Abstract
Purpose
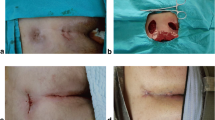
Pilonidal sinus disease (PD) is a common acquired disease, responsible for discomfort and time off work. There is currently no consensus on the best surgical therapy. We aimed at comparing conservative sinusectomy (S) to excision and paramedian primary closure (PC).
Methods
This is a randomized controlled trial compatible with the CONSORT statement standards. We included all patients with chronic PD between 2012 and 2017. We excluded patients with acute abscesses, recurrent PD after surgery with a curative intent and patients needing complex reconstructions with rotation flaps. Patients with chronic symptomatic PD were randomized to S or PC. Primary end-point was the rate of patients healed at 3 weeks, secondary outcomes were total healing time, pain, time off work, patient satisfaction and recurrence at 1 year. Patients were seen at a wound clinic until healed and contacted at 3, 6, and 12 months for follow-up.
Results
After inclusion of 58 patients the study was stopped prematurely due to discrepancy between expected and observed outcomes. Only 4/30 (13.3%) patients in the S group had healed completely at 3 weeks compared with 14/28 (50%) in the PC group (p = 0.01). Median time to complete healing was 54 (23–328) days in the S group compared to 34 (13–141) in the PC group (p = 0.025). Number of outpatient visits, time off work, analgesia requirement, and recurrence rates at 12 months 4 (16%) in the S group and 3 (11.1%) in the PC group (p = 0.548) were similar.
Conclusions
PC leads to faster healing compared to S, with similar healthcare burden.
Trial Registration
The study was approved by the local ethics committee and registered in www.clinicaltrials.gov (REF: NCT03271996).
The study was carried out at the Regional Hospital of Lugano, Switzerland



Similar content being viewed by others
Change history
26 May 2020
The original version of this article, unfortunately, contained an error. The given names and family names of the authors were interchanged and are now presented correctly. The original article has been corrected.]
References
McCallum I, King PM, Bruce J (2007) Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev (4):CD006213
Al-Khamis A, McCallum I, King PM, Bruce J (2010) Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev (1):CD006213
Enriquez-Navascues JM, Emparanza JI, Alkorta M, Placer C (2014) Meta-analysis of randomized controlled trials comparing different techniques with primary closure for chronic pilonidal sinus. Tech Coloproctol 18:863–872
Sakr M, Habib M, Shaheed AA (2006) Assessment of Karydakis technique as compared with midline closure for the management of chronic pilonidal sinus. J Pelvic Med Surg 12:201–206
Polat N, Albayrak D, Ibis AC, Altan A (2008) Comparison between Karydakis repair and primary closure for surgical treatment of sacrococcygeal pilonidal sinus. Medical Journal of Trakya University / Trakya Universitesi Tip Fakultesi Dergisi (TRAK UNIV TIP FAK DE) 25:87–94
Ortiz HH, Marti J, Sitges A (1977) Pilonidal sinus. A claim for simple track incision. Dis Colon Rectum 20:325–328
Gupta PJ (2004) A randomized study between excision and marsupialization and radiofrequency sinus excision in sacrococcygeal pilonidal disease. Curr Surg 61:307–312
Mohamed HA, Kadry I, Adly S (2005) Comparison between three therapeutic modalities for non-complicated pilonidal sinus disease. Surgeon 3:73–77
Oncel N, Kurt M, Kement M, Colak E, Eser M, Uzun H (2002) Excision and marsupialization versus sinus excision for the treatment or limited chronic pilonidal disease: a prospective, randomized trial. Tech Coloproctol 6:165–169
Soll C, Dindo D, Steinemann D, Hauffe T, Clavien PA, Hahnloser D (2011) Sinusectomy for primary pilonidal sinus: less is more. Surgery. 5:996–1001
Gips M, Melki Y, Salem L, Weil R, Sulkes J (2008) Minimal surgery for pilonidal disease using trephines: description of a new technique and long-term outcomes in 1,358 patients. Dis Colon Rectum 11:1656–1662
Emile SH, Elfeki H, Shalaby M, Sakr A, Giaccaglia V, Sileri P, Wexner SD (2018) Endoscopic pilonidal sinus treatment: a systematic review and meta-analysis. Surg Endosc 9:3754–3762
