Abstract
Purpose
This study aimed to clarify predictors and therapeutic significance of inguinal lymph node metastasis (ILNM) in patients with rectal cancer.
Methods
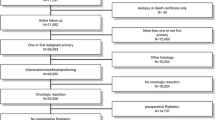
Patients with rectal adenocarcinoma invading the anal canal who underwent curative surgery between 2003 and 2019 were retrospectively reviewed. Synchronous and metachronous lymph node (LN) metastasis were collectively defined as final nodal metastasis (f-LNM). Factors associated with f-LNM were analyzed. Moreover, the “modified therapeutic value index,” defined by multiplication of the frequency of f-LNM by the 5-year overall survival rate for patients who received treatment for f-LNM, was calculated for each LN area.
Results
A total of 145 patients were enrolled (16 patients with f-ILNM). To predict f-ILNM, the cutoff of the inguinal lymph node (ILN) diameter of 8.5 mm gave an area under the curve of 0.889. Dentate line involvement (odds ratio 33.4) and ILN larger than the cutoff of 8 mm (odds ratio 11.9) were independently associated with f-ILNM. The modified therapeutic value indices of the inguinal, lateral pelvic, and mesorectal LNs in the entire population were 6.1, 8.2, and 20.3 points, respectively. In patients with dentate line invasion by cancer, the index of the ILN increased to 11.7 points. In patients with an ILN > 8 mm, the index further increased to 21.1 points.
Conclusion
Dentate line involvement and ILN > 8 mm predicted the development of ILNM in patients with rectal cancer invading the anal canal. Treatment of the ILN should be considered for patients with the above predictors given the significant therapeutic outcomes.



Similar content being viewed by others
References
Grinnell RS (1942) The lymphatic and venous spread of carcinoma of the rectum. Ann Surg 116(2):200–216. https://doi.org/10.1097/00000658-194208000-00005
Graham RA, Hohn DC (1990) Management of inguinal lymph node metastases from adenocarcinoma of the rectum. Dis Colon Rectum 33(3):212–216
Weiser MR (2018) AJCC 8th edition: colorectal cancer. Ann Surg Oncol 25(6):1454–1455. https://doi.org/10.1245/s10434-018-6462-1
Taylor N, Crane C, Skibber J, Feig B, Ellis L, Vauthey JN, Hamilton S, Cleary K, Dubrow R, Brown T, Wolff R, Hoff P, Sanfilippo N, Janjan N (2001) Elective groin irradiation is not indicated for patients with adenocarcinoma of the rectum extending to the anal canal. Int J Radiat Oncol Biol Phys 51(3):741–747
Hamano T, Homma Y, Otsuki Y, Shimizu S, Kobayashi H, Kobayashi Y (2010) Inguinal lymph node metastases are recognized with high frequency in rectal adenocarcinoma invading the dentate line. The histological features at the invasive front may predict inguinal lymph node metastasis. Color Dis 12(10 online):e200–e205. https://doi.org/10.1111/j.1463-1318.2009.02134.x
Adachi T, Hinoi T, Egi H, Ohdan H (2013) Surgical treatment for isolated inguinal lymph node metastasis in lower rectal adenocarcinoma patients improves outcome. Int J Color Dis 28(12):1675–1680. https://doi.org/10.1007/s00384-013-1746-1
Yeo SG, Lim HW, Kim DY, Kim TH, Kim SY, Baek JY, Chang HJ, Park JW, Oh JH (2014) Is elective inguinal radiotherapy necessary for locally advanced rectal adenocarcinoma invading anal canal? Radiat Oncol 9:296. https://doi.org/10.1186/s13014-014-0296-1
Wang R, Wu P, Shi D, Zheng H, Huang L, Gu W, Xu Y, Cai S, Cai G (2014) Risk factors of synchronous inguinal lymph nodes metastasis for lower rectal cancer involving the anal canal. PLoS One 9(11):e111770. https://doi.org/10.1371/journal.pone.0111770
NCCN Clinical Practice Guidelines in Oncology Version 3. 2019: Rectal cancer.
