JW, Oh JH (2015) Can chemoradiation allow for omission of lateral pelvic node dissection for locally advanced rectal cancer? J Surg Oncol 111:459–464
Akiyoshi T, Watanabe T, Miyata S, Kotake K, Muto T, Sugihara K, Japanese Society for Cancer of the Colon and Rectum (2012) Results of a Japanese nationwide multi-institutional study on lateral pelvic lymph node metastasis in low rectal cancer: is it regional or distant disease? Ann Surg 255:1129–1134
Watanabe T, Muro K, Ajioka Y et al (2018) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 23:1–34
Van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of randomised, phase 3 trial. Lancet Oncol 14:210–218
Uyama I, Sugioka A, Matsui H, Fujita J, Komori Y, Hanai T, Hasumi A (2001) Laparoscopic lateral node dissection with autonomic nerve preservation for advanced lower rectal cancer. J Am Coll Surg 193:579–584
Yamaguchi T, Konishi T, Kinugasa Y, Yamamoto S, Akiyoshi T, Okamura R, Ito M, Nishimura Y, Shiozawa M, Yamaguchi S, Hida K, Sakai Y, Watanabe M (2017) Laparoscopic versus open lateral lymph node dissection for locally advanced low rectal cancer: a subgroup analysis of a large multicenter cohort study in Japan. Dis Colon Rectum 60:954–964
Nagayoshi K, Ueki T, Manabe T, Moriyama T, Yanai K, Oda Y, Tanaka M (2016) Laparoscopic lateral pelvic lymph node dissection is achievable and offers advantages as a minimally invasive surgery over the open approach. Surg Endosc 30:1938–1947
Liang JT, Lai HS, Lee PH (2007) Laparoscopic pelvic autonomic nerve-preserving surgery for patients with lower rectal cancer after chemoradiation therapy. Ann Surg Oncol 14:1285–1287
Matsumoto A, Arita K (2017) Technique of laparoscopic lateral pelvic lymph node dissection based on vesicohypogastric fascia and ureterohypogastric nerve fascia for advanced low rectal cancer. Surg Endosc 31:945–948
Furuhata T, Okita K, Nishidate T, Ito T, Yamaguchi H, Ueki T, Akizuki E, Meguro M, Ogawa T, Kukita K, Kimura Y, Mizuguchi T, Hirata K (2015) Clinical feasibility of laparoscopic lateral pelvic lymph node dissection following total mesorectal excision for advanced rectal cancer. Surg Today 45:310–314
Amin MB, Greene FL, Edge S (2017) AJCC cancer staging manual, 8th edn. Springer, New York, pp 252–274
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Bandou H, Katsumata K, Murata K, Akagi Y, Takiguchi N, Saida Y, Nakamura K, Fukuda H, Akasu T, Moriya Y (2017) Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg 266:201–207
Ogura A, Konishi T, Cunningham C, Garcia-Aguilar J, Iversen H, Toda S, Lee IK, Lee HX, Uehara K, Lee P, Putter H, van de Velde CJH, Beets GL, Rutten HJT, Kusters M (2019) Neoadjuvant (chemo) radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low cT3/4 rectal cancer. J Clin Oncol 37:33–43
Kim HJ, Choi GS, Park JS, Park SY, Lee HJ, Woo IT, Park IK (2018) Selective lateral pelvic lymph node dissection: a comparative study of the robotic versus laparoscopic approach. Surg Endosc 32:2466–2473
Ogura A, Akiyoshi T, Nagasaki T, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Ueno M, Kuroyanagi H (2017) Feasibility of laparoscopic total mesorectal excision with extended lateral pelvic lymph node dissection for advanced lower rectal cancer after preoperative chemoradiotherapy. World J Surg 41:868–875
Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Akasu T, Moriya Y (2018) Urinary dysfunction after rectal cancer surgery: results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212). Eur J Surg Oncol 44:463–468
Funding
This research was supported by a grant from the National Medical Science Development Programs, The National Health Commission of China (W2015JZC01).
Author information
Authors and Affiliations
Contributions
Fanghai Han and Han Bin Yang contributed to the study conception and design; Bin Yang, Jing Huang, and Han Gao contributed to the acquisition of data; Shengning Zhou, Jianan Tan, and Guangyu Zhong contributed to the analysis and interpretation of data; Bin Yang, Fanghai Han, Jing Huang, and Shengning Zhou contributed to the writing of the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and the institutional review board of Sun Yat-sen Memorial Hospital of Sun Yat-sen University approved the project.
Consent to participate
Written informed consent was obtained from individual or guardian participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, B., Huang, J., Zhou, S. et al. Laparoscopic versus open selective lateral pelvic lymph node dissection following total mesorectal excision for locally advanced low rectal cancer. Int J Colorectal Dis 35, 1301–1309 (2020). https://doi.org/10.1007/s00384-020-03609-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03609-8