Nordon I, Senapati A, Cripps NP et al (2009) A prospective randomized controlled trial of simple Bascom’s technique versus Bascom’s cleft closure for the treatment of chronic pilonidal disease. Am J Surg 2:189–192
Stauffer VK, Luedi MM, Kauf P, Schmid M, Diekmann M, Wieferich K, Schnüriger B, Doll D (2018) Common surgical procedures in pilonidal sinus disease: a meta-analysis, merged data analysis, and comprehensive study on recurrence. Sci Rep 1:3058
Anderson J, Yip CO, Nagabhushan JS, Connelly SJ (2008) Day-Case Karydakis Flap for Pilonidal Sinus. Dis Colon Rectum 1:134–138
Ates M, Dirican A, Sarac M, Aslan A, Colak C (2011) Short and long-term results of the Karydakis flap versus the Limberg flap for treating pilonidal sinus disease: a prospective randomized study. Am J Surg 5:568–573
Bessa S (2013) Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the Management of Pilonidal Sinus Disease: a randomized controlled study. Dis Colon Rectum 56:491–498
Karaca T, Yoldaş O, Bilgin BÇ, Ozer S, Yoldaş S, Karaca NG (2012) Comparison of short-term results of modified Karydakis flap and modified Limberg flap for pilonidal sinus surgery. Int J Surg 10:601–606
Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G (2010) Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg 3:318–327
Arslan K, Said Kokcam S, Koksal H, Turan E, Atay A, Dogru O (2014) Which flap method should be preferred for the treatment of pilonidal sinus? A prospective randomized study. Tech Coloproctol 1:29–37
CDC SSI Guidelines: https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf
Sevinç B, Karahan Ö, Okuş A, Ay S, Aksoy N, Şimşek G (2016) Randomized prospective comparison of midline and off-midline closure techniques in pilonidal sinus surgery. Surgery. 3:749–754
Ersoy E, Devay AO, Aktimur R, Doganay B, Ozdoğan M, Gündoğdu RH (2009) Comparison of the short-term results after Limberg and Karydakis procedures for pilonidal disease: randomized prospective analysis of 100 patients. Color Dis 7:705–710
Arda IS, Güney LH, Sevmiş S, Hiçsönmez A (2005) High body mass index as a possible risk factor for pilonidal sinus disease in adolescents. World J Surg 4:469–471
Al-Khayat H, Al-Khayat H, Sadeq A, Groof A, Haider HH, Hayati H, Shamsah A, Zarka ZA, Al-Hajj H, Al-Momen A (2007) Risk factors for wound complication in pilonidal sinus procedures. J Am Coll Surg 3:439–444
Cubukçu A, Gönüllü NN, Paksoy M, Alponat A, Kuru M, Ozbay O (2000) The role of obesity on the recurrence of pilonidal sinus disease in patients, who were treated by excision and Limberg flap transposition. Int J Color Dis 3:173–175
Sakr M, El-Hammadi H, Moussa M, Arafa S, Rasheed M (2003) The effect of obesity on the results of Karydakis technique for the management of chronic pilonidal sinus. Int J Color Dis 1:36–39
Sievert H, Evers T, Matevossian E, Hoenemann C, Hoffmann S, Doll D (2013) The influence of lifestyle (smoking and body mass index) on wound healing and long-term recurrence rate in 534 primary pilonidal sinus patients. Int J Color Dis 28:1555–1562
Kayaalp C (2014) Do smoking and obesity really do not have any negative influence on wound healing after surgery of pilonidal disease? Int J Color Dis 29:1303–1304
Acknowledgments
We kindly thank Prof. Pietro Majno-Hürst for his critical review of the manuscript and Dr. Luca Fumagalli for the surgical technique illustrations.
Funding
The study was funded by the peer reviewed competitive fund ABREOC (Advisory Board for Research of the Ente Ospedaliero Cantonale).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The given names and family names of the authors were interchanged and are now presented correctly.
Article Summary
We randomized patients with chronic pilonidal sinus to sinusectomy or excision and paramedian primary closure. The importance of this study is that it showed faster healing times in the paramedian primary closure group with no difference in recurrence rates or “healthcare burden”.
Rights and permissions
About this article
Cite this article
Popeskou, S.G., Pravini, B., Panteleimonitis, S. et al. Conservative Sinusectomy vs. excision and primary off-midline closure for pilonidal disease: a randomized controlled trial. Int J Colorectal Dis 35, 1193–1199 (2020). https://doi.org/10.1007/s00384-020-03551-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03551-9