Zilli T, Betz M, Bieri S, Ris F, Roche B, Roth AD, Allal AS (2013) Elective inguinal node irradiation in early-stage T2N0 anal cancer: prognostic impact on locoregional control. Int J Radiat Oncol Biol Phys 87(1):60–66. https://doi.org/10.1016/j.ijrobp.2013.03.008
Tonouchi H, Ohmori Y, Kobayashi M, Konishi N, Tanaka K, Mohri Y, Mizutani H, Kusunoki M (2004) Operative morbidity associated with groin dissections. Surg Today 34(5):413–418. https://doi.org/10.1007/s00595-003-2738-5
Ishihara S, Kawai K, Tanaka T, Kiyomatsu T, Hata K, Nozawa H, Morikawa T, Watanabe T (2017) Oncological outcomes of lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Dis Colon Rectum 60(5):469–476. https://doi.org/10.1097/dcr.0000000000000752
Ueno H, Mochizuki H, Hashiguchi Y, Ishiguro M, Miyoshi M, Kajiwara Y, Sato T, Shimazaki H, Hase K (2007) Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg 245(1):80–87. https://doi.org/10.1097/01.sla.0000225359.72553.8c
Sasako M, McCulloch P, Kinoshita T, Maruyama K (1995) New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg 82(3):346–351
Ogawa S, Hida J, Ike H, Kinugasa T, Ota M, Shinto E, Itabashi M, Kameoka S, Sugihara K (2016) Selection of lymph node-positive cases based on perirectal and lateral pelvic lymph nodes using magnetic resonance imaging: study of the Japanese Society for Cancer of the Colon and Rectum. Ann Surg Oncol 23(4):1187–1194. https://doi.org/10.1245/s10434-015-5021-2
Ishibe A, Ota M, Watanabe J, Suwa Y, Suzuki S, Kanazawa A, Watanabe K, Ichikawa Y, Kunisaki C, Endo I (2016) Prediction of lateral pelvic lymph-node metastasis in low rectal cancer by magnetic resonance imaging. World J Surg 40(4):995–1001. https://doi.org/10.1007/s00268-015-3299-7
Langman G, Patel A, Bowley DM (2015) Size and distribution of lymph nodes in rectal cancer resection specimens. Dis Colon Rectum 58(4):406–414. https://doi.org/10.1097/dcr.0000000000000321
Shihab OC, Taylor F, Bees N, Blake H, Jeyadevan N, Bleehen R, Blomqvist L, Creagh M, George C, Guthrie A, Massouh H, Peppercorn D, Moran BJ, Heald RJ, Quirke P, Tekkis P, Brown G (2011) Relevance of magnetic resonance imaging-detected pelvic sidewall lymph node involvement in rectal cancer. Br J Surg 98(12):1798–1804. https://doi.org/10.1002/bjs.7662
Chand M, Heald RJ, Brown G (2013) The importance of not overstaging mesorectal lymph nodes seen on MRI. Color Dis 15(10):1201–1204. https://doi.org/10.1111/codi.12435
Ishihara S, Kawai K, Tanaka T, Kiyomatsu T, Hata K, Nozawa H, Morikawa T, Watanabe T (2018) Diagnostic value of FDG-PET/CT for lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Techniques Coloproctol 22(5):347–354. https://doi.org/10.1007/s10151-018-1779-0
Bae SU, Won KS, Song BI, Jeong WK, Baek SK, Kim HW (2018) Accuracy of F-18 FDG PET/CT with optimal cut-offs of maximum standardized uptake value according to size for diagnosis of regional lymph node metastasis in patients with rectal cancer. Cancer Imaging 18(1):32. https://doi.org/10.1186/s40644-018-0165-5
Grey AC, Carrington BM, Hulse PA, Swindell R, Yates W (2000) Magnetic resonance appearance of normal inguinal nodes. Clin Radiol 55(2):124–130. https://doi.org/10.1053/crad.1999.0330
Damin DC, Tolfo GC, Rosito MA, Spiro BL, Kliemann LM (2010) Sentinel lymph node in patients with rectal cancer invading the anal canal. Techniques Coloproctol 14(2):133–139. https://doi.org/10.1007/s10151-010-0582-3
Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Bandou H, Katsumata K, Murata K, Akagi Y, Takiguchi N, Saida Y, Nakamura K, Fukuda H, Akasu T, Moriya Y (2017) Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal Cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg 266(2):201–207. https://doi.org/10.1097/sla.0000000000002212
Oh HK, Kang SB, Lee SM, Lee SY, Ihn MH, Kim DW, Park JH, Kim YH, Lee KH, Kim JS, Kim JW, Kim JH, Chang TY, Park SC, Sohn DK, Oh JH, Park JW, Ryoo SB, Jeong SY, Park KJ (2014) Neoadjuvant chemoradiotherapy affects the indications for lateral pelvic node dissection in mid/low rectal cancer with clinically suspected lateral node involvement: a multicenter retrospective cohort study. Ann Surg Oncol 21(7):2280–2287. https://doi.org/10.1245/s10434-014-3559-z
Kim MJ, Chan Park S, Kim TH, Kim DY, Kim SY, Baek JY, Chang HJ, Park JW, Oh JH (2016) Is lateral pelvic node dissection necessary after preoperative chemoradiotherapy for rectal cancer patients with initially suspected lateral pelvic node? Surgery 160(2):366–376. https://doi.org/10.1016/j.surg.2016.04.006
Petrelli F, Trevisan F, Cabiddu M, Sgroi G, Bruschieri L, Rausa E, Ghidini M, Turati L (2019) Total neoadjuvant therapy in rectal cancer: a systematic review and meta-analysis of treatment outcomes. Ann Surg. https://doi.org/10.1097/SLA.0000000000003471
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rodel C, Cervantes A, Arnold D (2017) Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 28(suppl_4):iv22–iv40. https://doi.org/10.1093/annonc/mdx224
Funding
This research is supported by Grants-in-Aid for Scientific Research (C: grant number; 17K10620, C: grant number; 17K 10621, C: grant number; 17K10623, C: grant number; 18K07194, C: grant number; 19K09114, C: grant number; 19K09115) from Japan Society for the promotion of Science. This research is supported by the Project for Cancer Research and Therapeutic Evolution (P-CREATE), grant number: JP 19cm0106502 from the Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Contributions
H. Shiratori and H. Nozawa designed the study and wrote the initial draft of the manuscript, and K. Kawai, K. Hata, T. Tanaka, M. Kaneko, S. Emoto, H. Sonoda, and S. Ishihara revised it critically for important intellectual content. All the authors contributed to data collection, analysis, and interpretation of data and assisted in the preparation of the manuscript. All the authors agreed accountable for all aspects of the work and approved the final version to be published.
Corresponding author
Ethics declarations
This study was conducted following approval by the ethics committee of the University of Tokyo Hospital (No. 3252-(8)).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shiratori, H., Nozawa, H., Kawai, K. et al. Risk factors and therapeutic significance of inguinal lymph node metastasis in advanced lower rectal cancer. Int J Colorectal Dis 35, 655–664 (2020). https://doi.org/10.1007/s00384-020-03520-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03520-2